* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download View - OhioLINK ETD
Heart failure wikipedia , lookup
Coronary artery disease wikipedia , lookup
Aortic stenosis wikipedia , lookup
Myocardial infarction wikipedia , lookup
Cardiac surgery wikipedia , lookup
Electrocardiography wikipedia , lookup
Jatene procedure wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
EFFECTS ON BARORECEPTOR SENSITIVITY OF REPEATED ANESTHESIA
WITH MORPHINE-CHLORALOSE IN THE DOG
A Thesis
Presented in Partial Fulfillment of the Requirements for the Degree Master of Sciences in
the Graduate School of The Ohio State University
By
Daise Nunes Queiroz da Cunha, DVM
*****
The Ohio State University
2005
Master's Examination Committee:
Dr. Robert L. Hamlin, DVM, PhD, Adviser
Dr. Kathryn Meurs, DVM, PhD
Dr. Mark Strauch, PhD
,
Approved by:
V\!\c
Adviser
Veterinary Biosciences
Graduate Pro gram
ABSTRACT
Systemic arterial blood pressure is regulated mainly by the high-pressure
baroreceptor reflex. This reflex is responsible for maintaining systemic arterial pressure
despite diseases and pharmacological perturbations. An example of disease would
congestive heart failure, in which the increase in sympathetic activity is responsible for
reduction in baroreflex sensitivity. The clinical relevance of the baroreflex dysfunction
lies in the fact that studies have shown that physical training and beta-adrenergic
blockage improves baroreceptor sensitivity, as well as the patient’s prognosis. To
investigate the baroreceptors in dogs, we hypothesized that baroreceptor function, as
assessed by gain and time-constant, does not change with repeated exposures to
morphine-chloralose anesthesia, which is a very common anesthestetic protocol used in
laboratories of veterinary research. To study baroreflex, the most used tests are the
oxford, neck suction, and tilt. The latter, is discussed in more detail here, since it was the
method used to evaluate the baroreceptor response to morphine-chloralose anesthesia.
The purpose of this study was to determine the effects of repeated doses of morphinechloralose anesthesia on baroreceptors function, by tilting the dogs, and histological
integrity, by blood profile and blood cell evaluations, as well as histopathology of the
important organs. To accomplish these goals, 7 healthy hound-type dogs (20-25 kg) and 3
healthy beagle-hounds (9.5 - 12 kg), males, between 1 and 3 years of age, and healthy
were studied. All dogs were given, IV, morphine sulfate (1.5 mg/kg) as a pre-anesthetic.
They were then given, IV as a bolus, alpha chloralose (100 mg/kg), after which they
received a continuous infusion of alpha chloralose (30 to 40 mg/kg/hour) to sustain
ii
anesthesia. Animals were ventilated with room air at a rate (12/minute) and a tidal
volume (12.5 ml/kg) to sustain systemic arterial PaCO2 of approximately 40mmHg.
To access pressure within the carotid sinus, a fluid-filled catheter, attached to a pressure
transducer, was advanced retrogradely into the region of the carotid sinus for 4 dogs. To
measure aortic arch sinus arterial pressure a fluid-filled catheter attached to a pressure
transducer was advanced through a femoral artery into the region of the junction of the
ascending aorta with the arch for 4 dogs. Electrodes forming ECG leads I and II were
attached to all. Six dogs were studied 3 times with 48 hours between studies. Each time,
the dogs were studied 3 times with 30 minutes in between. After baseline measurements
of pressures (4 dogs) and ECG’s (6 dogs) were made for 30 seconds, dogs were tilted
within <1second to a head-up-position. This head-up tilt was maintained for 20 seconds,
after which the dogs were returned to the horizontal. Measurements of pressures (4 dogs)
and ECG’s (6 dogs) were made the entire time. The results show that in regards to the
baseline heart rate did decrease consistently with days. Neither time (P=0.50) nor day
(P=0.92) was significantly associated with the maximum absolute increase in heart rate.
As the experiment advances from day 1 to day 2 to day 3, the absolute decrease in heart
rate becomes larger.
During the initial 5 seconds of the head-up tilt the heart rate
increased approximately 12 beats/minute, while peak systolic (p= 0.027), diastolic (p=
0.014), and mean pressures (p= 0.029) decreased more at the carotid sinus than at the
aortic sinus. For the calculated gain (6 dogs) there were no differences among means
either by day (p=0.14) or by time (p=0.992), nor was there a day-time interaction
(p =0.751). The recover from each anesthetic episode was not turbulent or violent.
Analysis of the blood constitutes tissues evaluated in the histology showed no alterations
due to anesthetic regimen. There were no differences of significance in gain. An
important limitation is the lack of assurance that constant levels of anesthesia were
maintained over the 3 recordings of each day, or if constant levels were achieved each
day. Recovery from this anesthetic protocol is relatively long compared to other
anesthetics (e.g. propofol, isoflurane). Finally buffering of the baroreceptor response
elicited from changing pressure at the carotid sinus may alter, profoundly, the role of only
the carotid sinus receptors. Therefore it was concluded that 1.repeated anesthesia with
iii
morphine/chloralose results in no observable pathological changes monitored by
histopathology, blood chemistry, and analysis of blood cellular components; 2.gain of
high-pressure baroreceptor reflex may be assessed using the passive head-up tilt; 3.gain
did not change significantly within an anesthetic period or on subsequent days; 4.for
head-up tilt, the change in pressure on the carotid sinus was greater than the change of
pressure on the aortic sinus.
iv
Dedicated to my family and friends
v
ACKNOWLEDGMENTS
I am thankful to my major adviser, Dr. Robert L. Hamlin, for his genuine and
grand enthusiasm to teach, support and guide me throughout this journey. His example of
strength and courage has inspired many to pursue their careers with success. For all these
reasons, this has been an enjoyable experience of learning.
I would like to express my appreciation to my husband, Luis, for his love,
incentive and support in the most challenging moments. I am also immensely grateful to
my mother, father, and brother for their unconditional love.
I thank Dr. March Strauch, for being supportive all the times I needed his
assistance, and for his interest with my research.
To Dr. Kathryn Meurs, I would like to express my gratitude for her cooperation
kindness, and flexibility in the most crucial times.
I want acknowledge Dr. Yoshinori Nishijima, Dr. Francesca Travesso, Dr.
Adriana Pedraza, Paula Jenkins and Dr. Andy for all the extraordinary help with my
experiments, and finally for being such good friends.
My special thanks, to Dr. Matthew A. Buccelatto for his help with the
histophatology.
Finally I would like to recognize and thank Dr. Rajala-Schultz and her colleagues
for their assistance with the statistical analysis.
VI
VITA
September 30, 1976 ................ Bom-Ituiutaba, MG, Brazil
1997 - 2002 ........................... DVM
University Federal ofUberlandia, MG, Brazil
2002 - 2003 ........................... Internship
OARDC (Ohio Agricultural Research and Development Center)
The Ohio State University
2003 - 2004 ........................... Research Assistant
OARDC (Ohio Agricultural Research and Development Center)
The Ohio State University
2004 - present. ....................... Graduate Research Associate
The Ohio State University
vii
PUBLICATIONS
Moacir Santos Lacerda, Simone Tostes de Oliveira, Daise Nunes Queiroz.
Anatomical variations in the Dentition of Dogs crossbreed. In Agricultural Science,
Santa Maria, v.30, n.4, p.655-659, 2000.
1.
2.
Eduardo Mauricio Mendes de Lima; Frederico Ozanam Carneiro; Renato Souto
Severino; Andre Luiz Quagliatto Santos; Sergio Salazar Drummond; Valdiana Araujo
Leal; Daise Nunes Queiroz· Topographical study on the medullar cone in crossbreed
Zebu bovine fetus. Revista Ciencias. 10-12. art. 13, 2001.
3.
Julio Roquete Cardoso, Alan-kardec Martins, Daise Nunes Queiroz, Sergio
Salazar Drummond, Francisco Claudio Dantas Mota, Renato Souto Severino, Frederico
Ozanam Carneiro e Silva, Andre Luiz Quagliatto Santos. Origin and aspects of
ramification of the cranial and caudal mesenteric arteries in chickens. Bioscience
Journal. 18, n 1, 2002.
4.
Yunusemre Ozkanlar, Yoshinori Nishijima, Daise da Cunha, Robert L. Hamlin.
Acute effects of tacrolimus (FK506) on left ventricular mechanics. Pharmacological
Research. 52: 2005
FIELDS OF STUDY
Major Field: Veterinary Biosciences
Specialty: Cardiovascular Physiology, Pharmacology and Clinical Cardiology.
Vlll
TABLE OF CONTENTS
Page
Abstract ................................................................................................ .ii
Dedication ............................................................................................. v
Acknowledgments ................................................................................... vi
Vita .................................................................................................... vii
List of Tables .......................................................................................... x
List of Figures ........................................................................................ xi
List of Examples .................................................................................... xiv
Chapters:
1. Introduction ......................................................................................... 1
2. Literature Review .................................................................................. 4
3. Material and Methods ............................................................................ 34
4. Results ............................................................................................. 46
5. Discussion, Limitations, and Conclusions .................................................... 70
Bibliography ......................................................................................... 82
lX
LIST OF TABLES
Table
Page
I
Showing the measurements of the vertical distances between the
level of the carotid sinus and the heart .............................................. 37
2
Blood sample collected before the first experiment on day 1................... .40
3
Blood sample collected before the last experiment, on day 3 .................... 41
4
Histopathology .......................................................................... 42
5
The summary statistics of the heart rate at baseline, at tilt and at
recovery ................................................................................. 52
6
Absolute Change of The Heart Rate (Tilt and Recovery) ........................ 53
7
Pressure at carotid and aortic sinus, and heart rate changes during
the initial 5 seconds of the head-up .................................................. 65
8
Absolute_increase in heart rate and gain for 6 dogs during the initial
5 seconds of the head-up tilt ......................................................... 66
x
LIST OF FIGURES
Figure
Page
1
Effect of a stepwise pressure change in the isolated
aortic arch on heart rate .................................................................. 7
2
Schema showing the biological control system ..................................... . 11
3
Carotid and aortic sinus enervation and anatomy ................................... 12
4
Weight of the column ofblood ......................................................... 13
5
Morphine and alpha-chloralose chemical structure .................................. 16
6
Saturation point and threshold .......................................................... 20
4
Baroreceptor gain due to any perturbing force in the blood pressure ............. 21
5
The damping effect of the baroreceptor response to a perturbing
force in the blood pressure .............................................................. 25
10
Heart response to phenylephrine and nitroprusside
administration ............................................................................. 29
Xl
11
Blood pressure relationship with the firing of a
single afferent nerve fiber ............................................................... 30
12
Head-up and head-down tilt drawing ................................................. .32
13
A cut down in the neck for the insertion of a catheter
into the carotid sinus region ............................................................ 38
14
Graph of mean baseline heart rate versus time
for the 3 experimental days ............................................................. .47
15
Heart rate baseline for each dog on the 3 study days at the 3 times ............... 48
16
Mean absolute increase in heart rate versus time
for the 3 experimental days. . ........................................................... 50
17
Mean absolute decrease in heart rate versus time
for the 3 experimental days .............................................................. 51
18
Baseline heart rate versus time for the 3 experimental days ........................ 54
19
Absolute increase in heart rate versus time for the 3 experimental days .......... 55
20
Absolute decrease in heart rate versus time for the 3 experimental days ......... 56
21
Mean changes in heart and aortic sinus (various pressures)
during the initial 5 seconds of the head-up tilt ....................................... 62
22
Mean changes in heart and carotid sinus (various pressures)
during the initial 5 seconds of the head-up tilt ....................................... 63
Xll
23
Raw data from heart rate, carotid and aortic arch sinuses
pressures recorded during tilt.. ......................................................... 64
24
Calculated gain based on the heart rate change during
the 5 initial seconds of the head-up tilt.. .............................................. 67
25
Heart rate change during the 5 initial seconds
during the head-up tilt, for each of the 6 dogs ........................................ 68
26
Raw data of carotid sinus pressure fall precipitously ................................ 75
Xlll
LIST OF EXAMPLES
Example
Page
1
Row data of statistical analysis of heart rate baseline
made using the computer software, SAS ............................................. 63
2
Row data of statistical analysis of absolute increase in
heart rate baseline made using the computer software, SAS ....................... 65
3
Row data of statistical analysis of absolute decrease in
heart rate baseline made using the computer software, SAS ....................... 67
XIV
CBAPTERl
Introduction
Systemic arterial blood pressure, the force in systemic arteries that both moves
blood into capillaries and impedes the ejection from the left ventricle, is regulated by,
among other factors, the high-pressure baroreceptor reflex. That reflex is responsible for
maintaining
systemic
arterial
pressure
despite
diseases
and
pharmacological
perturbations. One of the distinguishing features of heart failure is cardio-acceleration
resulting from decreased parasympathetic traffic to the SA node that decreased traffic
resulting from inadequate baroreceptors function (Mortara,
1996~
Sopher, 1990).
Inadequate baroreceptors function may also lead to postural syncope following exposure
to various therapeutic agents.
The study of baroreceptors function, then, is of great importance to quantify the
severity of heart failure (Goldstein, 1975), to determine a putative mechanism for
postural hypotension, and to establish whether or not a potential therapeutic agent might
result in the inability to sustain systemic arterial blood pressure. The use of anesthetics is
critical
when
studying
baroreceptor
function
in
infrahuman
animals,
since
instrumentation can be otherwise painful, and psychological factors (i.e., perception of
being tilted) would influence the relationship between heart rate and blood pressure.
1
The baroreceptor in the hypertensive animals differs from those in normotensive animal
(McCubbin, 1956). In hypertension, they are reset to have a higher operating threshold;
therefore their sensitivity to increments in pressure may be reduced (Brown, 1980). It has
been suggested that enhanced Na+,K(+)-ATPase activity, caused by elevated
aldoretorone,
in baroreceptors is responsible for the blunted baroreceptor discharge
sensitivity seen inheart failure state (Wang, 1992).
