* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download ESC Guidelines on Heart Failure
Heart failure wikipedia , lookup
Coronary artery disease wikipedia , lookup
Electrocardiography wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Myocardial infarction wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
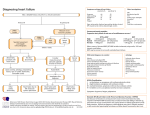
Heart Failure Guidelines 2016 What’s New? Michel KOMAJDA IHU ICAN - Département de Cardiologie CHU Pitié-Salpétrière Université Pierre et Marie Curie, Paris www.escardio.org/guidelines MAJOR CHANGES 1. A new term « HF with mid range ejection fraction » (HFmrEF). 2. A new algorithm for the diagnosis of HF. 3. Recommendations on prevention of HF. 4. Indications for the use of Sacubitril / Valsartan in HF with reduced ejection fraction (HFrEF). 5. Indications for cardiac resynchronisation therapy. 6. A new algorithm for the diagnosis and the management of acute HF. 7. A list of drugs contra-indicated in HFrEF. www.escardio.org/guidelines WHAT DOES NOT CHANGE ? First line therapies in chronic heart failure with reduced ejection fraction (HFrEF). 1 4 2 Indications for implantable cardiac defibrillator 3 Lack of evidence for the treatment of HF with preserved ejection fraction. Gaps in evidence. www.escardio.org/guidelines Definition HF is a clinical syndrome characterized by typical symptoms (e.g. breathlessness and fatigue) that may be accompanied by signs (e.g.ankle swelling, elevated jugular venous pressure, pulmonary crackles and peripheral oedema) caused by a structural and/or functional cardiac abnormality, resulting in a reduced cardiac output and/or elevated intracardiac pressures at rest or during stress. www.escardio.org/guidelines A new algorithm for the diagnosis of chronic HF Based on clinical probability of HF Based on the assessment of circulating natriuretic peptides, and on transthoracic echocardiography. www.escardio.org/guidelines Diagnostic algorithm for a diagnosis of heart failure of non-acute onset PATIENT WITH SUSPECTED HFa (non-acute onset ASSESSMENT OF HF PROBABILITY I. Clinical history: History of CAD (MI, revascularization) History of arterial hypertension Exposition to cardiotoxic drug / radiation Use of diuretics Orthopnoea / paroxysmal nocturnal dyspnoea 2. Physical examination: Rales Bilateral ankle oedema Heart murmur Jugular venous dilatation Laterally displaced/broadened apical beat www.escardio.org/guidelines 3. ECG: Any abnormality Diagnostic algorithm for a diagnosis of heart failure of non-acute onset 3. ECG: Any abnormality All absent I present Assessment of natriuretic peptides not routinely done in clinical practice NATRIURETIC PEPTIDES No . NT-proBNP 125 pg/mL . BNP 35 pg/mL Yes ECHOCARDIOGRAPHY If HF confirmed (based on all available data): determine aetiology and stard appropriate treatment www.escardio.org/guidelines Normal HF unlikely: Consider other diagnosis 9 A New Classification Heart failure with preserved, mid-range and reduced EF CRITERIA Type of HF HFrEF HFmrEF HFpEF I Symptoms ± Signs² Symptoms ± Signs² Symptoms ± Signs² 2 LVEF < 40% LVEF 40 – 49% LVEF 50% 3 - 1. Elevated levels of natriuretic peptidesb, 2. At least, one additional criterion: a. relevant structural heart disease (LVH and/or LAE); b. diastolic dysfunction (for details see Section 4.3.2). 1. Elevated levels of natriuretic peptidesb, 2. At least, one additional criterion: a. Relevant structural heart disease (LVH and/or LAE), b. Diastolic dysfunction (for details see Section 4.3.2). The only category with evidence based medicine is HF rEF www.escardio.org/guidelines Prevention of heart failure Treatment of risk factors (hypertension, diabetes, obesity, smoking cessation). Use of statins in patients with or at high risk of coronary artery disease. Use of ACE-I in patients with asymptomatic left ventricular dysfunction /stable CAD. -Use of beta-blockers in those with asymptomatic left ventricular