* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Heart Support
Saturated fat and cardiovascular disease wikipedia , lookup
Electrocardiography wikipedia , lookup
Heart failure wikipedia , lookup
Coronary artery disease wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
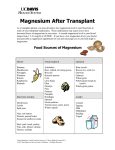
Program HE Heart Support Breakfast Organic oatmeal, milk, soymilk, or goat’s milk, 3 Tbsp. fresh ground flaxmeal * Hot brown rice cereal w/cinnamon and freshly ground almonds, green tea * Organic cottage cheese with flax oil, organic fruit or raw nuts (almonds, walnuts), green tea * 1 cup cottage cheese or yogurt, 1 tablespoon flax oil, 1 Tbsp. natural preserves * Poached organic omega-3 eggs or three egg omelet, sweet potatoes w/rosemary, ½ cup black beans * 2 organic eggs any style, 1 slice whole grain toast, 3 Tbsp. freshly ground flaxmeal Lunch and Dinner Season sardines in water (green and white label), green salad * Swordfish steak, grilled onions, green salad with flax oil dressing * Flank steak, baked potato, green salad with flax oil dressing * Broiled red snapper, steamed broccoli, baked yams * Large mixed green salad w/ oil and lemon juice, small can of tuna, chopped yellow and sweet red pepper * Broiled mackerel, steamed broccoli, green beans or other vegetable * Beef, lentil and vegetable soup, (celery, carrots, onion, cabbage) * Chicken salad made with sugar-free mayonnaise, roasted vegetables, spinach salad * Gourmet salmon salad made with 1 can salmon, 2 tsp. sliced scallions, 1 tsp. sliced radishes, 2 tsp. Rice vinegar, 1 tsp. flax oil, 1 tsp. soy sauce, and ¼ tsp. minced ginger root, all placed atop a green salad Snacks Roasted garlic or almond butter on rice cake or celery, protein shakes with freshly ground flaxseeds added, fresh green vegetable juice, handful of raw almonds, hazelnuts, walnuts, brazil nuts, or sesame seeds, an organic apple, pear, or grapes, sugar-free yogurt, rice cakes with nut butter, hard boiled egg. 1 Program HE Heart Support Beverages Green drinks: Green Magma, Kyogreen, or Green Kamut: 1 tsp. 1-3x day in water Herbal Teas: Ginger, Cinnamon, Chamomile, Linden Tea (improves integrity of blood vessel walls), Green Tea with Cinnamon Stick Avoid Cigarette smoke (even 2 hand), sugar, refined and processed foods, hydrogenated oils, safflower, sunflower, corn oils, soft drinks, alcohol, processed meats, being overweight. Do not consume large amounts of licorice as this can lower levels of magnesium and potassium. nd Suggestions and goals The basic idea of this eating program is to increase consumption of omega 3 fats, fiber, and whole natural foods. Eliminate sugar, refined or processed foods, and hydrogenated oils. Drink plenty of pure water. Supplements Magnesium Carnitine CoQ10 Vitamin E Taurine EPA/DHA B Complex Vitamin C Zinc Lipoic Acid Selenium Creatine 500-1,000 mg (balance with potassium in diet) 500-4,000 mg (½ to 1 hour before breakfast and lunch) 100-400 mg 400-800 IUs 1-3 grams 500-2,000 mg 1-2 per day 1-3 grams 25-50 mg 100 mg 200-400 mcg 1 gram Herbs: Hawthorn (leaf, berry, and flower) Cactus grandiflorus Motherwort Collinsonia (Stone Root) 1-4 ml per day ½-2 ml per day 1-3 ml dropper per day 1-2 ml dropper per day For MVP Patients: Hypoglycemia is one of the components that so often accompanies mitral valve prolapse (MVP), and it is important to balance blood sugar well if one is to successfully treat this condition. Adequate protein, sugar avoidance, and all the other recommendations for hypoglycemia should be followed by those with MVP. Hawthorn and cactus grandiflorus are two wonderful heart strengthening herbs that are very useful in MVP. 2 Program HE Heart Support Research Review Antioxidants Cardiomyopathies are the group of diseases affecting the cardiac muscle. Although they have never been related to oxidative stress diseases, an analysis of the causes of these pathologies reveals the presence of a prooxidative agent or that the intracardiocytic balance between oxidation and antioxidation has been broken. In support of this hypothesis, we analyze the pro-oxidative factors which co-operate with other factors or by