The baroreceptors reflex is expressed (Berne and Levy, 1972) as the change in
heart rate per change in mean systemic arterial pressure. Thus, this reflex may be
interrogated by changing systemic arterial blood pressure and measuring the change in
heart rate (Berne and Levy, 1972). In humans the reflex may be quantified by changing
pressure with various drugs-Oxford Method (Davies, 1999; Smyth, 1969) or by directly
stimulating high- pressure baroreceptors by neck suction (Eckberg, 1975). However, in
infrahuman mammals that do not cooperate (i.e., lay still) and may be perturbed by the
change in pressure, it is virtually impossible to explore the baroreceptor reflex without
need for chemical restraint. All means of chemical restraint are likely to alter the
baroreceptor reflex and vagal tone (Halliwill, 1992). Furthermore, if chemical restraint is
required to study the reflex repeatedly, it is not well understood whether the expression of
the reflex is altered by the history of chemical restraints (Shimokawa, 1998; Vatner,
1971).
Thus the purpose of this study was to determine the effects of repeated doses of
morphine-chloralose anesthesia on baroreceptors function and histological integrity of
important tissues.
2
Hypothesis:
Baroreceptor function in dogs, as assessed by gain and time-constant, does not
change with repeated exposures to morphine-chloralose anesthesia.
Over-view of Plan:
Dogs were exposed to 3 episodes of morphine-chloralose anesthesia.
Baroreceptor function was assessed by tilting the dogs and plotting the subsequent heart
rate response. Baroreceptor function was quantified as the change in heart rate divided by
the change in pressure. The time-constant (tau) of the system was quantified as the time
required for heart rate to achieve 63% of the maximal change (Hall, 1999). After the 3rd
episode of anesthesia, blood chemistries were compared to pre-exposure. Dogs were
euthanatized and important tissues were examined for histopathology.
3
CHAPTER2
LITERATURE REVIEW
History of Baroreceptor Function
Probably the first description about carotid baroreceptor reflex was in antique
Rome, when Rufus ofEfesus (98 to 177 b.c.) observed that ifthe arteries from the neck
were firmly pressed, the animals would become sleepy (Willius & Dry, 1948). An
explanation for this phenomenon was attributed to the compression of the neck nerves,
not to compression on the vessels. This concept endured for 17 centuries after the death
of Rufus.
The anatomical origin of the carotid sinus reflex was first discovered by Sir
Astley Paston Cooper (1768-1841 ), a surgeon in London. Cooper ligated the common
carotid arteries during correction of an aneurism surgery in 1808, and observed that the
systemic arterial pressure increased in response to the arterial occlusion. However, he
described this response as being a consequence of impaired brain perfusion (Rawling,
1968). This knowledge perpetuated until the end of the century and was reinforced by
many other researchers in that era.
4
Other researchers continually studied the baroreflex in the carotid sinus for years,
but always coming to the same erroneous conclusion as Rufus (98-177 d.c.), and Cooper
(1836). In 1859 the French physician Etienne Marey described the inverse relationship
between arterial blood pressure and heart rate, which is known today as the "Marey's law
of the heart" (Figure 1) (Berne and Levy, 1972). Shortly thereafter, in 1870, Concato
suggested that only the region at the carotid-bifurcation was sensitive to mechanical
deformation. After that, Francois-Franck (1879), was probably the first to recognize the
action-reflex of the carotid sinus. Siciliano (1900) argued that, if the effects of the
occlusion of the carotid artery were due to the cerebral ischemia, the same pressure
response would be observed after ligation of the vertebral artery or occlusion of the
internal and external carotid artery .... which clearly did not occur (Haibara, 2000).
Only after the studies by Hering in 1927, was the carotid sinus reflex understood
as it is today. Hering studied 110 animals (dogs, rabbits, cats, and monkeys) to
demonstrate that mechanical simulation (such as, clamping, stretching, and pulling the
vagus nerve) did not produce a significant response in the arterial blood pressure and
heart rate. Furthermore, he demonstrated that mechanical stimulation of the carotid sinus
by means of clamping (without obstruction) or by deformation of the vessel (introduced a
catheter into the carotid sinus to infuse saline under high pressure gradient), produced
hypotension and bradychardia. He demonstrated further that stimulation of the carotid
sinus nerve produced the same cardiovascular reflex. Hering also demonstrated that these
reflexes responses (hypotension and bradychardia) occurred independently, since atopine
5
or the section of the vagus nerve abolished the cardiac response, with no significant
effects in the vasomotor response (Ziemmer, 2004 ).
Cyon and Ludwing (1866) shared the same concepts about the central nervous
system regulation in the cardiac activity. Based on these concepts, both described the
aortic baroreflex mediated via the cranial branch of the aortic depressor nerve, which
when stimulated induced hypotension and bradychardia. Similarly to the Hering' s
studies, Cyon and Ludwing also observed that atropine abolished only the bradychardic
response, while the hypotension was not altered.
6
150
100
Heart rate
(bpm)
50
0
.........................T ...............................T ................................r···································T···········..······················T································r············.........
Aortic
arch
pressure
200
(mmHg)
100
0
-30
0
30
60
90
120
Time (sec)
Figure 1: Effect of a stepwise pressure change in the isolated aortic arch on heart rate.
When pressure is raised, the mean heart rate decreases and there is an increase in the
magnitude of the rhythmic fluctuations of heart rate at the frequency of respiratory
movements. (redrawn from Berne & Levy, Cardiovascular Physiology, St Louis:
7
Cyon and Ludwing were the first to acknowledge the baroreflex as an "integrator
system" that controls the cardiovascular system (Haibara, 2000; Ziemmer, 2004).
Most recent electrophysiological studies have shown that elevation of arterial
pressure in the carotid sinus and aortic arch causes reflex inhibition of sympathetic
nervous activity (Bronk, 1936; Downing, 1963; Heymans, 1958). However, the inhibitory
effect on sympathetic activity disappeared when the carotid sinus, aortic, and vagal
nerves were cut (Heymans, 1958).
Baroreceptor Histology
The receptor endings are located in segments of the arterial system showing an
elastic structure ("Windkessel vessels") (Grigoreva, 1962; Muratori, 1967). A connective
tissue analysis showed that the concentration of elastin in the carotid sinus was larger
than in the common carotid artery, and the smooth muscle content was lower in the
carotid sinus compared to the common carotid artery (Bagshaw, 1971; Rees, 1970). The
extent to which the receptors stretch for a given transmural pressure depends on the
geometry of the vessel wall (internal radius and wall thickness), and the elastic property
of the vessel wall. The baroreceptors have a three-dimensional structure, which respond
to deformation of the vessel wall in all directions (Heymans, 1958, Paintal 1972).
There are two types of sensory nerve endings in the carotid sinus of mammals.
Generally, "type 1 receptors consist of a few thin myelinated fibers that run together for a
long distance until they form a diffuse arborization in a large loose plexus".
8
"Type 2 receptor are a single thick myelinated fiber which runs quite a distance
until an extremely rich arboriz.ation begins, and the very fine end branches terminate in
neurofibrilar end plates" (Abraham, 1967).
Baroreceptor function
It is important that the systemic arterial pressure be held within limits essential to
delivering quantities of blood adequate to sustain body function during all physiological
states (e.g., sleep, quiet, excitement). This must be accomplished despite changes in
effective circulating blood volume attending postural changes, alterations in blood
volume resulting from diseases, and effects of therapeutic agents-all of which may alter
systemic arterial blood pressure. The body contains two sets of reflexes, which maintain
hemodynamic homeostasis: low pressure and high- pressure baroreceptor reflexes. The
low-pressure baroreceptors reflex is "designed" to maintain blood volume. They are
found in the large veins and in the atrial walls, whereas the high-pressure reflex is
"designed" to maintain systemic arterial pressure. Thus the benefit of these two
biological control systems is to maintain circulation with adequate pressures despite
perturbing forces. The atria baroreceptors are of two kinds; type A located at the entrance
of the pulmonary veins, and type B, which has its activation increased during the atria
filling phase (stretching fibers).
9
Definition of High Pressure Baroreceptor
The biological control system (Figure 2) constituting the high pressure
baroreceptors which regulate/maintain systemic arterial pressure is comprised of ( 1) a
level detector [which monitors the level of the variable (systemic arterial pressure) to be
controlled], (2) the integrator which compares the level of the systemic arterial pressure
to the "desired" level or set point, and (3) the controllers which return the perturbed
systemic arterial pressure back to the desired level. These three components of the
biological control system "communicate" with neurohwnoral signals. The set point for
systemic
arterial
pressure
is
approximately
http://www.cvphysiology.com/Blood%20Pressure/BPOI2.htm),
70
mmHg
(Internet
source:
the integrator is a neural network
located in the medulla oblongata, the controllers are the heart (by changing rate and
contractility) and systemic arterioles (by changing degree of constriction or dilatation),
and the level detectors are coils of cells located in the carotid sinus and aortic arch. The
level detectors communicate to the medulla oblongata by sending afferent volleys over
the vagus and glossopharyngeal nerves (Figure 3). The medulla communicates to the
controllers by sending efferent volleys to the heart and blood vessels. Buffering of a
reflex involving the carotid sinus occurs when effects of changing systemic arterial
pressure may influence baroreceptors other than those in the carotid sinus (Triedman,
1994). For example, during head-up tilt, the baroreceptors in the carotid sinus are
gravitationally above the level of the heart and pressure within falls proportional with the
weight of the column of blood between the heart and the baroreceptors (Figure 4).
10
On the other hand, pressures at the high pressure baroreceptors in the aortic sinus
and in other points of the systemic arterial tree located in the abdomen (below the heart)
may not change (for the aortic receptors) or may actually increase (for abdominal
receptors) because the heights of the columns of fluid between the heart and the
abdominal baroreceptors change but in a direction opposite to those above the heart.
11
Biological Control S~stem
Set
150
ml/kg/min
1.5 ml/kg
100 mmHg
7% ofBW
Controlled
co
t------.--
sv
PAo
BV
1.Level
JGA
Mech. Rec.(LV)
,_____________ HPBR (CS+AS)
vagus
glossopharyngeal
LPBR (LA)
Figure 2: Schema showing the biological control system. (1) level detector [which
monitors the level of the variable (systemic arterial pressure) to be controlled], (2) the
integrator which compares the level of the systemic arterial pressure to the "desired"
level or set point, and (3) the controllers which return the perturbed systemic arterial
pressure back to the desired level. JGA= Juxtaglomerular aparatus, Mech. Rec=
mechanical receptors, HPBR = high-pressure baroreceptors, LPBR= low pressure
baroreceptor, symp= sympathetic, art= artery, SAN= sino-atrial node, CO= cardiac
output, SV= stroke volume, PAo = aortic pressure, BV= blood volume, LA= left
atrium, CS= carotid sinus, AS= aortic sinus, LV= left ventricle. (Courtesy ofR.L. Hamlin)
12
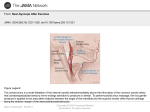
Figure 3: Schematic drawing showing both the carotid and aortic sinus enervation and
anatomy. The carotid (in the carotid body) and aortic sinus communicate to the
medulla oblongata by the glossopharyngeal and vagus nerves, respectively. It shows
the carotid and aortic sinus localization relative to the medulla oblongata and the heart.
Carotid body consists of carotid barorec'-Jors and chemoreceptors. (Taken from
internet)
15 cm blood
150mm/12.9
15 mmHg
=
·...
..
..
..
..
Figure 4: Schema showing the weight of the column of blood. Forcing ofbaroreceptor
during head-up tilt, the decrease in baroreceptor loading is alwavs equal to the weight
of blood in a vertical column from the receptor to the heart. It remains constant for a
given dog for all tilts. (Courtesy ofR.L. Hamlin)
14
Thus it is possible that during head-up tilt in which decrease in pressure unloading
the carotid baroreceptors is equal to but opposite in sign to that of the carotid, and if both
receptors have equal influence (i.e. gain) there may be no net effect.
However it is well known that the gain of the high- pressure baroreceptors in the
carotid sinuses is similar to those in the aortic sinus (Hainsworth,
1970~
Daly, 1926}-but
may be buffered by-pressure changes at other baroreceptors.
Morphine
Anesthesia with morphine-chloralose is considered best for studying neural
control of the cardiovascular system. It is minimally cardio-depressant and permits
normal sympathetic outflow, while exaggerating slightly the parasympathetic arm of the
autonomic nervous system. A disadvantage is that it requires use of a controlled
substance (morphine). Morphine (Figure 5) is used most often as the sulfate. It binds toµ
more than to
o
or
K
receptors, and produces analgesia, drowsiness, and both
psychological and respiratory depression. Unless administration is extremely slow,
morphine produces vomiting. Morphine has no major cardiovascular effects except, when
large dose are given, there is cardio-deceleration and systemic arterial hypotension
resulting from its parasympathomimetic activity. Morphine is distributed uniformly
within the body, is minimally lipophillic compared to other opioids, and only a small
percentage crosses the blood-brain barrier. Morphine undergoes glucuronidation in the
liver principally to morphine-6-glucouronide-a highly active analgesic. Excretion is
primarily in the urine and minimally in the bile. The biological half-life is 4 to 6 hours.
15
Alpha Chloralose
Alpha-chloralose (Figure 5) is an agent that produces minimal analgesia, therefore
must be used with an analgesic if potentially painful stimuli are anticipated. Alpha
chloralose is considered an appropriate agent (i.e., produces sufficient analgesia) for
catheter insertions (Katona et al, 1970), suturing, and even minor abdominal surgery. A
1% solution is made by dissolving the compound in water heated to 60 degrees Celsius
(Van Citters et al, 1964). Before injecting however, it is cooled to 40 degrees Celsius.
Alternately, a more concentrated solution of alpha chloralose may be made by dissolving
it in a 10% aqueous solution of polyethylene glycol heated to 60 degrees Celsius, and
then may be cooled to 40 degrees Celsius for administration. Because its soporific action
requires approximately 15 minutes to develop, a pre-anesthetic or a short-acting
anesthetic must be given before chloralose. Dogs anesthetized with alpha chloralose
frequently manifest hyperreflexia (Van Citters et al, 1964) with jactitations, particularly
in response to sudden sounds. One hundred mg/kg of chloralose is given as rapidly as
possible as a bolus, after which a constant infusion of 50 to 75 mg/kg/hour (Shubrooks Jr.
SJ, 1972) is given to sustain surgical anesthesia. In contradistinction to the profound
depressing effects on halothane and sodium pentobarbital on receptor function, alpha
chloralose has little such depression (Halliwill et al, 1992). Van Citters and colleagues
16
( 1964) found that after two hours both the level of pressure and the individual waveforms
were indistinguishable from control values. It is said that less than surgical anesthesia is
produced in dogs, and that respiratory support should be available because of respiratory
depression.
