* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Topic 2 X-rays and ECGs
Radiation burn wikipedia , lookup
Center for Radiological Research wikipedia , lookup
Image-guided radiation therapy wikipedia , lookup
Radiosurgery wikipedia , lookup
Backscatter X-ray wikipedia , lookup
History of radiation therapy wikipedia , lookup
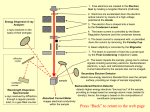
Industrial radiography wikipedia , lookup
Unit P3: Applications of physics Topic 2 X-rays and ECGs Student Notes Unit P3: Applications of physics Topic 2 X-rays and ECGs We Are Learning To 2.2 Explain the key features of passing a current through an evacuated tube, including: a thermionic emission of electrons from a heated filament b potential difference between the cathode (filament) and the anode (metal target) c why the vacuum is necessary d possible production of X-rays by collision with a metal target Note: only underlined parts are covered in this lesson Experiments by J. J. Thomson in 1897 led to the discovery of the electron, and the award of the 1906 Nobel prize. He detected electrons as they landed on a fluorescent screen. Filament bulb When an electric current heats up a metal filament – electrons are ‘boiled off’. We call this thermionic emission. The atom is so hot it changes to an ion and emits the electron. Although this occurs in a light-bulb filament, you are not aware of the electrons being emitted. Unlike the light from the filament, the electrons cannot pass through the glass bulb. How the electron gun part of the cathode ray tube works 1. Negative electrons are boiled off (thermionic emission) at the filament (cathode) 2. An accelerating voltage of 4000 V between the cathode and anode accelerates the negatively charged electrons towards the positive anode to high speeds. 3. Some of the electrons pass through a small hole in the anode and come out as an electron beam on the other side. Note: The apparatus must be in a vacuum, otherwise air molecules would stop the electrons by getting in their way. (Negative) filament cathode (Positive) accelerating anode A 6V supply to the filament Accelerating Voltage 4000V Deflecting a beam of electrons Parallel charged metal plates create an electric field and deflect the electron beam. The path of the electron beam can be changed by: 1. Increasing the accelerating voltage - the electrons will move faster and will not be deflected by the plates as much 2. Increasing the voltage between the deflection plates – this will deflect the electron beam more 3. Changing the charge on the plates - if the top deflection plate is negative and the bottom deflection plate is positive the beam will be deflected downwards (Negative) filament cathode Charged deflection plates (Positive) accelerating anode + A 6V supply to the filament Accelerating Voltage 4000V Unit P3: Applications of physics Topic 2 X-rays and ECGs We Are Learning To 2.1 Relate the ionisation by X-rays to their frequency and energy qualitatively (E = hf is not required) 2.2 Explain the key features of passing a current through an evacuated tube, including: a thermionic emission of electrons from a heated filament b potential difference between the cathode (filament) and the anode (metal target) c why the vacuum is necessary d possible production of X-rays by collision with a metal target Note: only underlined parts are covered in this lesson In 1895, a German physicist, Wilhelm Röntgen discovered X-rays The Nobel Prize in Physics 1901 "in recognition of the extraordinary services he has rendered by the discovery of the remarkable rays subsequently named after him" Cathode Ray Tube (X-Rays) X-Rays, such as those produced by this machine, are produced using an electron gun. Tungsten target Lead casing Cathode metal target cathode Anode X-rays X-Rays are produced by firing high energy electron beams at a tungsten anode. Higher energy X-rays can be produced by increasing the accelerating voltage. X-rays Increasing frequency The higher the accelerating anode voltage the greater the frequency of the X-rays that are produced Higher frequency = higher energy = more ionising = more danger! Unit P3: Applications of physics Topic 2 X-rays and ECGs We Are Learning To 2.3 Explain why