dysfunction and a history of myocardial infarction. www.escardio.org/guidelines Objectives of the treatment of heart failure with reduced ejection fraction Reduce mortality Improve clinical status functional capacity quality of life, prevent hospital admission Preventing HF hospitalizations and improving functional capacity. www.escardio.org/guidelines Treatment Algorithm for HFrEF We are HFA Initial management of symptomatic HF with reduced ejection fraction. www.escardio.org/guidelines Therapeutic algorithm for a patient with persistent symptomatic HF with reduced ejection fraction. www.escardio.org/guidelines SHIFT CV death / HF hospitalization 40 Placebo -18% p<0.0001 30 Ivabradine 20 10 0 0 6 12 18 24 30 Months Swedberg K, et al. Lancet 2010;376: 875-885. If-channel inhibitor Ivabradine is indicated in patients with: symptomatic HFrEF and LVEF ≤35% in sinus rhythm and with a heart rate ≥70 bpm who had been hospitalized for HF within the previous 12 months. The European Medicines Agency (EMA) approved ivabradine for use in Europe in patients with HFrEF with LVEF ≤35% and in sinus rhythm with a resting heart rate ≥75 bpm, because in this group ivabradine conferred a survival benefit. Main side effects :bradycardia, blurred vision LCZ 696: Angiotensin Receptor Neprilysin Inhibitor Heart Failure Natriuretic Peptide System Renin Angiotensin System pro-BNP Angiotensinogen (liver secretion) Angiotensin I BNP NT-pro BNP LCZ696 Angiotensin II O Neprilysin Inactive fragments 17 X O N OH X O HN OH O HO N N N NH AT1 receptor O Vasodilation blood pressure sympathetic tone aldosterone levels fibrosis hypertrophy Natriuresis/Diuresis AHU377 ↓ LBQ657 Valsartan Vasoconstriction blood pressure sympathetic tone aldosterone fibrosis hypertrophy PARADIGM HF Cardiovascular death / Heart Failure hospitalisation 40 1117 Kaplan-Meier Estimate of Cumulative Rates (%) Enalapril 32 (n=4212) 914 24 LCZ696 (n=4187) 16 HR = 0.80 (0.73-0.87) P = 0.0000002 Number needed to treat = 21 8 0 0 180 360 720 900 1080 1260 1544 1488 896 853 249 236 Days After Randomization Patients at Risk LCZ696 Enalapril 540 4187 4212 3922 3883 3663 3579 3018 2922 2257 2123 JJV McMurray et al, NEJM 2014 online Angiotensin receptor neprilysin inhibitor (Sacubitril/Valsartan) LCZ 696 is indicated in patients with: ambulatory, symptomatic HFrEF LVEF ≤35% elevated plasma NP levels (BNP ≥150 pg/mL or NT-proBNP ≥600 pg/mL) estimated GFR (eGFR) ≥30 mL/min/1.73 m2 of body surface area who are able to tolerate treatment with enalapril (at least 10 mg b.i.d.) Side effects: symptomatic hypotension. risk of angioedema (ACEI should be withheld for at least 36 h before initiating LCZ696). Therapeutic algorithm for a patient with symptomatic HF with reduced ejection fraction. Next steps www.escardio.org/guidelines Other pharmacological treatments recommended in selected patients with symptomatic (NYHA Class II-IV) HFrEF Angiotensin II type I receptor blockers ARBs are recommended only as an alternative in patients intolerant of an ACEI. The combination of ACEI/ARB should be restricted to symptomatic HFrEF patients receiving a beta-blocker who are unable to tolerate an MRA, and must be used under strict supervision. Combination of hydralazine and isosorbide dinitrate There is no clear evidence to suggest the use of this fix-dose combination therapy in all patients with HFrEF. This combination may be considered in patients who can tolerate neither ACEi nor ARB. Other treatments with less certain benefit in symptomatic patients with HFrEF Digoxin and other digitalis glycosides Digoxin may be considered in patients in sinus rhythm to reduce the risk of hospitalisation in symptomatic patients with HFrEF It is only recommended for the treatment of patients with HFrEF and AF with rapid ventricular rate when other therapeutic options cannot be pursued Digitalis should always be prescribed under specialist supervision. Caution should be exerted