17
HO
__...-Me
HO
H
HO--.....- -
Cl
o-....~11c1
r
H
Cl
Figure 5: Chemical structure. Morphine chemical structure on the top, and
alpha-chloralose Chemical structure on the bottom of the figure.
18
Because induction with alpha -chloralose may produce violent behavior (this may
be caused by contamination of the alpha chloralose with beta chloralose), either an opiate
(e.g., morphine) or a short-acting anesthetic (e.g., thiopental or methohexital sodium) is
usually given before initiation of alpha chloralose. After administration of a bolus
injection of 80 mg/kg, supplemental doses of up to 50% of the bolus dose per hour could
be given without altering hemodynamics. Doses of alpha chloralose greater than 280
mg/kg over 2 hours produced depression of left ventricular peak systolic pressure and
aortic pulse pressure, which produced death after 6 hours. There is abundant information
about long-term anesthesia/restraint with alpha chloralose, but little in information about
repeated anesthesia/restraint with the agent. Alpha chloralose did not depress
cardiovascular function in dogs anesthetized with it for 3 hours or more. Beagle puppies
given repeated chemical restraint with alpha chloralose after induction of anesthesia with
thiopental, did not manifest seizures, or behavioral or growth abnormalities.
The general effects of chloralose on the cardiovascular system are controversial
and not well understood. Comparison reveals that the reflex rise in the heart rate is
greater in the chloralose-anesthetized dog (+ 35 beats/min) (Berkowitz et al, 1969;
Delaunois et al, 1967; De Vleeschhouwer et al, 1967; Feigl, 1968; Thames et al, 1970;
Wang et al, 1970) than in the pentobarbital-anesthetized dog(+ 11 beats/min) (Bond et al,
1969; Constantine et al, 1971; Iriuchijima et al, 1968). However, others (DucheneMarullaz et al, 1682) found that the heart rate might be depressed (- 10 beats/min).
19
Parameters Expressing High Pressure Baroreceptor Function
Overall
Numerous authors have studied the static stimulus-response curve relating mean
systolic blood pressure to mean carotid sinus pressure (Donald, 1971; Sagawa, 1965;
Scher AM, 1969). The curve is sigmoid in shape and may be defined by three
characteristics: 1) the pressure at the threshold, 2) the pressure at the saturation level, and
3) the pressure at the point of maximal sensitivity. Anesthetized dog presented the
following values: threshold pressure, 45-70 mmHg; saturation pressure, 170-200 mmHg;
and the pressure at the point of maximal sensitivity, 120-140 mmHg (Donald, 1971,
Sagawa, 1965, Stegemann 1969).
In regards to the aortic arch baroreceptors, various studies agree very well that the
characteristic pressure levels were clearly higher than for the carotid sinus baroreceptors,
which is contradiction to those by Hainsworth (1970) and Daly (1926). This finding is
reflected in a general displacement of the aortic stimulus-response curve to the right of
the curve for the carotid sinuses (Donald, 1971). A comparison of the static stimulusresponse curves (James and Daly, 1970) between the carotid and aortic arch sinuses,
demonstrated that the reflex reduction in systemic vascular resistance produced by a rise
in mean carotid sinus was greater than in the aortic arch sinus. Despite these observations
concerning the aortic arch, there is no satisfactory explanation for these differences.
20
Threshold
The threshold of the baroreceptors reflex is determined by at what systemic
arterial pressure the baroreceptor reflex first occurs (Kirchheim, 1976), i.e., there is a
compensatory change in heart rate (Figure 6). This is also termed the sensitivity. When
blood pressure increases or decreases from a level of 200 mmHg, there is no change in
heart rate and no return in blood pressure toward normal. However from a level of 160
mmHg, heart rate does change and the blood pressure returns (albeit imperfectly) towards
normal. Thus the threshold is 160 mmHg.
Set Point
The set point of the baroreceptor reflex is that level of blood pressure at which an
increase in blood pressure will decrease the sympathetic tone and produce bradycardia
and a decrease in blood pressure will cause an increase in sympathetic tone resulting in
tachycardia. In both circumstances the compensatory response tends to restore the blood
pressure toward the desired set point.
Saturation Point
The saturation point of the baroreceptors reflex is determined by at what systemic
arterial pressure there is no further change in heart rate or systemic arterial pressure
(Kirchheim, 1976), (Figure 6).
21
The open-loop gain (Figure 7) of the high-pressure baroreceptors is defined as the
ratio of the return of blood pressure toward normal to the distortion imposed. That is, if
normal pressure were 100 mmHg, if a perturbing force (say hemorrhage) decreased it to
60 mmHg, and if the biological control system returned the pressure to 85 mmHg (i.e.,
not all the back to normal), the open-loop gain would be the amount of return (i.e., 25
mmHg) divided by the difference between the level to which it returned and the normal
value (i.e., 15 mmHg). The open-loop gain would be 1.67. If the pressure returned back
to normal, the open loop gain would be infinite, since the return would be divided by 0. If
the pressure did not return at all, the open-loop gain would be 0. Another expression of
baroreceptors gain is the ratio of change in heart rate to change in systemic arterial
pressure (Abrahamsson, 2003), since change in heart rate is one of the two mechanisms
(change in vascular resistance being the other) responsible for return of systemic arterial
pressure.
22
HR
\
\
\
.........................-r.-,__., •
~
•••••••••
SP
A HR
A SAP
t
\
\
\
TH
'-----------------------SAP
Figure 6: Saturation point and threshold. Plot showing the saturation point at in which
there is no further change in heart rate or systemic arterial pressure. SAP= systemic
arterial pressure, TH= threshold, HR= heart rate, SP= saturation point.
23
A
100
B
c
-wllr/tWliilliliilWliillllli---------.._--_.------ }
85
Recovery=
25mmHg
Pressure
(mmHg)
60
Perturbing
force
Gain = 25
15
Difference to
normal = 15mmHg
= 1.67
w..a...&..11a....-.-.••···················
Time(sec)
,,Hemonbage
Figure 7: Show the baroreceptor gain due to any perturbing force in the blood
pressure. The normal pressure is 100 mmHg, a perturbing force (hemorrhage)
decreased it to 60 mmHg, and the biological control system returned the pressure to 85
mmHg (i.e., not all back to nonnal), the open-loop gain is the amount of return (i.e.,
25 mmHg) divided by the difference between the level to which it returned and the
normal value (i.e., 15 mmHg). The open-loop gain is 1.67. A, B, C are different point
in time at which the arterial blood pressure bounces until it returns to stability again.
(Courtesy of R. L. Hamlin)
24
The most common expression of the gain is the ratio of change in heart rate to
change in mean systemic arterial pressure that occurs at a pressure midway between the
threshold and point of saturation when the relationship is nearly linear and ratio is
maximum.
Tau is expressed, usually, as the time-constant. The time-constant is defined as
the time required for the response to achieve 63.3% (approximately 2/3rds) of the new
steady state (Figure 8) (Burke and Irvin, 1979). A response with a short time-constant is
rapid; one with a long time-constant is slow. If the time-constant is long, the system is
described as one that is over-damped; i.e., it takes too long to return the level of the
controlled variable to the new steady state.
Ripple Factor
The value of a controlled variable oscillates around a mean, and this produces a
rippled appearance to the value of the controlled variable. That is it first exceeds the
mean, then is lower than the mean, then exceeds it, then is lower ... and so on. The
magnitude of the oscillations is the ripple factor.
25
Damping
If a biological control system is under-damped, the value of the perturbed
controlled variable returns toward normal. If it does so promptly and without
overshooting the new steady state, it is termed critically damped.
If it overshoots the mark and oscillates toward the mean, it is termed under-
damped. If it moves too slowly toward the mean it is considered to be over-damped
(Figure 9). The desirable biological control systems have a short tau, it is critically
damped (i.e., it returns quickly but does not overshoot) and the gain will be infinite (i.e.,
the controlled variable returns to normal (Triedman, 1994).
26
A
B
c
100 _ _ _ _ _ _ _ _ _ _ _ _ _..__ __._ _....._ _ }
Differenceto
nonnal = 15mmHg
85
•••••••••
Pressure
(mmHg)
Recovery = 25
mmHg
60
••••••
•~························
Tau
II'.•
Time (sec)
•
•
:...
Perturbing
force
Figure 8: Show the baroreceptor gain due to any perturbing force in the blood
pressure. The normal pressure is I 00 mmHg, a perturbing force (hemorrhage)
decreased it to 60 mmHg, and the biological control system returned the pressure
to 85 mmHg (i.e., not all the back to normal), the open-loop gain is the amount of
return (i.e., 25 mmHg) divided by the difference between the level to which it
returned and the normal value (i.e., 15 mmHg). A, B, Care different point in time
at which the arterial blood pressure bounces until it return to stability again. Tau is
the time constant. The time-constant is the time required for the response to
achieve 63.3% (approximately 2/3rds) of the new steady state. (Courtesy ofR. L.
Hamlin)
27
100
85
3. Over damped
2. Critically damped
'
'&
1. Under damped
60
Time (sec)
Perturbing
force
l~morrhage
Figure 9: Show the damping effect of the baroreceptor response to a perturbing
force in the blood pressure. The nonnal pressure is 100 mmHg, a perturbing force
(hemorrhage) decreased it to 60 mmHg, and the biological control system returns
the pressure to around 85 mmHg. The three (3) damping effects are shown.
1. under-damped, blood pressure returns toward nonnal; 2. critically damped,
pressure returns promptly and without overshooting the new steady state; 3. underdamped, it overshoots the mark and oscillates too slowly toward the mean. The
desirable biological control systems have a short Tau, it is critically damped.
(Courtesy of R. L. Hamlin)
28
Physiology and Pathophysiology
In heart failure
One of the distinguishing features of heart failure is a reduction in
parasympathetic efferent activity, an increase in sympathetic efferent activity both of
which either reduce or abolish respiratory sinus arrhythmia. It is thought that the
following sequence is responsible (Weber, 2001; Wang 1992; Sisson, 2004):
1.
reduction in cardiac output leads to reduction in renal plasma flow and delivery of
sodium to the juxtaglomerular apparatus (JGA);
2.
the JGA releases rennin;
3.
rennin activates angiotensinogen to form angiotensin-1;
4.
angiotensin-1 is converted to angiotensin-11 by the angiotensin converting enzyme,
chymases, cathepsin G, elastase, tissue plasminogen, and chymostatin-sensitive
All-generating enzyme (CAGE) (Sisson, 2004);
5.
angiotensin-11 loads the high pressure baroreceptors with sodium-potassium
ATPase;
6.
ATPase causes the high pressure baroreceptors to interpret the existing systemic
arterial pressure as too low and decreases the number of afferent volleys traveling
to the medulla oblongata;
29
7.
the medulla oblongata responds to "mis-information" that blood pressure is too
low
by
producing
vasoconstriction
(increasing
both
preload
due
to
venoconstriction and afterload by arterial and arteriolar constriction, and by
increasing heart rate by reducing vagal efferent activity and increasing
sympathetic efferent activity.
In fact the severity of heart failure can be semi-quantified by the degree of
reduction in respiratory sinus arrhythmia, and, since there is a reduction in
parasympathetic efferent activity, there is a similar reduction in baroreceptor function
(Berne and Levy, 1972).
Vasovagal syncope
When the left ventricular mechanoreceptors are overly sensitive and systemic
arterial pressure falls even slightly as might occur during postural changes, the ventricle
begins to contract more vigorously in response to the reduction in after-load (Hamlin,
1972). The increase in ventricular wall motion over-stimulates the mechanoreceptors,
which "report" to the medulla oblongata that the ventricle is heaving wildly. The medulla
interprets this as elevation of systemic arterial pressure, and responds by reducing the
heart rate by increasing vagal tone and by vasodilatation-both of which should lower
the arterial pressure. Thus the baroreceptors reflex is activated spuriously and results in a
precipitous fall in systemic arterial pressure reduced cerebral perfusion, and syncope.
Vasovagal syncope was first reported in miniature schnauzers by Hamlin in 1972
(Jochman-Edwards, 2002).
30
In response to drugs
Therapeutic agents may affect systemic arterial pressure by altering preload (the
venous return) or afterload (the interference "perceived" by the left ventricle to ejection)
(Salgado and Krieger, 1988).
Both may be caused by drug-induced alterations of smooth muscle tone in the
vasculature, or they may result from drug-induced alterations in baroreceptor sensitivity
and/or gain (Cowley, 1984). This is particularly important because of the ubiquitous use
of known vasoactive drugs (e.g., drugs used for erectile dysfunction, anti-hypertensives,
and diuretics). For example, a diuretic may produce venodilatation and reduce preload
and/or produce arteriolar dilatation and decrease afterload. Both might result in reduction
of systemic arterial pressure and syncope if not countered by the baroreceptors reflex.
Methods of study
Oxford
The baroreceptors reflex is elicited commonly by administering graded doses of
vasoactive compounds, which either elevate (e.g., phenylephrine) or reduce (e.g., sodium
nitroprusside) systemic arterial pressure by their effects on smooth muscle in systemic
arterioles (Davies, 1999; Smyth, 1969). The heart rate response (Figure 10) and/or the
firing rate of efferent nerves (Figure 11) to blood vessels are/is used as the dependent
variable(s); the independent variable being the change in systemic arterial pressure.
From the plot of heart rate or intensity of efferent nervous firing versus systemic
arterial pressure, all parameters (i.e., sensitivity, gain) of baroreceptor function can be
obtained. The problem with this methodology is that the drugs use to affect systemic
31
arterial pressure may also affect, directly, baroreceptor function.
Furthermore, if the
carotid sinus receptors are activated, say by a drug-induced increase in systemic arteriolar
vasoconstriction, then although the heart rate response will be appropriate (that is will
decrease) the appropriate increase in systemic vascular resistance will be blunted or
abolished because the vessels are already constricted.
32
.... , ...................... ..
I
j.
''
I
,~
RESP
130
--
HR
30
aso
BP
Figure 10: Example of decrease in heart rate response to increase in pressure produced
by phenilphrine, on the left. Example of increase in heart rate in response to decrease in
pressure produced by nitroprusside, on the right.
