* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Auditory system
Survey
Document related concepts
Transcript
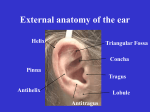
Auditory system Organ of hearing Auditory systems is an engineering masterpiece Size of a pea Detects vibrations as small as the size of an atom Responds 1000 times faster than the visual photoreceptors Much of human communications is mediated by the auditory system, including music Role of Audition in Behavior Language Localization of a sound source in the absence of visual cues Species-specific vocalizations Prosody – emotional content of language Appreciation of music Periodic condensation and rarefaction of air molecules are detected by the auditory system Complex sounds can be broken down into the fundamental frequency components Sound = pressure waves generated by vibrating air molecules Waveform (amplitude/time) Phase Amplitude (dB) Frequency (Hz) – spectrum 20 Hz to 20 kHz Flow of information External and middle ears collect sound waves and amplify their pressure Sound energy in the air is transmitted to the fluidfilled cochlea of the inner ear In inner ear a series of biomechanical processes break up the signal into simpler sinusoidal components Frequency, amplitude, phase of the original signal are all faithfully transduced by the sensory cells and encoded by the electrical activity of nerves Several levels of central processing in CNS Major components of the ear External (outer) ear, auris externa Middle ear, auris media auricle (pinna) external acoustic meatus (ear canal) tympanic membrane (ear drum) tympanic cavity auditory (eustachian) tube auditory ossicles Internal (inner) ear, auris interna - auditory and vestibular portions osseous labyrinth membranous labyrinth Ear overview – 3 components Major components of the ear (Lat. auris) External ear – auricle (pinna) Tuberculum Tragus Antihelix Helix Antitragus Lobulus Thin skin with fine hairs Elastic fibrocartilage Lobule of auricle Auricular tubercle (of Darwin) Ligaments of auricle extrinsic (connect the auricle with the temporal bone) and intrinsic (connect individual auricular cartilages) External ear – muscles M. auricularis sup. M. helicis major M. auricularis ant. M. helicis minor M.antitragicus M.tragicus Extrinsic auricular muscles - auriculares anterior, superior and posterior Intrinsic auricular muscles - helicis major and minor, tragicus, antitragicus, transversus auriculae and obliquus auriculae Innervation - CN VII External ear – blood supply External ear – sensory innervation External ear – external acoustic meatus Cartilaginous part – outer (~8 mm long), Osseous part – inner (~16 mm long), Thin skin; the thicker cerumen-producing ear canal Skin has fine hairs, tragi Sebaceous glands in the hair follicles Ceruminous glands ear wax, cerumen Conductive hearing loss Occlusion of the auditory canal by cerumen The tip of a water-filled syringe is placed just inside the ear canal, and a stream of warm water is instilled into the canal to remove earwax. Middle ear Function - sound conduction apparatus Components tympanic membrane tympanic cavity auditory (eustachian) tube auditory ossicles Tympanic membrane Separates the tympanic cavity from the external acoustic meatus Diameter 10-11 mm longest/8-9 mm shortest Parts pars flaccida (Schrapnell’s membrane) pars tensa → umbo Layers cuticular layer - continuous with the thin skin of the meatus (keratinized) fibrous layer – absent in pars flaccida radiate fibers circular fibers mucous layer - part of the mucosa of the tympanic cavity (single layer of flat cells, no ciliated cells Otoscopic appearance of the right tympanic membrane Tympanic membrane Otoscope The inner surface of the membrane is convex and the point of greatest convexity is termed the umbo Conductive hearing loss Damage to the tympanic membrane perforation of the tympanic membrane this ear drum has a 20% perforation in the posterior portion of this right ear drum this hole would usually be repaired with a graft placed under the ear drum...an operation called a tympanoplasty Mainly innervated by the auriculotemporal nerve, and appears to perceive only pain Conductive hearing loss Otitis media inflammation of the middle ear cleft immobile tympanic membrane, which can be dull, opaque, red, bulging, or