themselves to promote the development of this group of pathologies. We show also data demonstrating that the tissue and cellular damages are characteristic of an oxidative stress situation. Finally, we present evidence that in some cases of particular cardiomyopathies, the use of antioxidative strategies greatly improves the health of the patients. Therefore, we suggest that the use of antioxidants can be an alternative or complementary therapy in this group of diseases.1 Magnesium Reduced tissue magnesium stores may represent a significant risk factor for arrhythmias.2 These results suggest that intravenous magnesium sulfate may be effective in the acute management of cardiac arrhythmias in patients with a low serum iMg2+ level.3 The intricate role of magnesium on a biochemical and cellular level in cardiac cells is crucial in maintaining stable cardiovascular hemodynamics and electrophysiologic function. In patients with congestive heart failure, the presence of adequate total-body magnesium stores serve as an important prognostic indicator because of an amelioration of arrhythmias, digitalis toxicity, and hemodynamic abnormalities.4 Magnesium and Potassium The interactions of Mg and K in cardiovascular disease are diverse and complex. However, Mg deficiency and loss from the heart and arteries, caused e.g. by dietary deficiency or imbalance, or by diseases and their treatment, can contribute to cardiovascular damage, and to functional abnormalities. Although Mg deficiency interferes with K retention, it is seldom measured in routine clinical practice, and the need to correct low Mg levels, in order to replete K, is rarely considered. The heart, with its high metabolic activity, is particularly vulnerable to Mg deficiency or loss because of the importance of Mg in mitochondrial structure and enzymatic function. The need for Mg to activate Na/K ATPase has long been known. Mg has also been shown to be structurally part of the enzyme in cardiac mitochondria. Additionally, Na/K exchange occurs in association with phosphorylation and dephosphorylation, reactions that are also Mg- dependent. The demonstration that Mg modulates K+/proton (H+) exchange, and that cation selectivity in Na+ and K+ exchange for H+ is highly dependent on the concentration of Mg++, provides new insights into how Mg protects against K loss. The loss of myocardial K that results from Mg deficiency contributes to electrophysiologic changes, as can the Ca shifts of Mg loss. A high Ca/Mg ratio also predisposes to arterial spasms, and increases catecholamine release. Thus the arrhythmogenic potential of Mg deficiency can be related to imbalances between Mg and K or between Mg and Ca, or both. Electrical or K-induced catecholamine release is increased by a low Mg/Ca ratio, as are increased fatty acids and lipids and intravascular hypercoagulability. K or Ca loading of the patient with undiagnosed Mg inadequacy is not only often unsuccessful, but it may carry inherent risks. It can intensify the Mg depletion, the arterial contractility, and ECG abnormality. In the patient receiving digitalis, Mg deficiency can increase drug toxicity. In the case of myocardial infarction, Mg deficiency can increase the risk of malignant ventricular arrhythmias and sudden 3 Program HE Heart Support cardiac death. In the absence of alcoholism or gastrointestinal disease, the use of loop diuretic therapy for congestive heart failure, especially in elderly patients, is the most common cause of Mg depletion. A high concurrence of hypomagnesemia with hypokalemia, from whatever cause, has been documented. However, systemic Mg deficiency can exist despite normal Mg serum levels. Methodological difficulties hamper direct detection of cellular Mg deficiency, but patients can be indirectly evaluated by use of Mg-loading tests, which may be of combined diagnostic and therapeutic value.5 Selenium A case of selenium-deficiency myopathy, secondary to total parenteral nutrition, is presented. The literature on selenium-deficiency myopathy and cardiomyopathy is reviewed in the context of the literature concerning selenium status in numerous diseases. 