Examples taken from Goldstein et al (1982), Circulation 66:436
33
so
f
7
I
I
I
1111
111
11111
1111
I
111111111
1111111111
11111111
1111111
I
11111111111111
11111111111111
111111111111111
1111111
I
I
CL
1
I
200
0
II
1111111111111111111111111111111111111111 II lllll II 111111111111111111111111111111111
.5
1.0
t.5
2.0
Time-sec.
Figure 11: Example of the relationship of phasic aortic blood pressure to the firing of a
single afferent nerve fiber from the carotid sinus at different levels of mean arterial
pressure. From Berne RM and Levy MN.
Cardiovascular Physiology , St Louis:
Mosby. Page 133, 1972.
34
Baroreceptor function may be activated by changing the degree of stretch on the
carotid sinus by either a head-down or a head-up tilt (Baum et al, 1981; Bedford et al,
1988; Honda et al, 1993, Froget et al 2004) (Figure 12). The subject is placed on a
board, and systemic arterial pressure and heart rate are measured. The board is then tilted
so that the carotid sinus is either above (head-up tilt) or below (head-down tilt) the level
of the heart. It is conventional to perform tilts of approximately 70 degrees (Schwartz DS,
2000 ). The forcing on the baroreceptors then is proportional to the vertical height
between the carotid sinus and heart. This explores only the contribution of the carotid
sinus, since the change in vertical height between the aortic sinus and the heart would
change trivially. However, since the position of the aortic sinus with respect to both the
heart and the carotid sinus, is different, the net effect of a positive tilt, which replaces
only the carotid sinus may be buffered by the absence or opposite effects on the aortic
smus.
The tilt method is performed simply (Figure 12), and evaluates the baroreceptors reflex
in response to natural, i.e., physiological, stimulation. The negative features of this
methodology are ( 1) there is deactivation of thoracic cardio-pulmonary receptors by
pooling of blood in the pelvic quarters and thus decreasing venous return, (2)
psychological and/or vestibular stimulation may modify the reflex. The latter can be
prevented if lower-body negative pressure is applied to produce venous pooling without
postural change (Parati et al, 2000). It is important to appreciate that the change in heart
rate produce by unloading of the carotid baroreceptor must be made immediately-within
35
seconds-after the tilt (Borst et al, 1982; Ewing et al, 1980; Lida, 1999) because the
unloading due to hydrostatic effects occurs instantly, and after some time
vasoconstriction throughout the body and venous pooling in the dependent portion of the
torso result in altered physiology not necessarily due to the unloading.
B
fl
I/
Head-up tilt
Head-down tilt
Figure 11 : Head-up and head-down tilt. Drawing shows a dog in dorsal
recumbence (A). Tilt with the head-up forming a 70 degree angle with the
horizontal, and tilt with the head-down forming a 70 degree angle with the
horizontal (B). (Courtesy of Tim Vojt)
36
Neck Suction
By applying suction over the neck with "neck chamber device" (Dwain, 1980;
Eckeberg et al, 1975; Ludbrook et al, 1977; Mancia et al, 1983; Parati et al, 2000;
Schwartz DS, 2000), the negative pressure is transmitted to the carotid sinus, thus
expanding it, increasing the tension in the wall, and activating the high- pressure
baroreceptors resulting in cardio-deceleration and vasodilatation. This method is possibly
the best to utilize, since it requires giving no drugs, it stimulates only the carotid sinus,
and it does not alter baroreceptor function (as with the Oxford method). This method has
been used in space flight to interrogate the effects of zero gravity on baroreceptors
function. The disadvantages are that it requires specialized instrumentation and a formfitting cuff to surround the neck.
37
CHAPTERJ
MATERIALS AND MEIBODS
Protocol Approval
This study was conducted following approval by the ILACUC of The Ohio State
University, with protocol number 2004A0059.
Animals
Seven large hound-type dogs (average weight 20 kg) and 3 beagle-hounds
(average weight 11 kg) were determined to be healthy based upon their appearance, feed
consumption, absence of fever, and absence of murmur or abnormal breath sounds. All
dogs were intact males. Based upon dentition they ranged between 1 and 3 years of age.
Dogs had been fully vaccinated and were free of internal and external parasites.
Anesthesia
All dogs were given, N, morphine sulfate (Elkins-Sinn, NJ) (1.5 mg/kg) as a preanesthetic. They were then given, N as a bolus, alpha chloralose (Sigma Chemical Co, St
38
Louis, MO) (100 mg/kg), after which they received a continuous infusion of alpha
chloralose (30 to 40 mg/kg/hour) to sustain anesthesia.
Animals were ventilated with room air at a rate (usually 12/minute) and a tidal
volume (usually 12.5 ml/kg) to sustain systemic arterial PaC02 of approximately
40mmHg using a fix-volume respirator (Respirator pump, Model 613, Harvard Apparatus
Co. Inc. Millis, Mass.). The dogs were placed on heating pads (Heat Therapy Pump
Model TP-500, Gaymar Industries, Inc., Orchard Park, NY) to sustain body temperature
(37.0 ± 0.5°C).
Surgical preparations/Instrumentation:
To measure the pressure within the
carotid sinus, a fluid-filled catheter, attached to a pressure transducer (RS104A, Biopac
Systems, Inc., Santa Barbara, CA), was advanced retrogradely via the lingual branch of
the external carotid artery into the region of the carotid sinus for 4 dogs. "Head motion in
the vertical axis was measured by taping the open tip of a catheter filled with 0.9% saline
to the skin overlying the wing of the atlas, which approximates the position of the carotid
sinus in both the caudal-cephalic and the ventral-dorsal axes'', (Lamberti et al, 1968). To
measure systemic arterial pressure a fluid-filled catheter attached to a pressure transducer
was advanced through a femoral artery into the region of the junction of the ascending
aorta with the arch for 4 dogs. Electrodes (V7305 ECG electrodes, Tyco Healthcare
Group LP, Mansfield, MA 002048, USA) forming ECG leads I and II were attached to
all.
39
Recording
Recordings of the 2 lead ECG and pressures from the regions of the carotid sinus
and aortic arch were made on a Biopac MPlOO Data Acquisition System (Biopac, MPlOO
Software, Biopac Systems Inc, Santa Barbara, CA), with a sampling rate to 2 kHz and
frequency response flat to 150 Hz.
Experimental Protocol
Six dogs were studied 3 times with 48 hours between studies. Each time, the dogs
were studied 3 times with 30 minutes in between. They were place in dorsal recumbence
on a V-shaped board. Their limbs were attached to the board so that the dogs could not
slide, and so that the change in posture did not produce tension in the limbs that might
have altered redistribution of blood and affected the baroreceptor reflex. After baseline
measurements of pressures (4 dogs) and ECG's (6 dogs) were made for 30 seconds, dogs
were tilted within <lsecond to a head-up-position. The angle between the board and the
horizontal was approximately 70 degrees (Figure 12). This head-up tilt was maintained
for 20 seconds, after which the dogs were returned to the horizontal. Measurements of
pressures (4 dogs) and ECG's (6 dogs) were made the entire time. The vertical distances
between the level of the carotid sinus and the heart was measured with a centimeter ruler
(Table 1). The vertical height was used to calculate the unloading of the carotid sinus
40
high-pressure baroreceptors as follows. The height was converted to millimeters, and the
number in millimeters was then, divided by 12.9 (the ratio of the density of mercury
[13.6] to blood [12.9]) (Ageyama et al, 2001), to obtain the negative pressure to which
the carotid sinus should have been exposed during the tilt.
Dog JD
Length from carotid
sinus to heart (mm)
200
210
230
190
180
200
201
Baby
George
Happy
Houston
Igor
Kato
AVG
Table 1: Showing the measurements of the vertical distances between the level of the
carotid sinus and the heart. The measures were taken with a centimeter ruler. The
average (AVG) of the 6 dogs is shown.
Four dogs with cannulation, of the carotid sinus and aortic arch (Figure 13) were
exposed once, to both head-up and head-down tilts (Figure 12).
41
Artertal
OrA~SlH9
transducer
Figure 13: Showing a cut down in the neck for the insertion of a catheter into the carotid
sinus region. The catheter was connected to the arterial pressure transducer. The
nressures in the carotid sinus (shown ahove) and the aortic sinus were then recorded
42
The head-up tilt was performed precisely as described previously, and the head-down tilt
was performed as follows. Twenty seconds after the dog had been laid flat after the head-
up tilt, the board was inclined to approximately 70 degrees so that there was a head-down
tilt, i.e., the carotid sinus high pressure baroreceptors were subjected to an increased load.
This was sustained for 20 seconds, after which the dog was returned to the horizontal. As
before, pressures and ECG's were recorded continuously.
Blood chemistry
Venous blood samples (5 ml) were obtained before the first anesthetic episode
and again immediately before the last anesthetic episode. A sample was not obtained after
the last anesthetic episode because the anesthesia produces significant hemodilution and
would distort the findings. A CBC (RBC, WBC, differential, platelets, hemoglobin, PCV)
and clinical biochemical profile (ALT, AST, AP, creatinine, urea nitrogen) (Table 2 and
2) were performed in the clinical laboratory of the Ohio State University Veterinary
Teaching Hospital.
Necropsy/histology
Immediately following euthanasia with pentobarbital sodium, a post mortem
examination was conducted to retrieve tissues from all vital organs (Table 4). Tissues
were placed in 10% buffered formalin, and after suitable duration for fixation, 4 u
sections were collected and stained with eosin methylene blue. These tissues were
43
analyzed under the supervision of a board certified veterinary pathologist. The histology
of these tissues was compared to comparable tissues from known, normal dogs.
44
Chemistrya
Urea nitrogen
Creatinine
Phosphorus
Calcium
Na
K
Cl
Anion Gap
Serum Osmolarity
Bicarbonate
ALT
AST
AlKPhos
ALP/CAP
CK
Cholesterol
Bilirrubin Total
Total protein
Albumin
Globulins
Albumin/ Globulin
ratio
glucose
Lipemic index
Hemolytic index
lcteric Index
Blood Count
Plasma Protein
Packed Cell Volume
Hemoglobin
Red Blood Cells
MCV
Baby
George
Happy
Houston
Kato
Igor
16
0.9
4.2
11.2
146
4.3
110
17.6
292
22.7
24
18
28
1
75
169
20.1
6.7
3.7
3.0
1.2
14
0.9
5.1
11
146
4.2
111
17.9
291
21.3
36
15
37
2
86
168
0.10
8.2
3
5.2
0.6
21
1.2
5.4
11.2
150
4.4
111
20.5
300
22.9
23
21
33
2
121
166
0.10
7.7
3.5
4.2
0.8
15
1.1
5.8
10.8
151
5.3
114
24.6
300
17.7
28
27
58
4
207
213
0.14
6.4
4
2.4
1.7
17
1.2
5.5
10.7
151
4
116
21.5
301
17.5
179
136
68
2
87
152
0.1
6
3.4
2.6
1.3
105
7
4
0
94
5
9
0
85
13
10
0
78
15
105
0
95
6
3
0
6.9
44
15.4
6.77
65
8
41
13.6
6.89
60
8.2
42
14.3
6.59
64
7.4
45
16.3
6.52
69
8.5
46
15.8
6.6
69
34.7
34.1
36.2
34.6
MCHC
33
RDW
16.4
17.1
16.4
14.7
16.8
Nucleated Cells
8.3
12.3
12.1
6.58
7.56
1
Nucleated RBC's (%)
Band Neutrophils
0.4 (6)
4.6 (55)
6.5 (53)
6.2(51)
2.9(44)
4.9 (65)
Seg Neutrophils
Lymphocytes
2 (24)
3.3 (27)
3.5 (29)
2.5 (38)
1.9 (25)
Monocytes
0.3 (3)
6 (0.7)
0.4 (3)
0.5 (7)
0.6 (8)
Eosinophils
1.4 (17)
1.7 (14)
1.9 (16)
0.3 (5)
0.2 (2)
Leukocyte
Reactive
Reactive
lymphocytes lymphocytes
Morphology
197,000
426,000
255,000
272,000
Platelet Count
251,000
Platelet Evaluation
adequate
adequate
adequate
adequate
adequate
a Chemical analyzes of blood components, 6 Blood counting analyzes showing different types of cells.
Table 2: Blood sample collected before the first experiment on day 1. Showing the chemistry and the
profile analyses of blood from all dogs
45
Chemistry"
Urea nitrogen
Creatinine
Phosphorus
Calcium
Na
K
Cl
Anion Gap
Serum Osmolarity
Bicarbonate
ALT
AST
AlKPhos
ALP/CAP
CK
Cholesterol
Bilirrubin Total
Total protein
Albumin
Globulins
Albumin/ Globulin
ratio
glucose
Lipemic index
Hemolytic index
lcteric Index
Blood Count
Plasma Protein
Packed Cell Volume
Hemoglobin
Red Blood Cells
MCV
MCHC
RDW
Nucleated Cells
Nucleated RBC's (%)
Band Neutrophils
Seg Neutrophils
Lymphocytes
Monocytes
Eosinophils
Leukocyte
Morphology
Baby
George
23
0.9
4.7
11.3
151
4.8
109
24.4
303
22.4
44
22
33
2
103
180
0.1
6.9
3.9
3.0
1.3
15
1
4.4
11.1
147
4.6
110
22.9
294
18.7
31
14
38
2
85
205
<0.1
8.0
3.1
4.9
0.6
96
5
43
Happy
18
0.9
5.6
9.9
151
4.8
119
Houston
Igor
Kato
11
1.1
4.9
149
4.8
113
21.9
296
18.9
135
38
76
163
0.2
6.5
2.7
3.8
0.71
12
0.9
4.5
11.9
150
3.8
116
22.2
298
15.6
36
15
60
3
113
193
0.13
6.1
3.7
2.4
1.5
2
273
165
0.12
6.3
3.6
2.7
1.3
19
1.3
5.1
11.1
149
5.1
112
20.8
296
21.3
34
19
42
2
146
168
0.11
6.7
3.9
2.8
1.4
109
5
3
94
0
2
95
2
0
100
0
6
61
25
0
0
0
0
0
0
7
46.6
16.2
7.12
65.4
8.1
40.8
13.5
6.88
59.2
42
14
6.3
66.8
7.5
42
14.7
6
70
7.4
54
18.3
7.83
69
7.5
56
19.l
8.19
68
34.7
16.7
9.03
33.2
17
11.5
34.8
15.l
5.3
33.9
16.l
8.1
34.3
14.3
6.9
28
32
5
33.2
13.3
1(0.12)
5.9 (65)
6.6 (57)
4.82(39)
3.6(69)
4.5(55)
4.1(59)
2.1 (23)
3.0 (26)
4.82 39)
1.4(27)
2.3(28)
1.6(23)
0.5 (5)
0.6 (5)
0.62 (5)
0.1(3)
0.6(8)
0.7(10)
0.5 (6)
1.4 (12)
1.98(16)
0.05(1)
0.7(9)
0.6(8)
Reactive
Reactive
reactive
reactive
Norm
lymphocyt lymphocytes
lymphocyt lymphocyt
es
es
es
Platelet Count
283,000
198,000
275,000
278,000
222,000
Platelet Evaluation
ade9uate
ade9uate
adeguate
adeguate
ade9uate
ade9uate
8
Chemical analyzes of blood components, 6 Blood counting analyzes showing different types of cells.
