* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Week 2 File - ACI Moodle
Survey
Document related concepts
Transcript
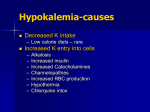
EMERGENCY MEDICINE Liverpool Hospital The Weekly Probe 3rd February 2014 Volume 17 Issue 2 Welcomes and Farewells- As the end of the term approaches there are new staff arriving and others moving to ?greener pastures. Thanks to all those moving on for all your hard work over the term, and for some of the regs, over the years. Thanks again. For the new staff, welcome. The place may seem a bit daunting at times but there is always someone to ask for advice and support. Rabies – occasionally we get visitors from overseas with recent potential exposure and non-travellers who may have been exposed to lyssavirus carried by bats. The info on this has been placed on the intranet site under “Clinical” then “medical” then "Infectious Diseases". Notify the Public Health Unit – they will also help organise the deliver and administration of the immunoglobulin and vaccine. Up-to-date – you may have tried to access Up-to-date unsuccessfully this week but the Hospital subscription is not being renewed- bugger! An option is Dynamed which is evidence based and more in point form. For access go to the Hospital web site then Libraries on the right then Liverpool – the link is on the right bottom of the screen. The advantage of this new service is that it is designed for point of care access with point form and you can get free access on you smart phone or ipad etc – go to Athens link on the left hand side http://www.swslhd.nsw.gov.au/liverpool/library/ then to the Athens registration form. Less detailed and to be honest it’s a bit of a step down from up-to-date. Urine microscopy- After discussions with micro over the last week, it has been pointed out that urine samples are assessed on a automated IRIS instrument. Apparently this is fast, accurate and reliable and we have substantially reduced the time to reporting of routine urine microscopy as a result. However they don’t report routinely on the presence or absence of bacteria. However if you clinically feel that this would change your management ring the lab and ask if this can be reported. Andi’s Trek – Andi Rauch has entered the Coastrek team challenge, a 50km walk to raise funds for The Fred Hollows Foundation, a charity which does a great job world-wide. Go to https://secure.coastrekfundraising.com.au/registrant/PersonalPage.aspx?eventid=43849&Registratio nID=672065 to help a great cause. THIS WEEK Alcoholic ketoacidosis Metabolic acidosis Ketone meter Next Week Joke / Quote of the Week The Week Ahead Alcoholic ketoacidosis: 54yo man with Hx of previous alcohol abuse presents with abdo pain post binge. No vomiting. Lipase 292 pH 7.1 Co2 24 , bicarb 9 BE -17 lactate 1 - EUC Na 132/ K 4.2 / Cl 98 /bicarb 9/ Urea 3.2 / Cr 71 BSL 6 What is it and how do we treat? Similar to other conditions in the ED our first priority is the ABCDEs, analgesia and supportive management. Looking at the various pathologies we need to treat precipitating factors and complications in this case the pancreatitis. However looking at the above VBG we note the pH of 7.1 and the CO2 of 24 which is consistent with a partially compensated metabolic acidosis. Metabolic Acidosis When you find a patient with an acidosis the first thing to do is calculate the anion gap so you can place the acidosis in a category of either normal anion gap & high anion gap acidosis. Anion gap = Na + K - (Cl + HCO3). Normal = 15 +/- 2,. The anion gap is due to sulphates, phosphate, protein, especially albumin, organic acids eg. lactic acid. In this case the AG was 132 + 4.2 – (98+9) = 29.2 – thus elevated AG. Increased anion gap acidosis can be due to: increased anion production (DKA, lactic acidosis, starvation, alcoholic ketoacidosis, inborn errors) or ingestion of toxins (salicylate OD, paraldehyde, methanol, ethylene glycol, cyanide, isoniazid, toluene), or acute/chronic renal failure. There are some great pneumonics to help you remember the causes of the acidosis. DULSI (like the old women’s name) is the easiest – Diabetes, Uraemia, Lactic acidosis, Salicylates , Intoxicants Increased Anion Gap acidosis: MUDSLEEP. Methanol, Uraemia, DKA, Salicylate, Lactate, Ethanol, Ethylene glycol, Paraldehyde + cyanide, + inborn errors of metabolism, + iron, isoniazid. Some people use the pneumonic MUDSLIDE to help them remember. Also consider the Osmolar Gap. Normal serum