6 Carnitine To evaluate the therapeutic efficacy of l-carnitine in heart failure, the myocardial carnitine levels and the therapeutic efficacy of l- carnitine were studied in cardiomyopathic BIO 14.6 hamsters and in patients with chronic congestive heart failure and ischemic heart disease. Oral administration of l-carnitine for 12 weeks significantly improved the exercise tolerance of patients with effort angina. In 9 patients with chronic congestive heart failure, 5 patients (55%) moved to a lower NYHA class and the overall condition was improved in 6 patients (66%) after treatment with l-carnitine. L-carnitine is capable of reversing the inhibition of adenine nucleotide translocase and thus can restore the fatty acid oxidation mechanism which constitutes the main energy source for the myocardium. Therefore, these results indicate that l-carnitine is a useful therapeutic agent for the treatment of congestive heart failure in combination with traditional pharmacological therapy.7 CoQ10 Over an eight year period (1985-1993), we treated 424 patients with various forms of cardiovascular disease by adding coenzyme Q10 (CoQ10) to their medical regimens. Doses of CoQ10 ranged from 75 to 600 mg/day by mouth (average 242 mg). Treatment was primarily guided by the patient's clinical response. In many instances, CoQ10 levels were employed with the aim of producing a whole blood level greater than or equal to 2.10 micrograms/ml (average 2.92 micrograms/ml, n = 297). Patients were followed for an average of 17.8 months, with a total accumulation of 632 patient years. Patients were divided into six diagnostic categories: ischemic cardiomyopathy (ICM), dilated cardiomyopathy (DCM), primary diastolic dysfunction (PDD), hypertension (HTN), mitral valve prolapse (MVP) and valvular heart disease (VHD). For the entire group and for each diagnostic category, we evaluated clinical response according to the New York Heart Association (NYHA) functional scale, and found significant improvement. Of 424 patients, 58 per cent improved by one NYHA class, 28% by two classes and 1.2% by three classes. A statistically significant improvement in myocardial function was documented using the following echocardiographic parameters: left ventricular wall thickness, mitral valve inflow slope and fractional shortening. Before treatment with CoQ10, most patients were taking from one to five cardiac medications. During this study, overall medication requirements dropped considerably: 43% stopped between one and three drugs. Only 6% of the patients required the addition of one drug. No apparent side effects from CoQ10 treatment were noted other than a single case of transient nausea. In conclusion, CoQ10 is a safe and effective adjunctive treatment for a broad range of cardiovascular diseases, producing gratifying clinical responses while easing the medical and financial burden of multidrug therapy.8 4 Program HE Heart Support Hypertrophic cardiomyopathy (HCM) is manifested by severe thickening of the left ventricle with significant diastolic dysfunction. Previous observations on the improvement in diastolic function and left ventricular wall thickness through the therapeutic administration of coenzyme Q10 (CoQ10) in patients with hypertensive heart disease prompted the investigation of its utility in HCM. Seven patients with HCM, six non-obstructive and one obstructive, were treated with an average of 200 mg/day of CoQ10 with mean treatment whole blood CoQ10 level of 2.9 micrograms/ml. Echocardiograms were obtained in all seven patients at baseline and again 3 or more months post-treatment. All patients noted improvement in symptoms of fatigue and dyspnea with no side effects noted. The mean interventricular septal thickness improved significantly from 1.51 +/- 0.17 cm to 1.14 +/- 0.13 cm, a 24% reduction (P 0.002). The mean posterior wall thickness improved significantly from 1.37 +/- 0.13 cm to 1.01 +/- 0.15 cm, a 26% reduction (P 0.005). Mitral valve inflow slope by pulsed wave Doppler (EF slope) showed a non-significant trend towards improvement, 1.55 +/- 0.49 m/sec2 to 2.58 +/- 1.18 m/sec2 (P 0.08). The one patient with subaortic