a beam of charged particles is equivalent to an electric current 2.4 Use the equation: current (ampere, A) = number of particles per second (1/ second, 1/s) x charge on each particle (coulomb, C) I=Nxq 2.5 Use the equation: kinetic energy (joule, J) = charge on the electron (coulomb, C) x accelerating potential difference (volt, V) KE = ½ mv2 = e x V Think of a moving electron in a CRT. e- We know that kinetic energy is given by: KE = ½ mv2 Where has it got this energy from? Answer: the accelerating voltage (V) Kinetic energy = charge of electron x accelerating potential difference KE = e x V KE = ½ 2 mv =exV e- v = velocity of the electron (metres per second, m/s) m = mass of an electron (kilograms, kg) e = charge on the electron (coulomb, C) V = accelerating potential difference (volt, V) KE = kinetic energy (joules, J) The charge on an electron is 1.6 × 10-19 C The mass of an electron is 9.1 × 10-31 kg Question 1 If the accelerating voltage in an electron gun is 3 kV, what is the kinetic energy of the electrons in the beam? The charge on an electron is 1.6 × 10-19 C. KE = eV KE = 1.6x10-19 x 3000 KE = 4.8 x10-16 J (3 marks) Question 3 What is the velocity of an electron that has been accelerated by the 2.5 kV anode voltage of a television picture tube? The charge on an electron is 1.6 × 10-19 C The mass of an electron is 9.1 × 10-31 kg KE = eV KE = 1.6x10-19 x 2500 KE = 4.0 x10-16 J KE = ½ mv2 4.0 x10-16 = 0.5 x 9.1 x 10-31 x v2 4.0 x10-16 = 4.55 x 10-31 x v2 4.0 x 10-16 = v2 4.55 x 10-31 8.79 x 1014 = v2 V = 29649973 m/s (2.96 x 107 m/s) e e e e e e e e e e What is current? Current is the rate of flow of electric charge around a circuit. e What is current? Current is the rate of flow of electric charge around a circuit. Electrons can flow in an electric circuit …… ….. and an electron beam. Current = number of particles flowing per second I = N x charge on each particle x q I = current in amperes, (A) N = number of particles flowing each second (1/s) q = charge on each particle in coulombs (C) Question 4 2.2 x 1014 electrons reach the anode per second. What is the current? The charge on an electron is 1.6 × 10-19 C I=Nq I = 2.2 x 1014 X 1.6 x 10-19 I = 0.0000352 A Or I = 3.52 x 10-5 A Exam Style Question: (a) The acceleration voltage between the cathode and anode is 8 000 V. Calculate the kinetic energy of one electron when it has reached the anode. Charge on 1 electron e = 1.6 × 10–19C KE = eV KE = 1.6x10-19 x 8000 KE= 1.28 X 10-15 J (b) 5.2 × 1016 electrons reach the anode per second. Calculate the current. I = N q I = 5.2 × 1016 x 1.6 x 10-19 I = 0.00832 A I = 8.32 × 10–3 A Unit P3: Applications of physics Topic 2 X-rays and ECGs We Are Learning To 2.6 Demonstrate an understanding of the inverse square law for electromagnetic radiation Intensity (brightness) The intensity depends on: • The distance from the source • The medium the radiation is travelling through the word ‘radiation’ is used to describe any form of energy, e.g. wave or particle originating from a source the intensity of radiation will decrease with distance from a source and according to the nature of the medium through which it is travelling Intensity The strength of a radiation is called its intensity. This is the power of the radiation per square metre and is measured in W/m2 Intensity (W/m2) = Power (W) Area (m2) Investigating how electromagnetic radiation spreads out as you increase distance 1metre Measure area Now move the projector to 2 m away and measure the area! Inverse Square Law Intensity = 1 d2 Source When electromagnetic radiation is emitted by a source, it spreads out and its strength (intensity) decreases the further you are from the source. When you double the distance from the source, the strength decreases to a quarter. The strength decreases according to the inverse square law. 1m 2m 3m When the radiations used for medical purposes pass through the body, they are not in a vacuum, they are in a medium. However, there is a similar pattern of decreasing intensity. Each material in the body reduces the intensity of the radiation by different amounts. Bone is dense and reduces the intensity the most. Muscle is less dense so it does not decrease the intensity as