Table 3: Blood sample collected before the last experiment, on day 3. Showing the chemistry and the
profile analyses of blood from all dogs
46
Dog ID
Organs
Kidneys
(Right and
left)
Adrenal glad.
(Right and
left)
Lungs
Heart 11vs,
Baby
Multifocal mininmal, NSF
subactue intersticial
nephrites,
lymphoplasmacytic
NSF
NSF
Multifocal, mild,
chronic,
lymphohysticytic,
peribronquites
NSF
LVFW, LA, RA)
Liver
Spleen
Stomach
Duodena
Pancreas
George
Moderate wide
spread congestion,
NSF
Wide spread mild
to moderate
eosinophilic,
lymphocytic
gastrites
NSF
NSF
Houston
Happy
Igor
Kato
NSF
NSF
NSF
NSF
NSF
NSF
Mild
NSF
lynphoplasmacytic ,
intersticial
agregates
NSF
IVS= focal eosinophilic
and histiocytic
myocardites with
eosinphylic abscess;
LVFW= multifocal minimal
lynphoplasmacytic
histiocytic and eosinophilic
and intersticial
myocardites
Focal chronic
Multrtocal mininmal
abscess, minimal to plasmacytic, eosinophilic
mild lynphoplasma portal hepatitis, unrelated
portal hepatitis.
to acute effects
Mild lymphoid
NSF
depletion related to
stress
NSF
NSF
NSF
NSF
NSF
NSF
NSF
NSF
NSF
Wide spread
congestion
NSF
NSF
NSF
NSF
NSF
Wide spread mild
eosinophilic and
lynphocytic
gastrites
NSF
NSF
NSF
NSF
NSF
NSF
Multifocal, mild to
moderate
eosinophilic and
NSF
NSF
NSF
NSF
Multifocal mild to
moderate subacute
lynphoplasmacytic,
intersticial nephrites
NSF
~mphoplasmacytic
NSF
NSF
NSF
NSF
NSF
NSF
Brain
Table 4: Hystopathology. Table is showing the vital organs and the main hystopathological findings in each of the "6
dogs" study grou2.
NSF= no significant findings; IVS= interventricular septum; LVFW= left ventricular free wall; LA= left atria; RA= right atria
47
Data analysis/statistics
Statistical analysis of the data (6 dogs)
Baseline heart rate and variability, within and across, days was addressed
statistically by analyzing the data with repeated measures model, using PROC MIXED in
SAS 9.1 (SAS Inst. Inc., Cary NC) (Littell et al, 1996). Time and day were included as
covariates and dog as a random effect in the model. Different covariance structures
(variance components,
1st
order autoregressive, compound symmetry and unstructured)
were tested: compound symmetry covariance structure fitted the data best and was used
in all the subsequent analyses to account for the correlated data structure.
To address maximum change between baseline and tilt, a new variable
"absolute_increase" was created. The variable was calculated as (maximum heart rate
during tilt - heart rate during baseline).
The change in heart rate between tilt and
recovery, a new variable "absolute_decrease" was created (maximum heart rate during
tilt
-
minimum
heart
rate
during
recovery).
Using
absolute_increase
and
absolute_decrease as outcome variables, data were analyzed similarly as for baseline
heart rate and variability, using PROC MIXED in SAS 9.1. Two different models were
run with both outcomes: first, only time and day were included as covariates (with dog as
a random effect) and second, with absolute increase as the outcome, the baseline heart
rate was included as a covariate and with absolute decrease as the outcome, the
maximum heart rate during tilt was used as a covariate.
48
These variables were included in the models to account for the variability among
subjects, days and times in the starting values from which either the increase or decrease
started. Interaction between day and time was also tested in each model.
How gain was calculated
For the 6 dogs whose pressures were not actually measured, two new variables
called "absolute_increase at 5 seconds" and "gain" were created by calculating the
change between the baseline heart rate and heart rate at 5 seconds (immediately after
tilting
before
effects
of venous
poling
would
be
important)
after tilting
("absolute_increase_5sec") and dividing this by 15 (the change in pressure calculated by
the change in position of the carotid sinus compared to the heart). The interest was to see
whether time or day significantly affected these measurements of gain.
Descriptive
statistics were run for both variables
To evaluate whether the variable "gain" was statistically associated with time and
day, repeated measures analysis using PROC MIXED in SAS 9.1 was performed. Time
and day were fixed effects and dog was included as a random effect in the model.
Similarly to the analysis done for "absulte_decrease", and absolute_increase, it had been
determined that compound symmetry covariance structure fitted the data best and thus, it
was used also in this analysis to account for the correlated observations within dogs.
For each outcome, pairwise comparisons were made between each day
and each time, using Tukey-Kramer adjustment for multiple comparisons.
49
Physiological Parameters
Instantaneous heart rate was calculated by dividing 60,000 (ms/minute) by the RR
(inter-beat) interval (ms). Pressures were recorded from the aortic arch and carotid sinus
in 4 dogs. In 6 dogs, only the instantaneous heart rate was calculated.
Measurements were made for 5 seconds epochs during 20 seconds before head-up
tilt, for 20 seconds during head-up tilt, and for 20 seconds after return to horizontal.
Three tilts were separated in time by 30 minutes. Each group of 3 tilts was separated by
48 hours. The change in heart rate produced by a tilt was the difference in heart rate
between the maximal value during the tilt and the average value for the 20 seconds before
the tilt. Means for 6 dogs were compared with each day and among the days to determine
how stable/repeatable the response was within a day and among days.
Carotid sinus and aortic pressures were measured (4 subjects) with dogs in the
horizontal and immediately after the dogs were tilted 70 degrees (Figure 12). The
differences in those pressures were calculated. The vertical distance between the carotid
sinus and the heart was measured using a cm ruler. The height between the carotid sinus
and the heart was converted to mm, and was divided by 12.9 (Ageyama et al, 2001}-the
ratio of the density of mercury (13.6) to blood (1.05). The means of the calculated and the
measured pressures were compared by a 2-tailed Student's t requiring a p<0.05 for
significance.
50
CHAPTER4
RESULTS
Tracings of heart rate during baseline, head-up tilt, return to baseline, head-down
tilt, and return to baseline are shown in figure 25.
Along the text graphs show the
relationship between baseline heart rate, absolute increase in heart rate (max - baseline)
when tilted, and absolute decrease in heart rate (max - min) during the experiment for
each of 3 episodes during each of 3 days. Mean values for the six subjects at each daytime combination are presented.
Although there were 48 hours between experimental days, the days are labeled as
1 (first day), 2 (second day), and 3 (third day). The times are labeled along the x-axis as
0, 30, and 60 minutes.
51
Baseline Heart rate
Figure 14 shows the mean baseline heart rate versus time for each experimental
day. From this graph, it appears that mean baseline heart rate decreases within each day
as time increases. It also appears that values on days 1 and 2 are very similar, but that
day 3 is usually lower than days 1 and 2.
There may be a time effect (rate drops consistently with time) and perhaps even an effect
of day (day 3 consistently lower than 1 and 2).
60
45
0
30
lime of experiment
60
Figure 14. Graph of mean baseline heart rate versus time for the 3 experimental days.
Symbols indicate experimental day.
52
George, batlellnl heartrate,
by day and time
Biby, blleellne heartrate
by day and time
65
65
60
55
60
55
50
50
45
45
40
35
40
30 60
0
30
eo
0
30
\
\
\
60
0 30 60
-
~
'-
"" --.
55
50
45
40
35
30
0
30 60
0
30
eo
65
.
55
50
30 60
0
0 30 60
..._
'
0
"a._
~
.
•
"-...
' ..
' """-
30 60
0
30
80
30
0
.
80
0
30
80
Kall>, baMUM '-rlnlle
by day and time
Igor, baseline heartrate
by day and time
60
~
Houston, bllaelne heartrate
by day and tine
Happy, baseline heartrate
by dly and time
65
60
.
\
35
30
30
0
\
.
06
~
- ---....
...............
eo
""' "-.,.
45
40
55
""" .
.
50
4S
40
35
3li
30
30
0
30
60
0
30
00
0
30
00
0
30
«>
0
30
«>
0
30
eo
Figure 15: Heart rate baseline for each dog on the 3 study days at the 3 times. Shows the
graphs that depict the changes in the baseline heart rate measurements for each individual
dog on the three times (0, 30 and 60) on the three study days.
53
As can be seen from figure 15, there is considerable amount of variability in the
baseline heart rate between dogs as well as within dogs. Happy, Houston and Igor have
higher heart rates to begin with on day 1 than Baby, George or Kato. Heart rate tends to
go down for some dogs (Baby, Kato) where as for some dogs it stays somewhat
consistent in some days
(Happy~
day 1 and 2, George and Igor day
2~
and Houston, day
3). For most dogs, the heart rate was not consistent from time to time within a day nor
was the pattern of change consistent from day to day.
Absolute Increase in Heart Rate
For each subject, day, and time combination, the absolute difference between
maximum heart rate and baseline heart rate was calculated.
Then, mean values for
absolute increase were calculated for each day and time. Figure 16 shows a graph of this
information. From this graph, it appears that the mean absolute increase becomes less as
time passes.
Also day 3 appears to differ from days 1 and 2 for the 0 minute
measurement, but day 1 seems to differ from days 2 and 3 at 30 minutes.
There appears to be an effect of time (heart rate increase becomes consistently
smaller as time increases) and that there is a day effect because of day 3 being lower than
the other 2 days at time 0.
54
20
€<U
Q)
:::c: 18
c:
Q)
th
<U
~
g 16
.!
::::>
0th
..0
<(
c:
14
<U
Q)
:?!
12
0
30
Time of experiment
60
Figure 16: Graph shows the mean absolute increase in heart rate versus time for the 3
experimental days. Symbols indicate experimental day.
Absolute Decrease in Heart Rate
For each subject, day, and time combination, the absolute difference between
maximum heart rate and minimum heart rate was calculated. Then, mean values for
absolute decrease were calculated for each day and time. Figure 17 shows a graph of this
information. From this graph, it appears as that the mean absolute decrease becomes less
55
as time passes. Again, there is a decreased magnitude of change as time passes. Also,
the responses at time 0 for all 3 days appear to be similar.
The 30 minute responses are very different for the 3 experimental days. The 60 minute
responses for days 1 and 2 are similar, but for day 3 are greater.
There appears to be a time effect (heart rate decrease becomes less for 30 and 60
minutes for days 2 and 3). There appears, also, to be a day effect, because at time 30, the
three days are quite different and at time 60, day 3 looks different from the other 2 days.
0
30
lime of experiment
60
Figure 17: Graph of mean absolute decrease in heart rate versus time for the 3
experimental days. Symbols indicate experimental day.
56
The summary statistics of the heart rate at baseline, at tilt and at recovery are presented in
Table 5.
Base Line
Day 1 Day2
Day3
Time
0
30
60
Tilt
Day 1
Day2
Day3
75.67
10.91
62.27
10.42
58.33
12.91
75.17
9.83
64.00
10.33
59.50
10.78
72.17
10.36
Recov
Day 1
Day2
Day3
55.00
8.22
47.33
7.99
45.17
9.19
51.83
10.71
43.00
3.69
38.67
6.86
Table 5: Means and Standard Deviations (in parenthesis) of the Heart Rate Measures at
time 0, 30, and 60 minutes During Day 1, Day 2, and Day 3
Absolute Change in Heart Rate
The mean of the increase of heart rate from baseline to tilt at time zero was 18.88
beats/min, 18.68 beats/min, and 15.53 beats/min during day one, day two and day three
respectively. When the measurement was made at 30 minutes the increase was 12.82,
14.19, and 14.19 beats/min during day 1, day2, and day 3 respectively. Lastly, the
measurement made at 60 minutes showed an absolute increase of the heart rate of 11.77,
12.09, and 12.29% during day 1, day 2, and day 3 respectively (Table 6).
On the other hand, the absolute decrease of the heart rate from tilt to recovery was
between 19.67 and 20.33 at time zero for day 1, day 2 and day 3 respectively (Table 6).
57
Time
minutes
0
30
60
Absolute Increase from
Base Line to Tilt
Dayl
Day2
Day3
18.88 6.41
12.82 5.74
11. 77 5.48
15.53 5.78
14.19 5.81
12.29 5.11
Absolute Decrease from
Tilt to Recove
Dayl
Day2
Day3
20.17 11.03
16.67 4.46
14.33 7.03
Table 6: Mean and Standard Deviation (SD, in parenthesis) of the Absolute Change of
The Heart Rate
Profile Plots and Qualitative Description of Heart rate Data
There are three sets of graphs presented that show the relationship between
baseline heart rate, absolute increase in heart rate (max - baseline) when tilted, and
absolute decrease in heart rate (max - min) during the experiment.
There were six
subjects in the study, with measurements made at 3 separate days and three times. Actual
values for the six subjects at each day-time combination are presented.
Although there were 48 hours between experimental days, the days are labeled as
I (first day), 2 (second day), and 3 (third day). The times are labeled along the x-axis as
0, 30, and 60 minutes.
Baseline Heart rate
Figure 18 shows the baseline heart rate versus time for each individual during
each experimental day; experimental days are displayed separately. From these graphs, it
appears as though baseline heart rate decreases within each day as time increases. This
58
effect is more consistent in Day 1 than in Day 2 or 3. It is difficult to identify a trend for
days.
day==1
day==2
70
60
E'
50
.e~
40
~
~ 30
-a::
:I:
Q)
c::
SJ
co
co
~
~
0
day==3
30
60
70
60
50
40
30
0
30
60
Ti me of experiment
Figure 18: Graph of baseline heart rate versus time for the 3 experimental days.