osmolality 280-300. Calculated serum osmolality = (2xNa) + Glucose + Urea. Osmolar Gap = Measured - Calculated. An osmolar gap > 10 is significant & indicates the presence of osmotically active substances eg. ethanol, methanol, ethylene glycol, isopropyl alcohol, mannitol. Normal Anion Gap acidosis can be due to: GIT loss of HCO3 (diarrhoea, ureterosigmoidostomy, anion-exchange resin, small bowel drainage, Ca Cl2, Mg Cl2., or Renal loss of HCO3 (carbonic anhydrase inhibitors, renal tubular acidosis, hyperparathyroidism, hypoaldosteronism), or other (dilutional acidosis, hyperalimentation acidosis, sulphur ingestion, HCl ingestion). Can use the pneumonic USED CARP. Ureteroenterostomy / obstructive uropathy, Small bowel fistula, Extra Cl, Diarrhoea, Carbonic anhydrase inhibitors, Addisons, Renal tubular acidosis, Pancreatic fistula. Low anion gap acidosis: can be due to Lithium toxicity (increased unmeasured cation), multiple myeloma (increased positive charge of abnormal proteins), hypercalcaemia, hyperMg, bromide intoxication. Lactic Acidosis can be divided into Type A or Type B. Type A: due to poor perfusion with tissue hypoxia eg. severe hypoxia, severe anaemia, haemorrhage, CCF, CO/CN poisoning, generalised seizures. Type B is where tissue hypoxia is not apparent such as in diabetes mellitus, Renal & liver failure, malignancy such as lymphoma, leukaemia or sarcoma, & drug ingestion such as ethanol, methanol & biguanides, salicylates, isoniazid, fructose, sorbitol; & congenital enz deficiencies (G6Pase defic). Editor: Peter Wyllie Compensated metabolic acidosis – the body will try to compensate when the pH reduces through the loss of exhaled CO2 - As useful rule in metabolic acidosis – the P aCO2 should equal the last 2 digits of the pH. However note you can get 2 pathologies occurring simultaneously – respiratory and metabolic eg aspirin overdose causing metabolic acidosis and respiratory alkalosis ALCOHOLIC KETOACIDOSIS In this case the patient had normal lactate levels and renal function with no other co-ingestants. The UA showed initially small ketones – repeated with moderate ketones. Ketones on dipstick was 6.4 (see below). The patient was given IV dextrose and later insulin IVI in addition to analgesia Alcoholic ketoacidosis (AKA) is an uncommon and frequently missed condition & as the signs & symptoms a patient with alcohol abuse presents with may be fairly non specific (abdo pain, vomiting, dehydration), the diagnosis may not be recognised. In general patients with AKA present post binge when the patient stops drinking. After the binge, appetite is often poor due to pain, fullness, vomiting etc. A starvation state develops with ketosis developing from fatty acid breakdown, complicated by dehydration from poor oral intake and vomiting. The patient presents with a high anion gap metabolic acidosis, vomiting, and signs of chronic ethanol abuse. AKA can develop in chronic alcoholics, but even in those who are relatively novice drinkers. AKA results from a complex interaction of ethanol metabolism, decreased caloric intake, volume depletion, and counter-regulatory hormones (eg, cortisol, glucagon). 3 mechanisms, which result in a relative deficiency of insulin with respect to glucagon, are thought to produce the state: 1. a lack of oral intake results in a depletion of glycogen stores. The body's starvation response includes a release of counter-regulatory hormones (epinephrine, cortisol, growth hormone), a decrease in serum insulin levels, and an increase in serum glucagon levels. 2. volume depletion may induce these counter-regulatory hormones, increasing glucagon levels while suppressing insulin. 3. the oxidation of ethanol produces acetaldehyde, which is oxidized to acetate. Both steps in this process convert nicotinamide adenine dinucleotide (NAD) to the reduced form of nicotinamide adenine dinucleotide (NADH), increasing the NADH/NAD ratio. This reduces hepatic gluconeogenesis, further reducing glucose levels. Hence, insulin levels remain suppressed, and serum glucagon levels remain elevated. The metabolism of alcohol itself is a probable contributor to the ketotic state. Ketone production is a protective mechanism during starvation to provide energy to the brain and other tissues. After consumption of available glycogen the body switches largely to fatty acids as a source of energy. In contrast to fatty acids, ketones can pass the blood-brain barrier to deliver energy to this organ. In early