* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Chapter 42: Circulatory System Circulatory System – Heart, blood
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Myocardial infarction wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
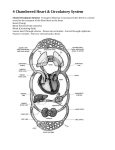
Chapter 42: Circulatory System Circulatory System – Heart, blood, & vessels Functions o Transports dissolved gases, nutrients, hormones, & metabolic wastes (e.g. urea, lactic acid) o Regulation of pH, electrolytes (ions) o Repair damaged tissue & vessels o Defense against toxins & pathogens o Stabilization of body temp Open Circulatory System o Insects (most arthropods), & most molluscs o Hemolymph bathes organs directly No distinction b/w blood & interstitial fluid (just body fluid) o ‘Heart’ pumps into open cavities Closed Circulatory System o Annelids, cephalopods, & vertebrates o Blood confined to vessels & distinct from interstitial fluid o More efficient at transporting circulatory fluids to tissues & cells Cardiovascular System – Circulatory & Lymphatic Systems Blood Vessels (~50,000 miles) o Arteries Carry blood away from heart Branch into arterioles which lead to capillary beds Heavy smooth muscle w/ elastin fibers, endothelial lining Deals w/ high pressure Very elastic (arterioles = less) o Veins Return blood to the heart Capillaries converge into venules, then converge into veins Same layers w/ less muscle Very low pressure B/w muscles (contract = blood moves) Valves – prevent blood backflow Diaphragm pressure also moves blood o Capillaries Thin-walled vessel One endothelial cell thick Facilitates exchange using all diffusion & bulk transport types Form dense, branched beds; 1,000 mi2 (only 250 of 5,000 ml of blood) Nutrient Exchange Occurs b/w blood & interstitial fluid across thin endothelial walls Difference b/w blood pressure & osmotic pressure drives fluids… o Out of capillaries at arteriole end o Into capillaries at the venule end Most blood proteins & all blood cells too large to pass thru endothelium Lymphatic System o Transports lipids from digestion o Returns interstitial fluid back to circulatory system Thoracic Duct drains into subclavian vein in neck o Lymph has lymphocytes (WBCs) o Valves in lymph vessels prevent backflow of fluid o Lymph Nodes Oval shaped gland Filled w/ honey-combed sacs made from connective tissue Space filled w/ lymphocytes Filter foreign materials & fight infections (multiply = swelling) o Lymph Organs: Thymus, spleen, tonsils ‘Educate’ lymphocytes that are made in bone marrow Heart o o o o o o o 4 muscular chambers enclosed in pericardium (i.e. sac) 2 Atria – collect venous blood & pump into… 2 Ventricles – pump blood to lungs & body Cardiac Muscle Striated & involuntary Cardiac Valves Atrioventricular Valves (lub) B/w Atria & Ventricles o Close during systole Right = Tricuspid Valve Left = Bicuspid Valve Semilunar Valves (dub) B/w Ventricles & 1st artery o Close during diastole Right Ventricle & Pulmonary Artery Left Ventricle & Aorta Cardiac Cycle Diastole – low pressure Ventricles relax (& filled) Atria contract Systole – high pressure Ventricles contract (& pump) Atria relax Cardiac Output Blood volume pumped per minute = Heart rate (beats/minute) & Stroke volume (amount pumped) Heartbeat Occurs w/o nervous stimulation Contraction starts in Right Atrium Sinoatrial (SA) Node = Pacemaker Cell mass that starts heartbeat Impulse spreads thru gap junctions & causes atrial contraction Atrioventricular (AV) node B/w Right Atrium & Ventricle Impulse pauses to allow full filling of ventricles Impulse spreads thru Bundle of HIS (‘hiss’) & Purkinje Fibers (muscle) Ventricles Contract Cardiac Control Pacemaker regulated by… Nervous System o Sympathetic speeds up heart Accelerator nerve from spine (spinal nerve) o Parasympathetic slows down heart Vagus nerve form brain (cranial nerve) Hormones (epinephrine = fast) Temperature Blood Flow High resistance = slow flow o Capillaries have highest resistance & slowest flow Vasodilation – smooth muscles relax in arterioles; blood pressure down o Nitric oxide is a major inducer Vasoconstriction – smooth muscles contract in arteriole walls; blood pressure up Precapillary sphincters can reduce capillary blood flow; helps divert blood elsewhere o o o Pulmonary Circulation Right Ventricle-Lungs-Left Atrium Right Ventricle pumps de-oxy blood through Pulmonary Arteries Arteries to arterioles to lung capillaries o O2 in & CO2 out (now oxy blood) Capillaries to Venules to Pulmonary Veins to Left Atrium o Systemic Circulation Systemic Circulation Left Ventricle-Body-Right Atrium