even show pus through it a demonstrable conductive hearing loss Tympanic cavity – 1.5 cm3, air-filled Epitympanic recess (the attic) - above the level of the membrane, which contains the upper half of the malleus and most of the incus Tympanic cavity proper (mesotympanum) opposite the tympanic membrane Hypotympanum (hypotympanic recess) – connected to the eustachian tube Tympanic cavity – 6 walls Lateral wall – paries membranaceus Medial wall – paries labyrinthicus Superior wall, roof – paries tegmentalis tegmen tympani → otogenic meningitis Inferior wall, floor – paries jugularis membrana tympani et recessus epitympanicus canaliculus tympanicus Anterior wall – paries caroticus Posterior wall – paries mastoideus antrum mastoideum Tympanic cavity Course of facial nerve in the tympanic cavity medial Chorda tympani lateral Course of chorda tympani nerve Brain is in proximity to the cells of the temporal bone → infection propagation Auditory (Eustachian, pharyngotympanic) tube Connects middle ear with nasopharynx Ventilates middle ear and air cells Equalizes pressure between middle ear & atmosphere Drains middle ear spaces Creates a barrier to ascending infection (more horizontal and shorter in infants) cartilaginous part - – 24 mm bony part - – 12 mm Middle ear - ossicles Malleus (Lat., hammer) - the largest, 8-9 mm long Incus (Lat., anvil) head, caput mallei neck, collum mallei handle, manubrium mallei anterior and lateral processes body, corpus incudis long process, crus longum lenticular process short process, crus breve Stapes (Lat., stirrup) head, caput stapedis limbs (crura) – anterior & posterior base, basis stapedis Middle ear – ligaments & joints body of incus long limb Conductive hearing loss Otosclerosis a bony ankylosis (knee) knits the bone of the middle ear to the stapes, preventing normal transmission of sound from the eardrum into the inner ear Importance of middle ear for hearing External ear airborne environment Low impedance Middle Ear Avoid reflection Air-fluid boundary Inner ear aqueous environment High impedance Because of the marked difference in elasticity and density between air and fluid, almost 99% of acoustic energy is reflected back at the air-fluid interface between the middle ear and inner ear Middle ear ensures transmission of the sound energy across the air–fluid boundary by boosting the pressure measured at the tympanic membrane almost 200-fold by the time it reaches the inner ear Middle ear - muscles Stapes - stapedius muscle – CN VII Malleus - tensor tympani muscle – CN V Reflexively activated by loud noise Protection against loud noise damage Stapedius & tensor tympani muscles tendon of tensor tympani m. tensor tympani m. stapedius tendon of stapedius Stapedius & tensor tympani muscles tendon of tensor tympani tendon of stapedius The stapedius reflex Hyperacusis Definition abnormal sensitivity to everyday sound levels or noises, often sensitivity to higher pitched sounds, in the presence of essentially normal hearing Cause damage to the nerve to the stapedius or the stapedius muscle, thereby causing faulty amplification of sounds Meneire’s Note: innervated by VII, IX, and X cerumen, foreign bodies otitis media, otosclerosis Meniere’s disease Inner ear Located within the petrous portion of the temporal bone Contains 2 systems of canals or cavities osseous (bony) labyrinth - protective “capsule” membranous labyrinth (within bony) - “working” part Location of labyrinth within the petrous portion of the temporal bone anterior medial lateral posterior Bony vs membranous labyrinth Bony labyrinth Membranous labyrinth Semicircular canals Semicircular ducts Vestibulum Sacculus (anterior cavity) → cochlear duct Utriculus (posterior cavity) → semicircular ducts Cochlea Cochlear duct Perilymph Endolymph bony Components of the labyrinth membranous sensory Perilymph vs endolymph Bony labyrinth – perilymph similar in ionic composition to cerebrospinal fluid and extracellular fluid of other tissues, but contains little protein emerges from the microvasculature of the periosteum and is drained by a perilymphatic duct into the adjoining subarachnoid space suspends and supports the closed membranous labyrinth, protecting it from the hard wall of the bony labyrinth Membranous labyrinth – endolymph high K+ (150 mM) and