starvation ketones are also used for energy by muscle cells but later these convert to fatty acids to conserve ketones for the brain. These mechanisms assist in preserving carbohydrate supplies for cells dependent on sugars for energy supply such as red cells and the renal medulla. The ketones which may be found in the circulation are acetoacetate, beta-hydroxybutrate and acetone. They are produced in the liver in an environment of low insulin and low intracellular carbohydrate as an adaptive mechanism to provide non-carbohydrate fuel for the brain and other tissues in times of starvation. Acetoacetate is produced from acetyl CoA and may then either be converted enzymatically to betahydroxybutyrate or non-enzymatically to acetone. The interconversion of acetoacetate and betaEditor: Peter Wyllie hydroxybutyrate requries the enzyme beta-hydroxybutyrate dehydrogenase and the ratio of the two metabolites depends on the prevailing concentrations of NAD and NAHD. The patient may complain of the following: Nausea, vomiting, hematemesis, and/or abdominal pain (each found in 60-75% of patients) Dyspnoea, tremulousness, dizziness, and/or hematemesis (10-20% each) Muscle pain, fever, diarrhoea, syncope, seizure, and/or melaena (1-8% each) Examination usually reveals signs of alcohol abuse and dehydration. Shock related to volume depletion may be present. The mental state may be impaired. There may be abdominal pain related to pancreatitis. Investigate with baselines FBC, EUC, BSL, LFTs, amylase / lipase, coagulation studies, blood culture if infection is suspected; CXR (aspiration, infection or if tachypnoea is present). Ensure a bedside Dextrostix and correct hypoglycaemia urgently. Arterial blood gas examination may reveal a mixed picture Blood gas- venous or arterial ABG may show a low PCO2, low bicarbonate, and normal partial pressure of oxygen (PO2). Serum pH may be misleading because the patient with AKA actually may have a mixed acid-base disorder. In addition to metabolic acidosis due to ketone formation, a metabolic alkalosis may be present due to vomiting and volume depletion. A respiratory alkalosis may be present secondary to hyperventilation. The possibility of a double or triple acid-base disorder means serum pH may be near normal despite a severe acid-base disturbance. Urinalysis: UA for ketones may be negative or only weakly positive because the nitroprusside test detects acetone and Acetoacetate but not beta hydroxybutyrate. In AKA hydroxybutyrate production is favoured over acetylacetate in a ratio of 5:1. As treatment progresses this ratio shifts and with improvement the UA test for ketones may become more positive as increased amounts of acetylacetate are produced. The anion gap is elevated. Metabolic acidosis may also be due to lactic acidosis. Hyponatremia and hypokalemia have been reported in patients with AKA. Treatment Begin with oxygen administration and ensure adequate ventilation (note altered LOC may be present). Begin volume resuscitation if the diagnosis is suspected. All alcoholic patients require thiamine to prevent the development of Wernicke’s. All patients with severe AKA are dehydrated. Several mechanisms are responsible for dehydration, including protracted vomiting, decreased fluid intake, and inhibition of antidiuretic hormone secretion by alcohol. Dehydration is a stimulus to the sympathetic nervous system and is responsible for elevated cortisol and growth hormone levels. Dehydration and volume constriction both decrease the ability of the kidneys to excrete ketoacids. Shock and lactic acidosis can develop. Once shock has been corrected rehydration with 5% dextrose and N Saline should occur. Carbohydrate and fluid replacement (in the form of 5% dextrose in normal saline) reverses the pathophysiological derangements that lead to AKA. Replenishing carbohydrates and fluids increases serum insulin levels and suppresses the release of counter-regulatory hormones and glucagon. Dextrose stimulates the oxidation of NADH and aids in normalizing the NADH/NAD ratio. Fluids alone do not correct AKA as quickly as fluids and carbohydrates together. Consider K, Mg replacement as resuscitation progresses. Phosphate depletion is also commonly present in alcoholics. The plasma phosphate concentration may be normal on admission; however, it typically falls to low levels with therapy as insulin drives phosphate into the cells. When present, severe hypophosphatemia may be associated with marked and