much. Graph showing the results of an experiment to measure intensity at different distances through a medium. Unit P3: Applications of physics Topic 2 X-rays and ECGs We Are Learning To 2.7 Relate the absorption of X-rays to the thickness of the material through which they are travelling, quantitatively 2.8 Describe how X-rays are used in CAT scans and fluoroscopes 2.9 Demonstrate an understanding of the comparison of the risks and advantages of using X-rays for treatment and diagnosis X-rays can be used to diagnose some medical conditions. X-ray photography X-rays can penetrate the body. The photographic film is turned from white to black by X-rays, so the more X-rays that are absorbed by an area of the body, the whiter that area will appear. This is why bones appear white on X-ray photographs. X-ray machine patient X-ray film Fluoroscopic (fluoroscopy) An X-ray procedure that produces immediate images and motion on a screen. The images look like those seen at airport baggage security stations. X-rays - airport security Fluoroscope France bans Britain's migrant X-ray scanner... because it might breach health and safety (Jan 2008) British border guards in Calais have been banned from using X-rays to search for illegal immigrants in lorries - unless they ask for the stowaways' written permission. French authorities have blocked the use of the scanners, claiming they could breach European health and safety laws. baby girl having a fluoroscope scan. Fluoroscopes are used to show a patient’s organs working. They consist of an X-ray source and an X-ray detector attached to a digital video camera. The patient is placed between the X-ray source and the detector. Computed (Axial) Tomography CAT / CT scans CAT scans use the different absorption of Xrays by bones and tissue and images taken from a number of different angles and positions to build up a 3D picture of the inside of the body of superb quality. Diagnostic and preventive scans: • Investigate cancerous tumours • Watch the heart in motion • Check for colon (bowel) cancer • Study haemorrhaging, bone trauma and lots more… ‘Slices’ through the body • CT scanners create a 2D image that is like a slice through the body, a bit like a slice of bread. • Many 2D images can be used to reconstruct a 3D image. BBC News, Sept 27 2010 A food production company was ordered to pay nearly £17,000 after a man found a dead mouse in a loaf of bread as he made sandwiches for his children. 34 What’s it like to have a CT scan? • A CT scanner is an X-ray machine rotated at high speed – so it’s pretty noisy… (see open CT scanner clip) • … but non-invasive. • It takes between a few minutes and an hour. • Sometimes you’re given an injection of a chemical to increase the contrast of the images. • You need to lie still with your arms above your head for the best image of the chest or body. CT Scan - What to Expect (UW Medicine) - YouTube.flv Dangers of X-rays This woman, like thousands of others, suffered from burns, scarring, and cancer after undergoing X-Ray "beauty treatments". Early X-Ray technicians fell victim to the horrible side-effects of radiation. Today we are aware of the dangers of X-rays. X-rays are ionising Early protective suits made of heavy aprons and metal helmets Ionising radiation can damage DNA. This could cause… 1. Cancer 2. Inflammation 3. Cell death 4. Damage to genes can lead to mutations in offspring Workers who work with radiation every day e.g. hospital staff/nuclear power plant workers need to: (1) monitor the dose they are being exposed to staff wear special badges that monitor their exposure. (2) take precautions to reduce the dose they are exposed to - leave the room or go behind a lead or thick concrete shield whilst a patient is being given radiation treatment Is ionising radiation harmful? Ionising radiation can damage DNA. This could cause… 1. Cancer 2. Inflammation 3. Cell death 4. Damage to genes can lead to mutations in offspring Cells are more sensitive to radiation during cell division than at other times. Cells which divide frequently (e.g. the gut walls) are more sensitive than those which rarely divide (e.g. nervous tissue). X-rays can be used to treat some medical conditions. Radiotherapy