* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Health care facility design, construction and renovation
Survey
Document related concepts
Sarcocystis wikipedia , lookup
Marburg virus disease wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Hepatitis C wikipedia , lookup
Gastroenteritis wikipedia , lookup
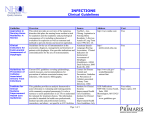
Hepatitis B wikipedia , lookup
Leptospirosis wikipedia , lookup
Trichinosis wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Pathogenic Escherichia coli wikipedia , lookup
Oesophagostomum wikipedia , lookup
Anaerobic infection wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Schistosomiasis wikipedia , lookup
Transcript
Prevention of Catheter-Associated Urinary Tract Infections 1. Describe the relevance of urinary tract infections in health care institutions. 2. Identify risk factors for urinary tract infections. 3. Describe measures for prevention. December 1, 2013 Learning objectives 2 • 50 minutes December 1, 2013 Time involved 3 • Up to 40% of all HAIs • Most involve urinary catheterisation • Risk of bacteriuria December 1, 2013 Introduction • 5% per day during the first week to almost 100% at 4 weeks of catheterisation • 1 to 4% of patients with bacteriuria will develop infection 4 December 1, 2013 Urinary tract sites commonly associated with infection 5 • Urine is an ultrafiltrate of blood, is normally sterile • Small numbers of perineal/ vaginal/bowel microorganisms in the distal urethra • Constantly washed out by micturition December 1, 2013 Urine • Bacteriuria = bacteria in the urine 6 • Specimen contamination reduced by • Cleaning external urethral area before collection • Collecting mid-stream urines • Urethral bacteria washed out in the first part of the stream December 1, 2013 Collection of urine • Processing specimen promptly, or refrigerating, to prevent overgrowth of contaminants 7 • Urine must be processed promptly • Contaminants can multiply at room temperature and give falsely high colony counts December 1, 2013 Laboratory diagnosis • If delay expected, transport the specimen in an ice box or add boric acid (1% W/V or 1 g/10 ml of urine) 8 • Usually endogenous microorganisms • E. coli and Proteus commonest in community infections • Catheter-associated UTI (CAUTI) December 1, 2013 Microbiology • E. coli commonest • Increasingly caused by resistant species • Klebsiella, Pseudomonas, Enterococcus and multiply drug resistant ESBL, VRE 9 Organism December 1, 2013 Bacteria Causing UTIs (%) Community Hospital E. coli Proteus Klebsiella Entero/Citro Pseudomonas Acinetobacter 80-90 5-8 1-2 45-55 10-12 15-20 2-5 10-15 <1 Coag -ve staph Staph aureus Enterococci 1-2 1-2 <1 10-12 <1 10 10 December 1, 2013 Microbiological support • The diagnosis of UTI depends on the microbiological support available • In patients with indwelling catheters, infections frequently polymicrobial • Presence of multiple bacteria does not necessarily indicate contamination 11 11 • Small numbers of bacteria are insignificant • True infections have large numbers in bladder urine • Microbiology labs count the number of bacteria in a urine specimen as ‘colony-forming units’ (cfu) • Significant bacteriuria gives a >95% likelihood of true UTI December 1, 2013 Quantitative bacteriology • ≥100,000 cfu/mL urine in 2 carefully-collected mid-stream urines (MSUs) 12 December 1, 2013 Urethral bacteria contaminate specimens, small numbers - - - - - Incubation Contamination - --- - - 102 -103 cfu/mL 13 • When large numbers of bacteria (>105/mL) in specimens of bladder urine & evidence of true UTI December 1, 2013 Significant bacteriuria • Smaller (insignificant) numbers may be due to contamination of the urine specimen during collection - urine has to pass through urethra • Contamination can come from perineum/genitalia 14 December 1, 2013 True UTI with significant bacteriuria - - - - - - - Infection Infection Natural incubation between micturitions - - - - - - - - -- -- - - - - - - -- - - - --- - - - - -- - - - - - - - -- - - - - >105 cfu/mL bacteria in bladder urine multiply to high numbers before collection 15 Number of patients 103 - 104 900 800 700 600 500 400 300 200 100 0 PROBABLE Mainly Gram+ves CONTAMINATION mixed species December 1, 2013 Quantitative microbiology distinguishes between true UTI & contamination or overgrowth 104 - 105 PROBABLE Mainly GramGram-ves INFECTION single species NOT INFECTED 10 1 10 2 INFECTED 3 10 10 4 10 5 Bacteria/mL 10 6 10 7 16 • In non-catheterised patients: • Fever, supra-pubic tenderness, frequency, dysuria • Pyuria • Positive nitrite reaction and a positive leukocyte esterase reaction December 1, 2013 Clinical diagnosis • In catheterised patients • Fever and leukocytosis or leucopenia additional diagnostic criteria 17 • Surveillance of CAUTI in selected patients • e.g. intensive care or surgical • Definition may be obtained: December 1, 2013 Definition and Surveillance • USA CDC/NHSN • Centers for Disease Control and Prevention/ National Healthcare Safety Network • HELICS • Hospital in Europe for Link Infection Control through Surveillance 18 • Normally urethral flora flushed out • With catheterisation, flushing mechanism circumvented • Flora can pass up through catheter or from drainage bag • Hands of personnel may contaminate the system during insertion or management December 1, 2013 Pathogenesis of a CatheterAssociated UTI 19 from Damani N N, Keyes JK. Infection Control Manual, 2004 December 1, 2013 