Numeric symbols indicate subjects; consecutive measurements on subjects are connected.
Absolute Increase in Heart Rate
For each subject, day, and time combination, the absolute difference between
maximum heart rate and baseline heart rate was calculated.
59
These values for absolute increase were graphed against time. Figure 2 shows a graph of
this information for each day.
Figure 19 offers some challenges for interpretation. It appears looking at data for
day 1 that, although increase varies among subjects, their responses are consistent over
time; however there are contradictions.
For example, Subject 2 consistently shows about a 10 bpm increase over 3 measures in
day 1. In day 2, subject 2's response is still about 10 bpm, but decreases over time. In
day 3, subject 2 has increases of around 20 bpm at 0 and 30 minutes (quite different from
similar measures made at days 1 and 2), but a 5 bpm increase at time 60 on day 3. Thus,
variability in the response appears to change with time and day.
60
day==2
day==1
40
30
20
10
0
c:
0
-~,
.c
<'O
~
0
day==3
30
60
40
30
20
10
0
~
0
60
30
lime of experiment
Figure 19: Graph of absolute increase in heart rate versus time for the 3 experimental
days. Symbols indicate subject identification numbers; days are plotted separately.
Absolute Decrease in Heart Rate
For each subject, day, and time combination, the absolute difference between
maximum heart rate and minimum heart rate was calculated. Then, values for absolute
decrease were plotted against time for each day.
Figure 20 shows a graph of this
infonnation. Again, responses appear to be rather variable.
61
On day 1, 4 subjects appear to have a reduced response at time 30 compared to time 0,
but little change from time 30 to 60; 2 subjects follow a different pattern. Days 2 and 3
have little evidence of specific patterns to the data - the absence of a pattern, though,
does not indicate that the response is consistent over day and time. In fact, it appears as if
there is some inconsistency in how subjects respond.
day==2
day==1
40
30
20
10
~
0
'01
i"'
~s!
0
day==3
30
60
40
30
20
10
~
0
0
30
60
lime of experiment
Figure 20: Graph of absolute decrease in heart rate versus time for the 3 experimental
days. Symbols indicate subject identification; consecutive measures are connected by
lines.
62
Statistical analysis of the results
Baseline heart rate
In agreement with the graphical presentation and descriptive statistics of the data,
both time and day were statistically significantly associated with the baseline heart rate in
the repeated measures model.
This indicates that baseline heart rate significantly varies across times and days. During
each day, as the length of anesthesia increased, the heart rate decreased (heart rate at time
0 was statistically significantly different from that at times 30 and 60 and heart rates at
times 30 and 60 also significantly differed). Days 1 and 2 were not statistically different
from each other, but they differed from day 3. Interaction between day and time was not
statistically significant (The pairwise comparisons are not shown.)
SAS output:
Solution for Fixed Effects
fEfect
Pr > ltl
Intercept
Estimate
standard
Error
DF
t Value
45.0088
1.9249
5
23. 38
0
10.5247
0.7227
44
14.56
30
2.9310
0.7227
44
4.06
TIME
DAY
<.0001
TIME
<.0001
TIME
0.0002
TIME
60
DAY
0.0349
DAY
0.0202
DAY
0
1
1.5727
0.7227
44
2 .18
2
1. 7423
0.7227
44
2.41
3
Effect
TIME
DAY
0
Type 3 Tests of Fixed Effects
Num
Den
DF
DF
F Value
2
44
112.99
2
44
3.53
Pr > F
<.0001
0.0377
Example 1: Row data of statistical analysis of heart rate baseline made using the
computer software, SAS.
63
Absolute Increase in Heart Rate
At each time and day, the change in heart rate between baseline and maximum
during the tilt (calculated as maximum - baseline) was positive and statistically
significantly different from zero, indicating that there was a significant increase in heart
rate between these measurements.
When only time and day were included in the model, time had a significant effect
on the absolute increase in heart rate from baseline to the maximum during the tilt (P<
0.0001). Day was not statistically significantly associated with the increase (P=0.6663).
Interaction between day and time was not statistically significant.
When the baseline heart rate was included in the model to account for the
variability between dogs and across days and times, neither time (P=0.50) nor day
(P=0.92) were significantly associated with the maximum absolute increase in heart rate.
Baseline heart rate, however, was a strong confounder (the effects of day and time on
absolute increase in heart rate changed considerably after inclusion of baseline heart rate
in the model). However, it only had an effect of borderline statistical significance
(P=0.06) on the absolute increase (as the baseline heart rate increased, also the absolute
increase between the times points became slightly higher).
64
SAS output:
Solution for Fixed Effects
Standard
Error
DAY
Estimate
TIME
Effect
Pr > ltl
Intercept
0.0005
c bl
0-:-0631 (the baseline hr is centered at 50 (the
TIME
0
0.2492
mean) to make the interpretation
TIME
30
0.5642
of the results more meaningful)
60
TIME
DAY
0.9956
DAY
0.7319
DAY
Effect
ltl
TIME
<.0001
TIME
<.0001
TIME
<.0001
DAY
<.0001
DAY
<.0001
DAY
<.0001
TIME
DAY
t Value
13.0746
1. 6380
5
7.98
0.3024
0.1585
43
1. 91
2.4592
2.1055
43
1.17
0.7938
1. 3660
43
0.58
0
1
0.007230
1. 3086
43
0.01
2
0.4531
1.3139
43
0.34
3
Effect
c bl
TIME
DAY
DF
0
Type 3 Tests of Fixed Effects
Num
Den
DF
DF
F Value
1
3.64
43
2
43
0.69
2
43
0.08
Least Squares Means
Standard
Estimate
Error
Pr > F
0.0631
0.5092
0.9231
DF
t Value
Pr >
0
15.8684
1.5567
43
10.19
30
14.2030
1.2521
43
11. 34
60
13.4092
1.4186
43
9.45
1
14.3473
1. 2298
43
11. 67
2
14.7932
1. 2317
43
12.01
3
14.3401
1. 2400
43
11. 56
Example 2: Row data of statistical analysis of absolute increase in heart rate baseline
made
usmg
the
computer
software,
SAS.
65
Absolute Decrease in Heart Rate
At each time point and day, the change in heart rate between the maximum during
the tilt to the minimum during the recovery (calculated as maximum - minimum) was
statistically significantly different from zero, indicating that there was a significant
decrease in heart rate between these measurements.
When only time and day were included in the repeated measures model, both
factors were statistically significantly associated with the absolute decrease in heart rate.
The interaction between day and time was not significant.
When the initial value (the maximum heart rate during the tilt) from which the
change was calculated was included in the model to account for the varying starting
levels among dogs across days and times, only day remained significant (P<0.0001). The
starting value, maximum heart rate, was a strong confounder and also had a significant
effect on the decrease.
The results from the repeated measures model suggest that the absolute decrease
in heart rate becomes greater as time passes (the length of anesthesia increases) when the
effect is adjusted for the starting heart rate and day. (This appears to be different from if
we look at the 'raw' values or from the results that were not adjusted for the starting heart
rate. Thus, it could be concluded that the starting heart rate has a strong impact on the
absolute decrease.) Also, as the experiment advances from day 1 to day 2 to day 3, it
appears that the absolute decrease in heart rate becomes larger.
66
SAS output:
Solution for Fixed Effects
Standard
DAY
Estimate
Error
Effect
TIME
Pr > ltl
Intercept
0.0001
c hrm
<-:-0001
(max. hr was centered at 60 to make
TIME
0
0.0653
the interpretation 'meaningful' )
TIME
30
0.1656
TIME
60
DAY
<.0001
DAY
0.0026
DAY
Effect
ltl
TIME
<.0001
TIME
<.0001
TIME
<.0001
DAY
<.0001
DAY
<.0001
DAY
<.0001
TIME
DAY
t Value
18.8764
1. 7227
5
10.96
0.4828
0.08451
43
5. 71
-3.1948
1. 6888
43
-1. 89
-1. 5042
1.0664
43
-1. 41
0
1
-4.3814
1. 0077
43
-4.35
2
-3.2588
1.0190
43
-3.20
3
Effect
c hrm
TIME
DAY
DF
0
Type 3 Tests of Fixed Effects
Den
Num
DF
DF
F Value
1
43
32.64
1.87
2
43
10.06
2
43
Least Squares Means
Standard
Estimate
Error
Pr > F
<.0001
0.1662
0.0003
DF
t Value
Pr >
0
15.5938
1. 7792
43
8.76
30
17.2843
1.6105
43
10.73
60
18.7885
1.7024
43
11.04
1
15.3876
1.5991
43
9. 62
2
16.5101
1.6015
43
10.31
3
19.7690
1. 6043
43
12.32
Example 3: Row data of statistical analysis of absolute decrease in heart rate baseline
made
usmg
the
computer
software,
SAS.
67
Results of Changes in Pressures at Carotid and Aortic Sinuses During the Initial 5
Seconds of the Head-up Tilt
Graphs depicting changes in heart rate and in various pressures at the aortic
(Figure 21) and carotid (Figure 22) sinuses are shown. Heart rate increased
approximately 12 beats/minute, while peak systolic (p= 0.027), diastolic (p= 0.014), and
mean pressures (p= 0.029) decreased more at the carotid sinus than at the aortic sinus
(Table 7). Pulse pressure tended to decrease more at the aortic than the carotid sinus, but
this did not achieve statistical significance (p= 0.545). This information can be visualized
in (Figure 23) showing the raw data recorded of heart rate, carotid and aortic sinuses
pressures during the tilt.
68
Changes in (Heart rate, Aortic sinus pressure) during the inlial 5 seconds of the Head-up tilt
10
ti
:i:
E
E
[
:e.
l11AVG N=41
5
w
Cl
~
PARAMElERS (HR, Ao)
HR= heart rate; HR rec= heart rate recovery; AoS= aortic sinus systolic pressure ; AoS rec= Aortic
sinus systolic pressure recovery from the head-up tilt; AoD= Aortic sinus diastolic pressure; AoD
rec= Aortic sinus diastolic pressure recovery; Mean Ao= mean aortic sinus pressure; Mean Ao rec=
mean aortic sinus pressure recovery from head-up tilt; Puls Ao= pulsatile aortic sinus pressure; Puls
Ao rec=pulsatile aortic sinus pressure recovery from head-up tilt.
Figure 21: Graph showing the mean changes in heart and aortic sinus (various pressures)
during the initial 5 seconds of the head-up tilt.
69
Changes in (Heart rate, Carotid sinus pressure) during the intial 5 seconds of the Head-up tilt
20
15
10
iC
ie
a
e=..
5
0
s
fo;l
c
~
-5
u
-10
-15
-20
PARAMETERS (HR, Cs)
I aAVG N=4j
HR= heart rate; HR rec= heart rate recovery; CsS= carotid sinus systolic pressure ; CsS rec= carotid sinus
systolic pressure recovery from the head-up tilt; Cs D= carotid sinus diastolic pressure; Cs D rec= carotid
sinus diastolic pressure recovery; Mean Cs= mean carotid sinus pressure; Mean Cs rec= mean carotid
sinus pressure recovery from head-up tilt; Puls Cs= pulsatile carotid sinus pressure; Puls Cs rec=pulsatile
carotid sinus pressure recovery from head-up tilt.
Figure 22: Graph showing the mean changes in heart and carotid smus (various
pressures) during the initial 5 seconds of the head-up tilt.
70
AVG
SD
AVG
SD
HR tilt
CsS tilt
CsD tilt
Mean Cs tilt
Puls Cs tilt
12.30
(5.73)
HR tilt
-15.50
(5.60)
AoS tilt
-14.25
(6.55)
AoD tilt
-12.75
(5.54)
Mean Ao tilt
-1.25
(3.94)
Puls Ao tilt
12.30
(5.73)
-6.00
(5.09)
-3.75
(5.79)
-4.58
(5.05)
-2.25
(2.21)
Table 7: Shows the heart rate, carotid and aortic sinus pressures change during the initial
5 seconds of the head-up tilt for 4 dogs.
AVG= average; SD= standard deviation; SEM= standard error mean; HR tilt= heart rate; CsS = carotid
sinus systolic pressure; CsD= carotid sinus diastolic pressure; Mean Cs= mean carotid sinus pressure; Puls
Cs tilt= pulsatile carotid sinus pressure. AoS= aortic sinus systolic pressure; AoD= aortic sinus diastolic
pressure; Mean Ao= mean aortic sinus pressure; Pul Ao= pulsatile aortic sinus pressure.
Pressure (Gain):
Gain could be calculated only if both change in pressure and change in heart are
known. This occurred in only the 4 dogs from which pressure was recorded. However,
change in pressure could be estimated--and should always have been constant--during
the initial 5 seconds of the tilt when only the tilt affects pressure (i.e., before homeostatic
responses could occur). Using data on the 4 dogs in which the change in carotid sinus
pressure was measured (averaging 15 mmHg) to calculate the degree of unloading the
carotid sinus baroreceptors, an average gain of 12 beats/minute: 15 mmHg, or 0.8
beats/minute/mmHg.
The gain was calculated for 6 dogs as the ratio of change in heart rate to change in
carotid sinus pressure, however since carotid sinus pressure was not measured, the
change in that pressure was taken as the weight of the vertical height of fluid between the
72
position of the carotid sinus and the heart-always the same for all dogs and
approximated to 15 mmHg. Table 8 shows the average gain with its standard deviation
for all 6 dogs by day (1,2,3) and by time (0,30,60). When subjected to ANOVA there
were no differences among means either by day (p=0.14) or by time (p=0.992), nor was
there a day-time interaction (p=O. 751 ).
Means and standard deviations by day and time are presented in the table 8.
Figure 24 shows a graph of the average calculated gain by day and time for 6 dogs.
Gain
Absolute Increase between
Baseline and 5 seconds after tilt
Time
(minutes)
Dayl
Day2
Day3
Dayl
Day2
Day3
0
11.461
(2.410)
9.478
(5.331)
9.127
(2.935)
10.264
(5.539)
10.443
(3.397)
12.279
(2.544)
9.417
(4.338)
9.646
(4.036)
8.623
(4.212)
0.764
<0.160)
0.632
(0.355)
0.608
(0.195)
0.684
(0.369)
0.696
<0.226)
0.819
C0.169)
0.628
(0.289)
0.643
<0.269)
0.575
C0.280)
30
60
Table 8: Shows the absolute_increase in heart rate for all 6 dogs during the initial 5
seconds of the head-up tilt. This absolute-increase heart rate was then, divided by 15 to
obtain the gain (on the right side of the table).