Left Ventricle pumps oxy blood through Aorta to… Systemic Arteries to arterioles to body capillaries Venules to Superior & Inferior Vena Cavae to Right Atrium Systemic Divisions Coronary Circuit – Heart o Coronary Arteries & Veins Cranial Circuit – Head o Carotid Arteries & Jugular Veins Brachial Circuit – arms o Brachial Arteries & Subclavian Veins Mesenteric Circuit – Digestive System & Liver o Mesenteric Arteries, Hepatic Portal Vein, Hepatic Vein Renal Circuit – Kidney o Renal Arteries & Veins Lower Appendage Circuit – legs o Femoral Arteries & Iliac Veins General Blood Path Right Atrium – Tricuspid Valve – Right Ventricle – Semilunar Valve – Pulmonary Arteries – Arterioles – Lung Capillaries – Venules – Pulmonary Veins – Left Atrium –Bicuspid Valve – Left Ventricle – Semilunar Valve – Aorta – Systemic Arteries – Arterioles – Body/Organ Capillaries – Venules – Superior & Inferior Vena Cavae Blood Characteristics o Temp – 38° C (100.4 ° F) o Viscosity – 5x Water o pH – 7.35-7.45 o Volume 5-6 L adult males & 4-5 L adult females Blood Plasma (55%) o Water 92% of plasma volume Solvent for transport Gases – O2 & CO2 Organic wastes – urea, uric acid, NH4+, creatinine, bilirubin o Plasma Proteins 7% of plasma volume Made in Liver Albumin – osmotic balance & transports insoluble molecules Globulin o Transport globulin – move lipids, ions, others (e.g. LDL) o Immunoglobulin – antibodies Fibrinogen (inactive) – clotting Hormones & enzymes (regulatory) o Ions aka blood electrolytes 1% of plasma volume Osmotic balance, pH buffer, regulate membrane permeability Na+, K+, Ca2+, Mg2+, Cl-, HCO3-, HPO42-, SO42- Blood Cells (45%) o Hematopoiesis Process of blood cell formation Liver & spleen – embryo only Red (bone) Marrow Hematopoietic stem cells o Can become all blood cells o Mitosis makes more o Differentiate & released o Erythrocyte (RBC) Biconcave disc No nucleus, mitochondria, ribosomes Transports O2 & some CO2 250 million hemoglobins (4 O2) Erythropoiesis stimulated by Erythropoietin (EPO; Low O2) Ribs, vertebrae, sternum, & pelvis o Leukocyte (WBC) Larger, colorless, nucleated Often mature in lymph tissue e.g. T Lymphocyte named for Thymus Can leave circulatory system Basophil, eosinophil, neutrophil, lymphocyte, monocyte Dendritic cell, NK cell, T & B lymphocytes, macrophage o Platelet Very small amount of blood cells Cellular fragments that bud off from large stem cells in marrow Plays a critical role in coagulation (formation of solid clot from liquid blood) Blood Clotting Triggered when endothelium damaged & connective tissue exposed Platelets adhere to collagen o Release substance making surface sticky & more platelets stick o Tissue Factor (III; protein) released by damaged cells & platelets (starts cascade) Clotting Cascade o Mulit-step Clotting Factor cascade ends w/ inactive prothrombin (II) converted into thrombin Turns fibrinogen (I) into fiber Surround platelets & RBCs Shrink, pull together = clot o Thrombus – clot inside blood vessel Embolus – free-floating thrombus Blood Types o Type A (AA or AO genes) A Antigens, B Antibodies o Type B (BB or BO) B Antigens, A Antibodies o Type AB (AB) A & B Antigens, No Antibodies o Type O (OO) No Antigens, A & B Antibodies o Rh Factor – RBC protein present or not: +/- Cardiovascular Disease Disorders of heart & vessels #1 cause of death worldwide Cholesterol o Steroid used to keep membrane fluidity (temp buffer) o Low-density lipoprotein (LDL from liver) delivers cholesterol to cells for membrane production o High-density lipoprotein (HDL) scavenges cholesterol for return to liver o High LDL/HDL ratio = High risk of heart disease Atherosclerosis o Growth of plaques in inner wall of arteries Narrows lumen o Endothelium Inflammation (injury) starts process LDL enters artery lining; macrophages come & engulf (form foam cells) Extracellular matrix forms attracting more LDL & macrophages (plaque grows) o Plaque can rupture; blood clot formed o Arteriosclerosis (artery hardening) occurs if calcium is deposited Blockages Heart Attack (myocardial infarction) o Death of cardiac muscle tissue resulting from blockage of one or more coronary arteries (supply oxy blood to heart muscle) Stroke o Death of nervous tissue in brain, usually resulting from rupture or blockage of arteries in head Angina pectoris o Caused by partial blockage of coronary arteries & results in chest pains Hypertension o High Blood Pressure Promotes atherosclerosis & increases risk of heart attack & stroke Increases chances of endothelium inflammation (increases pressure) o Can be reduced by dietary changes, exercise, and/or medication