in females, in the elderly and in patients with reduced renal function. Treatments not recommended in symptomatic patients with HFrEF Statins Oral anticoagulants and antiplatelet therapy Except in patients with atrial fibrillation There is no evidence on the benefits of antiplatelet drugs in patients with HF without accompanying CAD, whereas there is a substantial risk of GI bleeding. Renin inhibitors It is not presently recommended as an alternative to an ACEI or ARB ATMOSPHERE Main Outcomes McMurray JJV et al. N Engl J Med 2016;374:1521-1532 Treatments (or combinations of treatments) that may cause harm in patients with symptomatic (NYHA Class II–IV) HFrEF Recommendations Classa Levelb Thiazolidinediones (glitazones) are not recommended in patients with HF, as they increase the risk of HF worsening and HF hospitalization. III A NSAIDs or COX-2 inhibitors are not recommended in patients with HF, as they increase the risk of HF worsening and HF hospitalization. III B Diltiazem or verapamil are not recommended in patients with HFrEF, as they increase the risk of HF worsening and HF hospitalization. III C The addition of an ARB (or renin inhibitor) to the combination of an ACE-I and an MRA is not recommended in patients with HF, because of the increased risk of renal dysfunction and hyperkalaemia. III C www.escardio.org/guidelines ESC Heart Failure Guidelines Manage HF co-morbidities in all heart failure patients. www.escardio.org/guidelines EMPAREG OUTCOME Zinman B et al. N Engl J Med 2015;373:2117-2128 ESC Heart Failure Guidelines: devices www.escardio.org/guidelines Implantable cardioverter-defibrillator in patients with heart failure Recommendations Class Level I A I A I B III A III C Patients should be carefully evaluated by an experienced cardiologist before generator replacement, because management goals and the patient’s needs and clinical status may have changed. IIa B A wearable ICD may be considered for patients with HF who are at risk of sudden cardiac death for a limited period or as a bridge to an implanted device. IIb C Secondary prevention An ICD is recommended to reduce the risk of sudden death and all-cause mortality in patients who have recovered from a ventricular arrhythmia causing haemodynamic instability, and who are expected to survive for >1 year with good functional status. Primary prevention An ICD is recommended to reduce the risk of sudden death and all-cause mortality in patients with symptomatic HF (NYHA Class II–III), and an LVEF ≤35% despite ≥3 months of OMT, provided they are expected to survive substantially longer than one year with good functional status, and they have: • IHD (unless they have had an MI in the prior 40 days – see below). • DCM. ICD implantation is not recommended within 40 days of an MI as implantation at this time does not improve prognosis. ICD therapy is not recommended in patients in NYHA Class IV with severe symptoms refractory to pharmacological therapy unless they are candidates for CRT, a ventricular assist device, or cardiac transplantation. www.escardio.org/guidelines Recommendations for cardiac resynchronization therapy implantation in patients with heart failure Classa Levelb CRT is recommended for symptomatic patients with HF in sinus rhythm with a QRS duration 150 msec and LBBB QRS morphology and with LVEF 35% despite OMT in order to improve symptoms and reduce morbidity and mortality. I A CRT should be considered for symptomatic patients with HF in sinus rhythm with a QRS duration 150 msec and non-LBBB QRS morphology and with LVEF 35% despite OMT in order to improve symptoms and reduce morbidity and mortality. IIa B CRT is recommended for symptomatic patients with HF in sinus rhythm with a QRS duration of 130-149 msec and LBBB QRS morphology and with LVEF 35% despite OMT in order to improve symptoms and reduce morbidity and mortality. I B CRT may be considered for symptomatic patients with HF in