The tumour is exposed to X-rays radiation at different angles. This gives normal cells a low dose of radiation, while the tumour receives a high dose. However, levels have to be carefully monitored so that healthy cells are not damaged as well. Rotating X-ray source tumour In some patients radiation treatment may not be able to destroy the cancer. Sometimes it is used only to reduce suffering (palliative care). Unit P3: Applications of physics Topic 2 X-rays and ECGs We Are Learning To 2.10 Explain how action potentials can be measured with an electrocardiogram (ECG) to monitor heart action 2.11 Relate the characteristic shape of a normal ECG to heart action 2.12 Use the equation: frequency (hertz, Hz) = 1/time period (second, s) f = 1/T 2.13 Describe the use of a pacemaker to regulate the heart action Right Atrium Left Atrium Right Left Ventricle Ventricle An electrocardiogram (ECG) measures the electrical activity of the heart. An ECG trace can then be used to calculate a patients heart rate and to check for abnormalities. Action potential When a heart beats, each muscle cell must contract at exactly the right moment in order to push the blood out of the heart. An action potential (electrical signal) is sent to each muscle cell to tell it when to contract. This electrical signal starts in the SA node (pacemaker). The human body contains a high proportion of water with salt dissolved in it, which means that it will conduct electricity. The action potentials are conducted through the body to the skin, where they can be detected and used to produce an electrocardiogram (ECG). Pacemakers Some people’s hearts do not beat properly. The action potentials do not spread across the heart properly. A pacemaker can be attached to the heart. The pacemaker detects the action potentials, amplifies them and transmits them to other parts of the heart, so that the chambers of the heart contract correctly. 1. The SA node (pacemaker) produces an electrical stimulus A V 5. Cells in ventricle relax. A V 2. The cells in the atria contract. 3. The AV node delays conducting the impulse from the atria to the ventricles. This delay allows the atria to fill the ventricles with blood before they contract. 4. Cells in the ventricles contract. QRS-wave is due to the contraction of the ventricles P-wave is due to the contraction of the atria T wave is due to the relaxation of the ventricles frequency (hertz, Hz) = 1/time period (second, s) f=1 T 0.8 Frequency = 1 time period Frequency = 1 0.8 1.25 bps 1.25 bps x 60 75 Unit P3: Applications of physics Topic 2 X-rays and ECGs We Are Learning To 2.14 Describe the principles and use of pulse oximetry the word ‘radiation’ is used to describe any form of energy, e.g. wave or particle originating from a source the intensity of radiation will decrease with distance from a source and according to the nature of the medium through which it is travelling Pulse Oximetry Used to measure: 1. Heart rate 2. Oxygen concentration in blood Non-intrusive/non-invasive technique (no cutting/no surgery/no needles) A fit, healthy person should have an oxygen saturation level between 95% & 100%. If the blood is 95% saturated. This is written 95 SPO2%. Pulse Oximeters are routinely used on the wards and in casualty department. Hypoxia (medical) a shortage of oxygen in the body Hypoxia (environmental) a condition in high altitudes such as mountains where the reduced partial pressure of oxygen available leads to hypoxia Photodetector Oxygenated blood absorbs more IR light than red light. IR LEDs LEDs L Beam of red light Beam of infrared li Red IR Red LEDs Photodetector Photodetector Poorly oxygenated blood absorbs more red light than IR light Amount of red and IR detected by photodector Oxygenated blood Poorly oxygenated blood Red IR Red IR Emission Absorption Transmission How does a pulse oximeter calculate heart rate? During a pulse the arteries stretch, their volume increasing in the moment after the heart contracts and pushes out blood. As the pulse of blood passes through the beam of light from the LEDs, the blood absorbs more of the light and the photodetectors receive less light, so the reading changes. Each change is detected as a pulse.