73
Gain calculated for 6dogs
- 1.5 -,---------------:::c:
8
~
1 +-~-----~~---+~----------~~~~-
s
ao
030
~0.5
-
160
Day1
Day2
Day3
Tmi (days)
Figure 24: Graph showing the calculated gain based on the heart rate change during the 5
initial seconds of the head-up tilt, by day (1, 2, 3) and time (0, 30, 60) minutes.
74
As can be seen from the graphs above, there was a considerable amount of
variability between dogs as well as within dogs in the "absolute_increase at 5seconds".
For all dogs the change in heart rate from baseline to 5 seconds after tilting was positive
(i.e., increase in heart rate) at every time point in each day, with average range (from 8 to
12), as can be seen in table 7. (The graphs would look identical for the outcome "gain",
as it is the same variable, just scaled differently, as it was calculated by dividing the
absolute increase at 5 seconds by 15 (change in blood pressure after tilt). Houston
developed 200 degree AV block of Mobitz type I-Wenchebach phenomenon on day 3,
therefore heart rate was not possible be measured.
Recovery from anesthesia, and analysis of vital tissues
While dogs did not recover from each anesthetic episode as smoothly as from
isoflurane, they elevated their heads within 1. 5 hours, they stood staggeringly within 2
hours, and they walked normally within 4 hours. All dogs defecated, none vocalized, and
all were sensitive to noise, but no dog became violent or developed seizures during
recovery from anesthesia.
Analysis of the blood constitutes showed no difference between values before the
initial anesthesia and before the final anesthesia (Table 2 and 3). No samples were
obtained after the final anesthesia, because value would have been so distorted by the
large volume required for the anesthetic.
There were histopathological changes (Table 4 ), however none appeared to be
related to the anesthetic.
76
CHAPTERS
DISCUSSION, LIMITATIONS, AND CONCLUSIONS
DISCUSSION
Difficulty/easiness of experiments: These experiments are relatively easy to
conduct. Less than 90 minutes was required from induction to anesthesia to the last tilt.
Even when arteries (carotid, femoral) were catheterized, minimal surgical expertise was
required. The fact that baroreceptor function could be measured with minimal or no
surgical interventions may be important, since surgical interventions involving
thoracotomy, pain, or possible denervation of autonomic nerves would no doubt
obfuscate results.
The anesthetic protocol to study baroreceptor function is enormously important.
Ideally no anesthetic would be used, since it is clear that any anesthetic will alter
baroreceptor function. It is known (Silverman and Muir, 1993), however, that anesthesia
with morphine-chloralose permits as nearly intact autonomic control of cardiovascular
77
function as is possible. Furthermore to study an awake dog would of necessity have
included psychological responses that would clearly impact on baroreceptor function.
Morphine is required before chloralose, since dogs anesthetized with chloralose, alone,
manifest usually a very turbulent induction and recovery, and since chloralose alone, is
not known to produce analgesia (Balis and Monroe, 1964). One dog, developed 2nd
degree AV block of Mobitz type 1-Wenchebach phenomenon-due no doubt to the
parasympathomimetic effect of morphine. Chloralose must be given in a rather large
volume of warm saline (250 ml for induction) and then sustained with a volume of
approximately 70 ml over the remainder of the protocol.
Dogs urinated minimally
throughout the study, thus volume expansion could be important. This volume expansion
may have altered the baroreceptors response, however there is no alternative manner for
anesthetizing with chloralose, and anesthetics requiring little volume for dilution (e.g.,
pentobarbital)-or given by inhalation (e.g., isoflurane)--are known to obfuscate
baroreceptor function prodigiously. All dogs were ventilated with room air during the
procedures since the anesthetic protocol depresses the respiratory system. This positive
pressure ventilation may alter baroreceptor function, however it is probably more
essential in studing baroreceptor function to sustain blood gasses (actually end-tidal
PC02) within limits of normal (PaC02 between 35 and 45 torr) than to allow them to
become disturbed.
An important goal of this study was to determine if the anesthetic protocol
produced manifestations of toxicity. First it is important that all dogs tolerated the
repeated episodes of anesthesia without apparent detriment.
78
This is in contradistinction to some reports of violent tonic convulsions induction (Balis
and Monroe, 1964). These convulsions were attributed to contamination of alpha
chloralose with beta chloralose, but in any case would have been precluded by preanesthesia with morphine.
There were no biochemical changes between pre-anesthesia on days 1 and 3, and no dog
manifested histological changes in any of the many organs evaluated. Ease of induction
to and recovery from anesthesia did not change between the
1st
and 3rd days. Thus
repeated anesthesia with morphine-chloralose-at least given 3 times over 9 days-can
be performed without concern for safety. A possible long-term manifestation of toxicity
was not addressed in this study. If 0 out of 6 dogs did not manifest toxicity, then the
upper limit of the 95% confidence interval for the general population not manifesting
toxicity would be 0.5 (i.e., 3/6) (Burke and Mann, 1979).
In this study the dogs were subjected to passive tilt, in which the thoracic and
pelvic limbs were supported so that tilting did not change the tension in skeletal muscles,
which might have stored blood displaced by gravitational forces (Bloomfield et al 1997;
Vardan et al, 1994). That is, by virtue of the fact that the muscles in the so-called
dependent portion of the torso were not under greater tension, the vascular components
could have sequestered more blood than if the dogs had been actively standing and the
muscles would have compressed the blood vessels. Therefore with passive tilt compared
with active tilt, more blood would have shifted to the pelvic quarters, less blood would
have returned to the heart, cardiac output and systemic arterial pressure would have fallen
79
more, and the baroreceptors reflex would have been activated with passive than with
active tilt.
When the high-pressure baroreceptors in the carotid sinus were displaced above
the heart, the pressure within decreased (i.e., the baroreceptors became "unloaded")
instantaneously. Then, as blood pooled with the pelvic quarters, the baroreceptors became
still more "unloaded" due to the decrease in cardiac output (see above).
Since the baroreceptor response (i.e., increase in heart due to decrease loading) is
mediated, very rapidly, via altered parasympathetic traffic, then there should have been
an immediate increase in heart rate followed by a slower increase (Berne and Levy,
1997).
Heart rates decreased (Figure 14) from heart rate before the initial tilt of each day
to before the second and the third tilt of each day. This reduction could not have been due
to reduction in body temperature, since all dogs were lying on a heating pad. More
likely, the reduction could be attributable to the duration of anesthesia, to changing depth
of anesthesia or to metabolic products. Because end-expiratory C02 was monitored and
kept between 35 and 45 torr, it is unlikely that respiratory acidosis was important,
however it is not unusual for animals to develop metabolic acidosis during prolonged
anesthesia. Because chloralose anesthesia was sustained with supplemental boluses of 3040 mg/kg/hour, it is highly likely that the rate of infusion exceeded the rate of
metabolism. While this is not dangerous to the dogs since they were ventilated artificially
and all dogs awakened from anesthesia, the blood and tissue concentrations of chloralose
were not measured and may have increased gradually over time.
80
In addition, it is not known if chloralose is a satisfactory analgesic, and it is
possible that the increasing concentrations became more analgetic, suppressed cerebral
input, and slowed heart rate. The decrease in heart rate between the first and second
anesthetic epoch were always greater than between the second and third, thus this
explanation is implausible, since if the administration exceeded excretion and metabolism
between the first and second, it should have exceeded also between the second an third
unless metabolism and/or excretion increased.
There is no data to support that contention. It is also impossible to attribute the
decrease in heart rate to a parasympathomimetic effect of chloralose, since-when given
alone--chloralose actually increases heart rate.
Since the concentration of morphine
must have been declining, also, the decrease in heart rate is even more curious because
morphine is a known parasympathomimetic, therefore when it is metabolized heart
should have accelerated.
Even though day and time did not have statistically significant effects on absolute
heart rate increase, it would be incorrect to conclude from this that the increase in heart
rate is consistent and does not vary among days and times. It is likely that due to the
small sample size (6 dogs) and large variability among the measurements between dogs,
days and times, we did not have enough power to see statistically significant differences.
The results (both graphical and from the repeated measures model) suggest that
there was a trend (even though not statistically significant) towards a smaller increase in
heart rate as time passes, i.e. the longer the anesthesia continues. However, as the graphs
suggested, the change between times was not consistent across days.
81
In this study the gain of the high-pressure baroreceptor reflex was sought to
characterize it. Gain if the ratio of output to input, and for this reflex output would be
decrease in heart rate (an estimate of neural output from the baroreceptors to the medulla)
and input would be increase in distending force on the baroreceptors. In 4 dogs change in
intra-carotid blood pressure was measured, but in 6, pressure were not measured.
However for all head-up tilts the immediately unloading was presumed to equal the
weight of blood in the vertical column between the carotid sinus and the heart (Figure 3).
This occurred instantaneously, and should have elicited the baroreceptors response
virtually instantaneously over the very rapid-acting arm of the autonomic nervous
system-the parasympathetic portion. In (Figure 26) it can be observed that there was, in
fact, an immediate decrease in pressure within the carotid artery (solid arrow). This
resulted in an instantaneous and slight increase in heart rate. Then there was a greater and
more sustained decrease in pressure (open arrow) that resulted, no doubt, from pooling of
blood in the dependent portions of the body, decrease in venous return, decrease in
cardiac output, and decrease in arterial pressure.
82
1.:0.C
Figure 26: Raw data of carotid and aortic arch sinuses pressures. The solid arrow
represents the first decrease in carotid sinus blood pressure, and the open arrow indicates
the additional fall in carotid sinus blood pressure due to the blood being pooled towards
the dependent portions of the body. Aortic arch sinus pressure and heart rate are the two
next traces from top to bottom. The X-axis is time with units in seconds.
83
This further and more sustained decrease in pressure resulted in a prolonged and greater
increase in heart rate.
After the increase in heart rate, it can be observed that heart rate decreased toward
pre-tilt levels as blood pressure returned to are pre-tilt levels. This increase in pressure
results, no doubt, from a return in venous return after the veins in the dependent portions
of the torso became full, and other haemostatic mechanisms (e.g., rennin-angiotensinaldosterone-sympathetic), which decreased venous capacitance.
The results describe heart rate and pressure. The gain should be the instantaneous
change in heart rate divided by the instantaneous change in blood pressure, remembering
that this pressure was actually measured in 4 dogs (Table 8 and Figure 24).
Pressures at the level of the carotid sinus changed more than at the aortic sinus.
This occurs, no doubt, because, in response to tilting, the carotid sinus is moves upward
from the level of the heart by the vertical distance between the heart and the carotid sinus,
whereas that distance is less for the aortic sinus, which lies closer to the heart. That is the
vertical distance between the carotid sinus is greater than that for the aortic sinus.
The gain the HPBR reflex is given as the ratio of change in HR (i.e., the "output")
to change in pressure (i.e., the "input"). The reflex is thought to be influenced similarly
by both the aortic and carotid sinuses (Berne and Levy, 1972), therefore the gain in this
study is taken as the change in heart rate divided by the change in carotid sinus pressure.
It is not known when the forcing on the carotid sinus is greater than that on the aortic
sinus, which should be used to calculate the gain of the entire system.
84
It is not known, when forcing on the receptor are different from those on another,
whether the effect on heart rate should be summed, averaged, or treated in some other
manner. Gain in this study is taken as the ratio of change in heart rate to change in carotid
sinus pressure .... neglecting effects on and influences by the aortic sinus. The average
gain of the HPBR reflex is 12 beats/minute: 15 mmHg.
The study demonstrates no change in gain of the high-pressure baroreceptors
(ratio of change in heart rate to change in carotid sinus pressure) by either day or time or
by day-time interaction. This apparent lack of difference may be an artifact caused by the
relatively high standard deviations, average coefficient of variation being 0.474 (SD
0.213), or in fact it may represent that there truly is no change in gain over either time or
day.
It is impossible to compare these values for gain with those obtained by others,
for a variety of reasons. First the anesthetic protocol used here is unique; most others use
sodium pentobarbital. Second the technique used here is orthostatic change, whereas
others used either response to vasoactive compounds (i.e., nitroprusside, phenylephrine)
or neck suction. In the study using pentobarbital the gain of the baroreceptor reflex
varied between 0.5 and 1.8; the mean gain here is 0.654, SD 0.113, maximum 0.818,
minimum 0.479. Thus the mean value in this study is slightly less than the mean value
reported for pentobarbital. This is unexpected, since pentobarbital is known to blunt the
baroreceptor response and therefore should reduce the gain.
85
The difference may be attributable to greater changes in blood pressure produced
by the vasoactive agents, or to a direct effect of the vasoactive agents on the baroreceptor,
i.e., not merely the change in pressure.
Most investigators utilize the Oxford method to establish baroreceptors function.
In so doing, however, one of the "outputs: of the reflex (i.e., vasomotion) is obfuscated
by the forcing (vasomotion). The orthostatic and neck suction methods permit monitoring
both change in heart and change in vascular tone in response to change in blood pressure.
Can these results be extrapolated to the general population? These dogs were all
medium size, they were all males, and they were all in good health. The more rigidly
controlled a study, by definition, the less generalized are the results.
86
LIMITATIONS
The purpose of this study was to determine if gain of the high-pressure
baroreceptor could be measured reproducibly from dogs anesthetized repeatedly over 9
days, this being an indicator of the possible effect of repeated anesthesia with morphinechloralose. The fact that no differences of significance in gain were observed may be due
to the small number used and to the relatively great coefficient of variation of the values.
This study did not determine if gain would remain constant over longer periods, with
different anesthetics, or with more anesthetic episodes with morphine-chloralose.
Furthermore, gain was measured over a relative small change in pressure produced by
tilt, versus the larger changes that are produced by either the Oxford or neck-section
methods.
Baroreceptor function was monitored only by ratio of change in heart to
change in pressure over the limited range (i.e., by gain), and neither threshold nor
saturation point was monitored. Furthermore the heart rate responses to neither return to
the horizontal posture from head-up tilt nor the movement from horizontal to head-down
tilt were assessed. Although it is clear that repeated anesthesia did not produce
histopathological or blood chemical evidence of an anesthetic effect, this may not be
applicable to animals afflicted with diseases (e.g., heart failure).
