* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Summary of Factors that Regulate Cardiac Output
Management of acute coronary syndrome wikipedia , lookup
Heart failure wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Coronary artery disease wikipedia , lookup
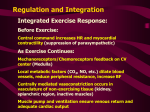
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Jatene procedure wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Electrocardiography wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
2 November 2011 Control of Cardiac Output Properties of Blood Vessels Announcements & Reminders Test 2 on Monday Photo-shoot Friday 1pm Biology Suite 1QQs & Moodle 1QQ # 24 for 8:30 1. What is the difference between a heart sound and a heart murmur? 2. What type of cell has “funny” Na+ channels and what is unusual about these channels? 3. In what situation might an ectopic pacemaker actually be beneficial? 1QQ # 24 for 9:30 1. How would heart rate be affected by an antagonist of beta adrenergic receptors? Explain your answer. 2. What type of cell has T-type Ca++ channels and what is the purpose of these channels in those cells? 3. Suppose your sinoatrial node pacemaker cells ceased working. Would your heart continue to beat, and if so, would it beat faster or slower than before? Explain. S1 So far, we’ve dealt with the factors that control Cardiac Output by changing heart rate. 3 CO = HR x SV 2 + sympathetic - parasympathetic 1 5L/min = 72 beat/min x 70 ml/beat 35L/min = ? beat/min x ? ml/beat S2 Figure 12.20 Stroke Volume Animation S3 Frank-Starling Law of the Heart Does not depend on hormones or nerves Assures that the heart adjusts its output based on VENOUS RETURN Ventricular Function Curve Ways to enhance Venous Return: 1) muscle contractions 2) “respiratory pump” 3) venoconstriction FS LoH = SV is proportional to EDV ↑VR→ ↑EDV → ↑SV S4 Length-tension “curve” for Cardiac muscle Fig. 09.21 High EDV Low EDV Overinflation of ventricles leads to less effective pumping S5 Overinflation of ventricles results in reduction in stroke volume Treatments? …..diuretics S6 NE from Symp postganglionics & EPI from Adrenal medulla Contractility Increase Ejection Fraction Note: cardiac myofibers NOT innervated by parasympathetic division S7 3 Effects of Sympathetic Stimulation 1: Increase rate of contraction 2: Increase peak tension 3: Decrease twitch duration Why should the contraction be shorter? S8 Summary: Control of Stroke Volume FS LoH • End diastolic volume (preload) • Contractility (strength of ventricular contraction due to adrenergic stimulation) • Pressure in arteries that must be overcome = Afterload Afterload is analogous to trying to pump more air into a tire that is already fully inflated (heart contracting to overcome diastolic pressure.) S9 High blood pressure increases the workload of the heart….. Cardiac hypertrophy….increase chance of irregular conduction of AP through heart Hypertrophic cardiomyopathy S 10 Figure 12.20 Animation S 11 Factors that control Cardiac Output by changing heart rate and stroke volume. Afterload (MAP) CO = HR x SV EDV (FSLoH) + sympathetic - parasympathetic contractility 5L/min = 72 beat/min x 70 ml/beat 35L/min = ? beat/min x ? ml/beat Summary of Factors that Regulate Cardiac Output S 12 Fig. 12.28 Even persons with heart transplants can adjust CO in the absence of innervation of heart. Notice: No Parasymp innervation of Cardiac Myofibers, Parasymp to Conducting Cells only. End of material for Test # 2 Begin material for Test # 3 S 13 Heart is pump that generates pressure gradient. Blood flows through vessels, which have resistance. Arterioles have greatest resistance and create “backpressure” in the arteries and aorta. Mean Arterial Pressure = diastolic +1/3(systolic – diastolic) = 70 + 1/3(120-70) = 70 + 17 = 87 mm Hg S 14 Mean Arterial Pressure = Cardiac Output x Total Peripheral Resistance MAP = CO x TPR MAP = (HR x SV) x TPR