sinus rhythm with a QRS duration of 130-149 msec and non-LBBB QRS morphology and with LVEF 35% despite OMT in order to improve symptoms and reduce morbidity and mortality. IIb B CRT should be considered for patients with LVEF 35% in NYHA Class III-Ivc despite OMT in order to improve symptoms and reduce morbidity and mortality, if they are in AF and have a QRS duration 130 msec provided a strategy to ensure bi-ventricular capture is in place or the patient is expected to return to sinus rhythm. IIa B Recommendations www.escardio.org/guidelines Acute heart failure www.escardio.org/guidelines Clinical profiles of patients with acute heart failure based on the presence/absence of congestion and/or hypoperfusion CONGESTION (‒) HYPOPERFUSION (‒) HYPOPERFUSION (+) Cold sweated extremities Oliguria Mental confusion Dizziness Narrow pulse pressure CONGESTION (+) Pulmonary congestion Orthopnoea/paroxysmal nocturnal dyspnoea Peripheral (bilateral) oedema Jugular venous dilatation Congested hepatomegaly Gut congestion, ascites Hepatojugular reflux WARM-DRY WARM-WET COLD-DRY COLD-WET Hypoperfusion is not synonymous with hypotension, but often hypoperfusion is accompanied by hypotension www.escardio.org/guidelines Management of patients with acute heart failure based on clinical profile during an early phase www.escardio.org/guidelines PATIENT WITH ACUTE HEART FAILURE Bedside assessment to identify haemodynamic profiles PRESENCE OF CONGESTION ? Yes (95% of all AHF patients) No (5% of all AHF patients) ‘’Wet’’ patient ‘Dry’’ patient ADEQUATE PERIPHERAL PERFUSION ? Yes No ‘Wet and Warm’ patient (typically elevated or normal systolic blood pressure) Vascular type – fluid accumulation Hypertension prédominates • Vasodilator • Diuretic Cardiac type – fluid accumulation Congestion prédominates • Diuretic • Vasodilator • Ultrafiltration (consider if diuretic resistance) No Yes ‘Dry and warm’ Adequately perfused = Compensated Dry and cold’ Hypoperfused, Hypovolemic Adjust oral therapy Consider fluid challenge Consider inotropic agent if still hypoperfused ‘’Wet and Cold’’ patient Systolic blood pressure <90 mmHg Yes • Inotropic agent • Consider vasopressor in refractory cases • Diuretic (when perfusion corrected) • Consider mechanical circulatory support if no response to drugs No • Vasodilators • Diuretics • Consider inotropic agent in refractory cases ESC Heart Failure Guidelines : Ten Commandments Enrol the patients with HF in a multidisciplinary care management program in order to reduce the risk of HF hospitalization and mortality. www.escardio.org/guidelines Gaps in evidence Clinicians responsible for managing patients with HF must frequently make treatment decisions without adequate evidence or a consensus of expert opinion. The following is a short list of selected, common issues that deserve to be addressed in future clinical research: Indications for ICDs in specific subgroups (e.g. ARVC and HFmrEF / HFpEF) and optimal selection of ICD candidates. QRS morphology or duration as a predictor of response to CRT. CRT in patients with AF. Efficacy of PV ablation as a rhythm-control strategy in patients with AF. Interventional approach to recurrent, live-threatening ventricular tachyarrhythmias. The role of remote monitoring strategies in HF. Non-surgical (percutaneous) correction of functional mitral and tricuspid regurgitations. Identification of indications for coronary angiography/revascularization in patients with HF and chronic stable CAD; Effects of novel LVADs as destination therapy and bridge to transplantation. www.escardio.org/guidelines Heart Failure 2017 29 April – 2 May 2017 4 days of scientific exchange 108 scientific sessions 6 148 healthcare professionals 100 + countries represented 2010 300 abstracts and cases submitted expert faculty members 2000m exhibition space 40 industry sessions and workshops 2 Call for abstracts opens on November 3 www.escardio.org/heartfailure