obstruction showed an improvement in resting pressure gradient after CoQ10 treatment (70 mmHg to 30 mmHg).9 Taurine We compared the effect of oral administration of taurine (3 g/day) and coenzyme Q10 (CoQ10) (30 mg/day) in 17 patients with congestive heart failure secondary to ischemic or idiopathic dilated cardiomyopathy, whose ejection fraction assessed by echocardiography was less than 50%. The changes in echocardiographic parameters produced by 6 weeks of treatment were evaluated in a double-blind fashion. In the taurine- treated group significant treatment effect was observed on systolic left ventricular function after 6 weeks. Such an effect was not observed in the CoQ10-treated group.10 Omega 3 Fats and Arrhythmias Interest in the potential cardiovascular benefits of omega-3 long chain polyunsaturated fatty acids has been largely focused on possible antiatherothrombotic effects. In addition, however, definitive antiarrhythmic effects of these dietary omega-3 fatty acids have been reported by Charnock & McLennan. Our studies commenced with the observation that two of these fatty acids, eicosapentaenoic (C20:5n-3, EPA) and docosahexaenoic acid (C22:6n-3, DHA) prevented contracture and fibrillation of isolated neonatal cardiac myocytes when exposed to toxic levels of ouabain (0.1 mM). This protection was associated with prevention of excessively high intracellular calcium concentrations in the myocyte. Further, it was shown that these fatty acids modulate calcium currents through L-type calcium channels and that the effect occurs within a few minutes of adding EPA or DHA to the medium perfusing the cultured cardiac myocytes. Infusing an emulsion of the omega-3 fatty acids intravenously just prior to compression of a coronary artery in a conscious, prepared dog will prevent the expected subsequent ischemia-induced ventricular fibrillation.11 Hawthorn Hawthorn (crataegus) has been used since antiquity for medicinal purposes. More recent research suggests it to be useful in congestive heart failure. Rigorous clinical trials show benefit concerning objective signs and subjective symptoms of congestive heart failure stage NYHA-II. No adverse drug reactions have been reported. It is therefore concluded that crataegus is an effective and safe therapeutic alternative for this indication.12 5 Program HE Heart Support 1. Romero-Alvira D, Roche E, Placer L. Cardiomyopathies and oxidative stress. Med Hypotheses 1996;47(2):137-44. 2. Haigney MC, Berger R, Schulman S, et al. Tissue magnesium levels and the arrhythmic substrate in humans. J Cardiovasc Electrophysiol 1997;8(9):980-6. 3. Kasaoka S, Tsuruta R, Nakashima K, et al. Effect of intravenous magnesium sulfate on cardiac arrhythmias in critically ill patients with low serum ionized magnesium [published erratum appears in Jpn Circ J 1997 Oct;61(10):886]. Jpn Circ J 1996;60(11):871-5. 4. Douban S, Brodsky MA, Whang DD, Whang R. Significance of magnesium in congestive heart failure. Am Heart J 1996;132(3):664-71. 5. Sheehan JP, Seelig MS. Interactions of magnesium and potassium in the pathogenesis of cardiovascular disease. Magnesium 1984;3(4-6):301-14. 6. Marcus RW. Myopathy and cardiomyopathy associated with selenium deficiency: case report, literature review, and hypothesis. Md Med J 1993;42(7):669-74. 7. Kobayashi A, Masumura Y, Yamazaki N. L-carnitine treatment for congestive heart failure--experimental and clinical study. Jpn Circ J 1992;56(1):86-94. 8. Langsjoen H, Langsjoen P, Willis R, Folkers K. Usefulness of coenzyme Q10 in clinical cardiology: a longterm study. Mol Aspects Med 1994;15(Suppl):s165-75. 9. Langsjoen PH, Langsjoen A, Willis R, Folkers K. Treatment of hypertrophic cardiomyopathy with coenzyme Q10. Mol Aspects Med 1997;18(Suppl):S145-51. 10. Azuma J, Sawamura A, Awata N. Usefulness of taurine in chronic congestive heart failure and its prospective application. Jpn Circ J 1992;56(1):95-9. 11. Leaf A. Omega-3 fatty acids and prevention of ventricular fibrillation. Prostaglandins Leukot Essent Fatty Acids 1995;52(2-3):197-8. 12. Weihmayr T, Ernst E. [Therapeutic effectiveness of Crataegus]. Fortschr Med 1996;114(1-2):27-9. 6