possibly life-threatening complications, such as myocardial dysfunction, in these patients Bicarbonate therapy should be considered only in the face of severe, life-threatening acidosis (ie, pH <7.1) that is unresponsive to fluid therapy. Evidence of pancreatitis is found in most patients, and many exhibit impaired glucose tolerance or mild type II DM after recovery from the acute episode. Editor: Peter Wyllie Unless the patient has prior diabetes or other reasons as to whuy they not produce insulin in response to the dextrose load, routine insulin administration is not recommended. The initial management should be in a high dependency setting till there is documented improvement in the metabolic state as indicated by an improving pH. In the patient with profound acid base disturbance, ICU admission may be initially required. Evaluate the patient for signs of alcohol withdrawal syndrome, which may include tremors, agitation, diaphoresis, tachycardia, hypertension, tremors, agitation, seizures, or delirium. Exclude other causes of autonomic hyperactivity and altered mental status. If the diagnosis of alcohol withdrawal syndrome is established, consider the judicious use of benzodiazepines, which should be titrated to clinical response. An alcohol withdrawal scale should continue to be monitored throughout the admission and D&A services should be involved early. Ketone Meter (Optium®) Acetoacetate (AcAC) is either converted enzymatically to beta-hydroxybutyrate (BOHB) or nonenzymatically to to acetone. AcAc and BOHB are moderately strong organic acids; acetone is an inert, volatile chemical. The BOHB/AcAc ratio is normally 1 to 2:1, and may reach 6 to 10:1 in DKA . Note, the urine analysis sticks use a nitroprusside reaction which detects Acetyl Acetate. Acetone is approximately 1/20 as reactive as AcAc but nitroprusside does not react with beta hydroxybutyrate. AS mentioned above in AKA hydroxybutyrate production is favoured over acetylacetate yet as treatment progresses this ratio shifts and with improvement, the UA test for ketones may become more positive as increased amounts of acetoacetate are produced. The ketone meter however detects beta-hydroxybutyrate, and thus is more reliable in detecting the relevant ketone bodies at a earlier stage as you don’t have to wait for the patient to pass urine. The meter takes ~ 30 seconds to provide a result. Due to cost reasons the people who it should be performed on are all sick diabetics or alcoholics or sick patients found to have hyperglycaemia (new Dx of diabetes). The below values and recommendations from the manufacturer for insulin dependent diabetics - <0.6mmol/L - 0.6-1.5mmol/L - 1.5-3.0 - > 3.0 - normal - mild hyperketonuria – extra insulin ~15% with adequate carbohydrates – “impending DKA” – extra insulin ~20% with adequate CHO – seen with DKA You need to look at each case individually but looking at these suggestions, I’d be checking a venous pH with all pts > 1.5 till we get a feel for the significance of those values 1.5-3.0. For those on insulin infusions for DKA or the AKA patients, I’d also be repeating the test every 4 -6 hrs looking for some improvement particularly after the acidosis (as reflected by the BE and bicarb – knowing that patients have a respiratory compensation) has resolved. Take Home Points: Calculate the anion gap when assessing metabolic acidosis – DULSI / USED CARP are the 2 mnemonics to remember Consider alcoholic ketoacidosis as a differential and use the ketone meter- UA is limited in value Treat AKA with good supportive management with a focus on extra carbohydrates, thiamine and electrolyte correction (esp K and PO4) - Editor: Peter Wyllie JOKE / Quote OF THE WEEK NEXT WEEK A colleague at RNSH treated where they had a 50yo cyclist who came off his bike, smashed his helmet and was amnesic and bruised and battered. The complicating issue was that he had a deep brain stimulator in place to manage his Parkinson's disease tremor. What are the implications of this to us in the ED ? Please forward any funny and litigious quotes you may hear on the floor (happy to publish names if you want) THE WEEK AHEAD Tuesdays - 11.30-2.30 Intern teaching -Thomas & Rachel Moore Wednesday 0800-0900 Critical Care Journal Club. ICU Conf Room / 12.30-1.30 Resident MO in Thomas & Rachel Moore Thursday 0730-0800 Trauma Audit. Education Centre / 0800-0830 MET Review Education centre / 1300-1400 Medical Grand Rounds. Auditorium. Editor: Peter Wyllie