low Na+ (16 mM) similar to intracellular fluid generated largely by capillaries in the stria vascularis in the wall of the cochlear duct drained from the vestibule into venous sinuses of the dura mater by the small endolymphatic duct Inner ear fluids Na+ K+ mEq/l mEq/l MM g/l Perilymph 140 5 0.68 200 Endolymph 5 150 0.023 30 Ca++ Protein Plasma 145 4 2.6 4300 CSF 140 3 1.2 30 The membranous labyrinth includes the sense organs for equilibrium & hearing Organs for the sense of equilibrium and balance Saccule → macula Utricle → macula Semicircular ducts → crista ampullaris in ampulla Organ for the sense of hearing Cochlea Liquor of inner ear Endolymphatic duct Perilymphatic duct Components of the labyrinth Cochlea (L., snail) 35 mm in length Makes 2⅓ two-and-one-half turns around a bony core – modiolus Modiolus contains blood vessels and surrounds the cell bodies and processes of the acoustic branch of CN VIII in the cochlear (spiral) ganglion Modiolus (Lat., Modiolus & cochlear nerve Spaces of Cochlea Scala vestibuli - perilymph Scala media (cochlear duct) - endolymph Scala tympani - perilymph Scala vestibuli and scala tympani are in reality one long tube, beginning at the oval window and ending at the round window. They communicate at the apex of the cochlea via an opening known as the helicotrema. 2 membranes separate scala media from the other compartments (vestibular) basement membrane with simple squamous epithelium on each side Organ of hearing thick basal lamina zona arcuata zona pectinata Although the cochlea narrows from base to apex, the basilar membrane widens toward the apex. The helicotrema is the continuity between the scala vestibuli and the scala tympani. Cross-section through cochlea = Scala media Stria vascularis Epithelium responsible for production and maintenance of the endolymph for the entire membranous labyrinth Encloses a network of capillaries Cells with many deep basal infoldings of their plasma membranes → numerous mitochondria Fluid and K+ ions pumped from the capillaries by the epithelial cells are released in the cochlear duct Reissner’s (vestibular membrane) Stria vascularis Spiral prominence Stria vascularis & disease CONGENITAL HEARING LOSS Derived from ectoderm, neural crest cells and mesenchyme Failure of NC migration results in absence of endolymph production Hair cells don’t survive Spiral organ (organ of Corti) Organ of Corti = sensory + supporting cells (~150 µm wide) The site of mechanochemical transduction Hair cells ~16,000/cochlea Kandel, Schwartz, Jessell; Principles of Neural Science, 4th ed. Hair cells – auditory receptor cells Outer hair cells (OHC) – in 3 rows Inner hair cells (IHC) – in 1 row Hair cells – 1 Kinocilium + 30 stereocilia K Functions of kinocilia are unclear, they disappear shortly after birth in mammals Kandel, Schwartz, Jessell; Principles of Neural Science, 4th ed. Links between stereocilia Current Opinion in Neurobiology Volume 12, Issue 4 , 1 August 2002, Pages 380-386 Stereocilia contain actin filaments Supporting cells of the organ of Corti Pillar cells - filled with tonofibrils; converge to form the fluid-filled tunnel of Corti Phalangeal (Deiters') cells – support IHC & OHC Hensen’s cells – columnar cells, outer to the outer phalangeal cells; outer border of the organ of Corti Border cells (inner side) & Claudius cells (outer side) – form external borders of the organ of Corti Tectorial membrane Gelatinous structure with embedded filamentous elements. It extends over the free surface of the organ of Corti. The hairs of the hair cells are attached to it. Relations between phalangeal & hair cells Outer phalangeal cells have processes → OHC Inner phalangeal cells do not have processes → IHC Bony cochlea vestibulum H – helicotrema M – modiolus SG – spiral ganglion VN – n.vestibulocochlearis FN – facial nerve OC – organ of Corti SV – scala vestibuli ST – scala tympani CD – cochlear duct AO – auditory ossicle А – ampulla of a semicircular canal CA – crista ampullaris Bony cochlea limbus spiralis scala vestibuli tectorial membrane vestibular membrane cochlear duct stria vascularis Lamina spiralis ossea ganglion spirale Organ of Corti prominentia spiralis Fibers of cochlear nerve scala tympani basilar membrane Lig. spirale epithelium Bony cochlea Organ of Corti sulcus