Four main sites through which bacteria may reach the bladder in a catheterised patient 20 Care bundle approach • Evidence-based interventions • When implemented together result in reduction in CAUTIs December 1, 2013 Principles to Prevent UTI - 1 21 Staff training • Training on procedures for insertion and maintenance of urinary catheters based on local written protocols December 1, 2013 Principles to Prevent UTI - 2 Catheter size • Smallest diameter catheter that allows free flow of urine 22 Antimicrobial coated catheters • Reduce asymptomatic bacteriuria • For placement less than 1 week December 1, 2013 Principles to Prevent UTI - 3 • No evidence they decrease symptomatic infections • Should not be used routinely • Should be considered in selected high risk patients 23 Catheter insertion and care • • • • Sterile equipment and aseptic technique Sterile lubricant or local anaesthetic gel Meatal cleansing with soap and water Antimicrobial ointment harmful December 1, 2013 Principles to Prevent UTI - 4 • Should be avoided 24 Drainage tubing and bag •Secure to the patient •Catheter drainage bag below the bladder •Bag and tap not in contact with the floor •Clamp drainage during movements •Not disconnect the drainage bag •Bag emptied when ¾ full •Hand hygiene •Alcohol impregnated swabs •No disinfectant added to bag December 1, 2013 Principles to Prevent UTI - 5 25 Specimen collection • Samples from the port • Aseptic technique • Disinfection of port with alcohol • Sterile needle, syringe, container • Never a sample from the bag. • No routine testing December 1, 2013 Principles to Prevent UTI - 6 26 Antimicrobial agents • Routine administration not recommended • Single dose prophylactic may be used in selected patients • No routine use while the catheter in situ • Treatment may not be successful December 1, 2013 Principles to Prevent UTI - 7 27 Condom catheters • May be used for short-term drainage • Frequent changes • Removed if irritation or skin breakdown • Condom for 24 hour continuous use should be avoided December 1, 2013 Principles to Prevent UTI - 8 28 • Avoid urinary catheterisation • not for incontinence • consider intermittent catheterisation • Remove catheters as soon as possible • Aseptic technique and sterile equipment • Don’t change catheters routinely • Closed drainage system • No irrigation or instillation • Empty drainage bag December 1, 2013 Key points 29 1. 2. 3. APIC Elimination Guide: Guide to the Elimination of CatheterAssociated Urinary Tract Infections (CA-UTIs); Developing and applying facility-based prevention interventions in acute and long-term care settings, 2008. http://www.apic.org/Content/NavigationMenu/PracticeGuidance /APIC EliminationGuides/CAUTI_Guide.pdf HICPAC. Guidelines for prevention of Catheter-associated Urinary Tract infections 2009. Atlanta, GA: CDC, 2009. http://www.cdc.gov/hicpac/cauti/002_cauti_toc.html European and Asian guidelines on management and prevention of catheter-associated urinary tract infections. Intern J Antimicrobial Agents 2008: 31S; S68-S78. http://www.escmid.org/fileadmin/src/media/PDFs/4ESCMID_Lib rary/2Medical_Guidelines/other_guidelines/Euro_Asian_UTI_Gui delines_ISC.pdf December 1, 2013 References 30 4. 5. 6. SHEA /IDSA Practice Recommendation: Strategies to Prevent Catheter-Associated Urinary Tract Infections in Acute Care Hospitals. Infect Control Hospital Epidemiol 2008; 29 (Supplement 1): S 41-S50. http://www.jstor.org/stable/10.1086/591066 High Impact Intervention No 6. Urinary Catheter Care Bundle. London, Department of Health, 2007. http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@ dh/@en/documents/digitalasset/dh_078125.pdf UK Dept. of Health epic2: Guidelines for preventing infections associated with the use of short-term urethral catheters. J Hospital Infect 2007; 65S: S28-S33. http://www.vidyya.com/2pdfs/0124 infection.pdf December 1, 2013 References 31 7. 8. Infectious Diseases Society of America Guidelines. Diagnosis, Prevention, and Treatment of Catheter-Associated Urinary Tract Infection in Adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clin Infect Dis 2010; 50:625–663. http://www.idsociety.org/content.aspx?id=4430#uti December 1, 2013 References 32 1. 2. Incontinence is an indication for urinary catheterisation. T/F? For a general strategy to prevent UTI, what measure you would consider first: a) b) c) d) 3. Treatment of infected patients Avoid unnecessary catheterisation Replacement permanent catheterisation for intermittent Use of condom catheters December 1, 2013 Quiz Regarding prevention of UTI, which of the following is incorrect a) b) c) d) Keep system closed Hand hygiene before insertion/management of urinary devices Maintain catheter drainage bag below the bladder Use of antimicrobial prophylaxis in patients with urinary catheterisation 33 • IFIC’s mission is to facilitate international networking in order to improve the prevention and control of healthcare associated infections worldwide. It is an umbrella organisation of societies and associations of healthcare professionals in infection control and related fields across the globe . • The goal of IFIC is to minimise the risk of infection within healthcare settings through development of a network of infection control organisations for communication, consensus building, education and sharing expertise. • For more information go to http://theific.org/ December 1, 2013 International Federation of Infection Control 34