87
A major limitation is the lack of assurance that constant levels of anesthesia were
maintained over the 3 recordings of each day, or if constant levels were achieved each
day. This shortcoming is virtually impossible to overcome unless tissue concentrations
are measured, but would not be present if volatile anesthetics (e.g., halothane,
sevofluorane) were used. Recovery from this anesthetic protocol is relatively long
compared to other anesthetics (e.g. propofol, isoflurane), and dogs recovered less
peacefully than for anesthetics with narcotic or analgesic properties. Because of the
variability of values for gain and the small "n", the power of this study at an alpha of 0.1
was <0.1-well below an acceptable limit of at least 0.6.
Finally the specific relationship between heart rate and body posture depends
upon the effect of changing posture on all baroreceptors, some located below and some
above the level of the heart, therefore subjected to differing perturbations of pressure
because of their position. The totality of the input to the medulla from these highpressure baroreceptors depends upon the effects of tiling on their stimulation and their
relative sensitivities. Although both aortic and carotid receptors are thought to posses
equal gain, this is not known for the numerous other receptors. Thus a buffering of the
baroreceptor response elicited from changing pressure at the carotid sinus may alter,
profoundly, the role of only the carotid sinus receptors. Of course this variability by
position could be circumvented using the Oxford method of perturbing the receptors,
since the change in pressure is independent of their position. The neck suction device
would affect only the carotid sinus receptors; therefore the lack of input from all other
baroreceptors would be absent.
88
CONCLUSIONS
1. Repeated anesthesia with morphine/chloralose results in no observable
pathological changes monitored by histopathology, blood chemistry, and analysis of
blood cellular components.
2. Gain of high-pressure baroreceptor reflex may be assessed using the passive
head-up tilt.
3. Gain did not appear to change significantly within an anesthetic period or on
subsequent days.
4. For head-up tilt, the change in pressure on the carotid sinus was greater than the
change of pressure on the aortic sinus.
89
REFERENCES
Abraham A. The structure of baroreceptors in pathological conditions in man. In:
Baroreceptors and Hypertension, edited by P. Kezdi. Oxford: Pergamon. 273-291,1967.
Abrahamsson C, AAhlund C, Nordlander M, Lind L. A method for heart rate-corrected
estimation ofbaroreflex sensitivity. J Hypertens. 21:2133-2140,2003.
Ageyama, Naohide et al. Specific gravity of whole blood in Cynomologus monkeys,
squirrel, monkeys, and tarnarins. Contemporary Topics in Lab An Sciences. 40:3, 2001.
Bagshaw RJ, Fischer JM. Morphology of the carotid sinus in the dog. J. Appl Physiol.
31: 198-202,1971.
Balis GU and Monroe RR. The pharmacology of chloralose. Psychopharmacology 6: 130, 1964.
Baum T et al. Antihypertensive and orthostatic responses to drugs in conscious dogs. J.
Pharmacol. Methods 6:21-32, 1981.
Bedford et al. Arterial hemodynarnics during head up tilt in conscious dogs. J. Appl.
Physiol. 65: 1556-1562, 1968.
Berkowitz WD, Scherlag BJ, Stein E, Damato AN. Relative roles of sympathetic and
parasympathetic nervous systems in the carotid sinus reflex in dogs circulation.
Circulation Res. 24:447-455, 1969.
90
Berne RM and Levy MN. Cardiovascular Physiology, St Louis: Mosby.265 pages, 1972.
Borst C, Wieling W, Van Brederode JFM. Mechanisms of initial heart rate response to
postural change. Am J Physiol. 243:H676-H681, 1982.
Bronk DW, Ferguson LK, Magaria R, Solandt DT. The activity of the cardiac
sympathetic centers. Am. J. Physiol. 117:237-249, 1936.
Brown AM. Brief Reviews. Receptors under pressure - An uptake on baroreceptors.
Circulation Research. 46: 1-10, 1980.
Burke WE, Irvin DG. Electronics- Basic Principles. 1st. Ed. 752 pages.
Constantine JW, McSane WK, Wang SC. Comparison of carotid artery occlusion and tilt
responses in dogs. Am J Physiol. 221:1681-1685, 1971.
Cowley AW, Merrill D, Osborn J, Barber BJ. Influence of vasopressin and angiotensin
on baroreflex in the dog. Circ. Res. 54:163-172, 1984.
Daly M de B, Verney EB. Localisation of receptors involved in the reflex regulation of
the heart rate. J Physiol. London. 62:330-340, 1926.
Davies LC, Francis DP, Jurak P, et al. Reproducibility of methods for assessing
baroreflex sensitivity in normal controls and in patients with chronic heart failure.
Clinical Science. 97:515-22, 1999.
De Vleeschhouwer GR, Heymans C. Baroreceptors and reflex regulation of heart rate. In:
Baroreceptors and Hypertension, edited by Kezdi. Oxford: Pergamon. 187-190, 1967.
Delaunois AL, Bernard PJ. Cardiac output during carotid sinus reflexes. In:
Baroreceptors and Hypertension, edited by P. Kezdi. Oxford: Pergamon. 181-185, 1967.
Donald DE, Edis AJ. Comparison of arotic and carotid baroreflexes in the dog. J Physiol.
London. 215:521-538, 1971.
91
Downing SE, Siegel JH. Baroreceptor and chemoreceptor influences on sympathetic
discharge to the heart. Am. J. Physiol. 204:471-479, 1963.
Duchene-Marullaz P, Fabry-Delaigue R, Gueorguiev G, Kantelip JP. Influence of
chloralose and pentobarbitone sodium on atrioventricular conduction in dogs. Br. J.
Pharmac. 77:309-317, 1982.
Dwain LE. Nonlinearities of the humam carotid baroreceptor-cardiac reflex. Circ Res.
47:208-216, 1980.
Eckberg DL, Cavanaugh MS, Mark AL, et al. A simplified neck suction device for
activation of carotid baroreceptor. J Lab Clin Med. 85:167-73, 1975.
Ewing DJ, Hume L, Campbell IW. Autonomic mechanisms in the initial heart rate
response to standing. J Appl. Physiol.: Resp. Envirom. Physiol. 49:809-14, 1980.
Feigl EO. Carotid sinus reflex control of coronary blood flow. Circulation Res. 23:223237, 1968.
Froget G, Betat AM, Camus L, Lainee P. Evaluation of orthostatic reactivity in a
conscious dog tilt model using telemetry. Safety Pharmacology Society, 4th. Annual
meeting, Covington, Kentuky, September, 2004.
Goldstein RE, Beiser GD, Stampfer M, et al. Impairment of autonomically mediated
heart rate control in patients with cardia dysfunction. Circ Res. 36:571-77, 1975.
Grigoreva TA. The innervation of blood vessels. New York: Pergamon, 1962.
Haibara AS, Santos RAS. Descobrimento e importancia dos baroreceptors. Rev. Bras
Hipertens. 7(2):113-115, 2000.
Hainsworth JR, Ledsome R, Carswell F. Reflex responses from aortic baroreceptors.
American Journal of Physiology. 218:423-429, 1970.
92
Hall JE. Integration and regulation of cardiovascular function. Adv in Physiol Educ.
22:S174-Sl86, 1999.
Halliwill JR, Billman GE. Effect of general anesthesia on cardiac vagal tone. American
Physiology Society. HI 719-24, 1992.
Hamlin RL, Smetzer DL, Breznock EM. Sinoatrial syncope in miniature schnauzers. J
Am Vet Med Assoc. 161: 1022-1027, 1972.
Heymans C, Neil E. Reflexogenic Areas in the cardiovascular system. London: Churchill,
1958.
Honda K et al. Orthostatic hypotension: with particular reference to experimentally
induced orthostatic hypotension model in dogs. Int. Angiol. 12:110-112, 1993.
Iriuchijima JE, Soulbsby JR, Wilson MF. Participation of cardiac sympathetics in carotid
occlusion pressor reflex. Am J. Physiol. 215: 1111-1148, 1968.
James A J, Daly DM. Comparison of reflex vasomotor responses to separate and
combined stimulation of carotid sinus and aortic arch baroreceptors by pulsatile and nonpusatile pressure in the dog. J. Physiol., London. 209:257-293, 1970.
Katona PG, Poitras JW, Barnett GO, Terry BS. Cardiac vagal efferent activity and heart
period in the carotid sinus reflex. 218:1030-37, 1970.
Kennon MG, Jiangping G. Enhancement of l-Aminobutyric Acid Receptor Activity by
CX.-Chloralose. The Journal of Pharmacology and experimental therapeutics. 285: 680-686, 1998.
Kikushima S, Kobayahi S, Nakagawa H, Katagiri T. Triggering mechanism for neurally
mediated syncope induced head-up tilt test: role of catecolamines and response to
propanolol. J Am Coll Cardiol Journal. 33:350-357, 1999.
93
Kirchheim HR. Systemic arterial baroreceptor reflexes. Physiological Reviews. 56: 100176, 1976.
Lamberti JJ, Urquhart J, Siewers RD. Observations on the regulation of arterial blood
pressure in unanesthetized dogs. Circulation Research. 23:415-28, 1968.
Lida R, Hirayanagi K, Iwasaki K. Non-invasive assessment of hum.am baroreflex during
different body positions. Journal of the Autonomic Nervous Sustem. 75:164-70, 1999.
Littell RC, Milliken GA, Stroup WW, Wolfinger RD. SAS System for mixed models.
SAS Inst. Inc., Cary NC, 4th. Ed. 633 pages, 1996.
McCubbin JW, Green JH, Page Ill. Baroreceptor function in chronic renal hypertension.
Circulation Research. 4:205-210, 1956.
Mortara A, Tavazzi L. Prognostic implications of autonomic nervous system analysis in
chronic heart failure: role of heart rate variability and baroreflex sensitivity. Archives of
Gerontology and Geriatrics. 23:265-75, 1996.
Muratori G. Histological observations on the structure of the carotid sinus in man and
mammals. In: Baroreceptor and Hypertension, edited by P. Kezdi. Oxford: Pergamon,
253-265, 1967.
Paintal AS. Cardiovascular receptors. In: Handbook of Sensory Physiology. Berlin:
Springer Verlag. 3(1): 1-45, 1972.
Parati G, Di Rienzo M, Mancia G. How to measure baroreflex sensitivity: from the
cardiovascular laboratory to daily life. J Hypertens 18:7-19, 2000.
Rawling EG. Sir Astley Paston Cooper, 1768-1841: "the prince of surgery". Can Med
Assoc J. 3;99(5):221-5, 1968.
Ress PM, Jepson P. Measurement of arterial geometry and wall composition in the
carotid sinus baroreceptor area. Circulation Research. 26:461-467, 1970.
94
Sagawa K, Watanabe K. Summation of bilateral carotid sinus signals in the barostatic
reflex. Am J Physiol. 209:1278-1286, 1965.
Salgado HC, Krieger EM. Extent of baroreceptor resetting in response to sodium
nitroprusside and verapamil. Inter-American Society Proceedings. Suppl I Hypertension.
11:1-1211-125, 1988.
Scher AM, Young AC. Nonlinearity in the control of blood pressure and heart rate. Ann.
N.Y. Acad. Sci. 156:722-730, 1969.
Schwartz DS. Studies on baroreceptor function in dogs.1-131, 2000. Dissertation
Shimokawa A, Kunitake T, Takasaki M, Kannan H. Differential effects of anesthetics on
sympathetic nerve activity and arterial baroreceptor reflex in chronically instrumented
rats. Journal of the Autonomic Nervous System. 72:46-54, 1998.
Shubrooks Jr. SJ. Carotid sinus counterpressure as a baroreceptor stimulus in the intact
dog. Journal of Applied Physiology. 32:12-19, 1972.
Silverman J, Muir WW III. Special Topic Review. A review of laboratory animal
anesthesia with chloral hydrate and chloralose. Laboratory Animal Science. 43:210-216,
1993.
Sisson DD. Neuroendocrine evaluation of cardiac disease. Vet Clin Small Anim.
34:1105-1126, 2004.
Smyth HS, Sleight P, Pickering GW. Reflex regulation of arterial pressure during sleep in
man. A quantitative method of assessing baroreflex sensitivity. Circ Res. 24:109-121,
1969.
Stegemann J, Tibes U. Sinusoidal stimulation of carotid sinus baroreceptors and
peripheral blood pressure in dogs. Ann. N. Y. Acad. Sci. 156:787-795, 1969.
95
Thames MD, Kontos HA. Mechanisms of baroreceptor-induced changes in heart rate.
Am J. Physiol. 218:251-256, 1970.
Triedman JK, Saul JP. Blood pressure modulation by central venous pressure and
respiration. Buffering effects of the heart rate reflexes. Circulation. 89: 169-179, 1994.
Van Citters RL, Franklin DL, Rusmer RF. Left ventricular dynamics in dogs during
anesthesia with alpha-chloralose and sodium pentobarbital. The Am. J. of Cardiology.
349-354, 1964.
Vardan S, Hill NE, Mehrotra KG, Mookherjee S, Smulyan H. Baroreflex function during
45-degree passive head-up tilt before and after long-term thiazide therapy in the elderly
with systolic systemic hypertension.Am. J Cardiol. 73:253-7, 1994.
Vatner SF, Franklin D, Braunwald E. Effects of anesthesia and sleep on circulatory
response to carotid sinus nerve stimulation. American Journal of Physiology. 229: 124955, 1971.
Wang HH, Chai CY, Kuo JS, Wang SC. Participation of cardiac and peripheral
sympathetics in carotid occlusion response. Am. J. Physiol. 218:1548-1554, 1970.
Wang W, McClain JM, Zucker lli. Aldosterone induces baroreceptor discharge in dogs.
Hypertension. 19: 270-277. 1992.
Weber KT. Review article. Mechanisms of disease. Aldosterone in congestive heart
failure. N Engl J Med. 345:1689-1697, 2001.
Willius FA, Dry TJ: A History of the Heart and Circulation. Philadelphia: W B. Saunders
Co., 1948.
Ziemmer HD. Heinrich Ewald Hering and the carotid sinus reflex. Clin Cardiol. 27:486487, 2004.
96