spiralis ext. cuniculus Cells of Claudius Cells of Hansen Outer hair medius cells (Nuel) sulcus spiralis int. tectorial membrane Inner hair cell Border cell cuniculus ext. limbus spiralis Internal sulcus cells cuniculus med. (Nuel) Fibers of cochlear nerve Tunnel of Corti Lig. spirale Cells of Boettcher basilar membrane Outer Outer pillar phalangeal cell cells (Deiters) Inner pillar cell Inner phalangeal cells Lamina spiralis ossea Basilar membrane is displaced by energy (sound) waves from the stapes Basilar membrane Basilar membrane displacement is converted into electrical signals by the organ of Corti Mechanoelectrical transduction Changes in sound waves Basilar membrane vibrations Ion Channels open Depolarization Action potential Mechanoelectrical transduction & hair cells Drug-induced damage to hair cells Some antibiotics damage OHCs Hearing abnormalities produced by antibiotics is a consequence of damage to the cochlear amplifier Hair cells are innervated by the spiral ganglion 30,000 bipolar neurons Receptors of sensory systems - primary sensory neurons pseudounipolar part of PNS (except jaw proprioception) bipolar part of CNS Nerve supply to hair cells 90% of spiral ganglion neurons (type I cells) innervate IHC 10% of spiral ganglion neurons (type II cells) innervate OHC each fiber diverges to innervate many OHC each IHC receives contacts from about 10 fibers; each fiber contacts only 1 IHC Efferent fibers to hair cells originate in the contralateral superior olive in the pons and and terminate on OHC and the afferent terminal boutons innervating IHC. Efferent fibers have an inhibitory effect on auditory stimuli. Types of hearing loss Conductive hearing loss - various problems in the middle ear which can reduce conduction of vibrations by the chain of ossicles from the tympanic membrane to the oval window Sensorineural hearing loss – is due to defects in any structure or cell from the cochlea to auditory centers of the brain, but commonly involves loss of hair cells or nerve degeneration (can be congenital or acquired) Patients with severe sensorineural deafness may be helped by cochlear implants prosthetic electrode array Basilar membrane is the mechanical analyzer of sound - tonotopy A traveling wave is shown at a given instant along the cochlea, which has been uncoiled. The graphs profile the amplitude of the traveling wave along the basilar membrane for different frequencies and show that the position where the traveling wave reaching its maximum amplitude varies directly with the frequency of stimulation. Auditory system Spiral Ganglion Cranial Nerve VIII Dorsal Cochlear Nuc Cochlear Nucleus Superior Olivary Nuc Lateral Lemniscus Ventral Cochlear Nuc Origin: Course: Termination: Laterality: Spiral ganglion CNVIII, auditory pathway, auditory cortex Auditory Cortex (Heschl’s gyrus) BA 41,42 Bilateral Inferior Colliculus Medial Geniculate Auditory Cortex Auditory system Superior Olivary Nuc Lateral Lemniscus Origin: Course: Termination: Laterality: Spiral ganglion CNVIII, auditory pathway, auditory cortex Auditory Cortex (Heschl’s gyrus) BA 41,42 Bilateral Superior olivary complex → sound localization MSO = medial superior olive Purves, et al, Neuroscience, 3rd ed. Auditory system Lateral Lemniscus Origin: Course: Termination: Laterality: Spiral ganglion CNVIII, auditory pathway, auditory cortex Auditory Cortex (Heschl’s gyrus) BA 41,42 Bilateral Auditory system Inferior Colliculus Lateral Lemniscus Origin: Course: Termination: Laterality: Spiral ganglion CNVIII, auditory pathway, auditory cortex Auditory Cortex (Heschl’s gyrus) BA 41,42 Bilateral Auditory system Brachium of Inferior Colliculus Origin: Course: Termination: Laterality: Spiral ganglion CNVIII, auditory pathway, auditory cortex Auditory Cortex (Heschl’s gyrus) BA 41,42 Bilateral Auditory system Medial Geniculate Nucleus Origin: Course: Termination: Laterality: Spiral ganglion CNVIII, auditory pathway, auditory cortex Auditory Cortex (Heschl’s gyrus) BA 41,42 Bilateral Auditory system – area A1 (A-I) Transverse gyri of Heschl Central auditory pathways bilaterality Purves, et al, Neuroscience, 3rd ed. Auditory system - overview Modality: Modality: Auditory AuditorySensation Sensation(Hearing) (Hearing) Receptor: Receptor:Organ Organof ofCorti Cortiof ofCochlear CochlearDuct Duct Cranial -cochlear CranialNerve: Nerve:VIII VIII-cochlear 1st 1st Neuron: Neuron:Spiral SpiralGanglion Ganglion 2nd 2ndNeuron: Neuron:Cochlear CochlearNucleus, Nucleus,Ventral Ventral&&Dorsal Dorsal dorsal, dorsal,intermediate intermediateand andventral ventralacoustic acousticstriae striae trapezoid trapezoidbody body lateral laterallemniscus lemniscus 3rd 3rd Neuron: Neuron:Inferior InferiorColliculus Colliculus brachium brachiumof ofinferior inferiorcolliculus colliculus 4th 4th Neuron: Neuron:Medial MedialGeniculate GeniculateNucleus Nucleus(MG) (MG) auditory auditoryradiation radiation Termination: Termination:Primary PrimaryAuditory AuditoryArea Area(A (AI)I) Brodmann Brodmannarea area41, 41,42 42 Auditory Pathways A. spiral ganglion B. dorsal and ventral cochlear nucleus C. inferior colliculus D. medial geniculate nucleus E. Primary auditory area F. superior olivary nucleus G. nucleus of lateral lemniscus 1. acoustic striae & trapezoid body 2. lateral lemniscus 3. brachium of inferior colliculus 4. auditory radiation 5. commissure of inferior colliculus VIIIc. cochlear division Auditory pathways – 3D Primary auditory cortex – A I The Auditory Cortex Purves, et al, Neuroscience, 3rd ed. Tonotopic organization is maintained along the entire auditory pathway Tonotopic organization is maintained along the entire auditory pathway Purves, et al, Neuroscience, 3rd ed. Auditory cortex Tonotopic (cochleotopic) organization Binaural properties of cortical neurons Wernicke’s area, next to A1, is for the comprehension of speech Probably as we move into auditory association areas - neurons that respond to complex sounds and species-specific vocalizations (Grandma’s voice…) Lesion localizing BECAUSE OF HEAVY CALLOSAL CONNECTIONS, A UNILATERAL LESION OF THE AUDITORY CORTEX PATHWAYS DISTAL TO THE COCHLEAR NUCLEI WILL RESULT IN VIRTUALLY NO LOSS OF HEARING THE PATIENT WILL MOST LIKELY EXPERIENCE AN IMPAIRMENT IN THE ABILITY TO LOCALIZE THE DIRECTION AND DISTANCE OF SOUNDS Sound Localization – 2 Cues Time cues – Low frequency sounds (below 3 KHz) are localized due to interaural time differences, capitalizing on the phase-locking abilities of primary afferent fibers. Achieved by the medial superior olive (MSO). Intensity cues – High frequency sounds (above 3 KHz) are localized due to interaural intensity differences. The head creates an acoustic shadow. Achieved by the lateral superior olive (LSO). INTERAURAL TIME DELAY AS A CUE TO THE LOCATION OF SOUND (a) Sound waves coming from the right side reach the right ear first, and there is a large interaural delay before the sound propagates to the left ear. (b) If the sound comes from straight ahead, there is no interaural delay. Delays for three directions are shown. Interaural time differences - MSO Illustration of how the MSO computes the location of a sound by interaural time differences. A given MSO neuron responds most strongly when the two inputs arrive simultaneously, as occurs when the contralateral and ipsilateral inputs precisely compensate (via their different lengths) for differences in the time of arrival of a sound at the two ears. They systematic (and inverse) variation in the delay lengths of the two inputs creates a map of sound location: in this model E would be most sensitive to sound located to the left, and A to sound from the right; C would respond best to sounds coming from directly in front of the listener. Higher-order cortical auditory areas “Where” pathway “What” pathway “What” & “Where” are processed separately Inner ear development The rudiments of the internal ears appear shortly after those of the eyes as two patches of thickened surface epithelium, the otic placodes, lateral to the hindbrain Carnegie stage 12 – ~day 27 Late 4th – early 5th week Otic pit By the time the anterior neuropore closes, the first and second pharyngeal arches are evident The regions between the pharyngeal arches are termed pharyngeal clefts. The indentation just dorsal to the second pharyngeal cleft is the developing inner ear, the otic pit. Otic pit Later ear development Carnegie stage 21 – ~day 53 Derivatives of the pharyngeal pouches Some of the neural crest cells in each of the arches become cartilage Otic vesicle & pinna development CRL External ear development