* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Evaluation of current methods performing in Preimplantation Genetic
Behavioural genetics wikipedia , lookup
Koinophilia wikipedia , lookup
Heritability of IQ wikipedia , lookup
X-inactivation wikipedia , lookup
Population genetics wikipedia , lookup
Human–animal hybrid wikipedia , lookup
Neocentromere wikipedia , lookup
Molecular Inversion Probe wikipedia , lookup
Genetic engineering wikipedia , lookup
History of genetic engineering wikipedia , lookup
Human genetic variation wikipedia , lookup
Genetic testing wikipedia , lookup
Medical genetics wikipedia , lookup
Microevolution wikipedia , lookup
Public health genomics wikipedia , lookup
Genome (book) wikipedia , lookup
Hybrid (biology) wikipedia , lookup
Designer baby wikipedia , lookup
Evaluation of PGD-AS methods- 1 -
Evaluation of Current Biopsy Methods performing in Preimplantation Genetic
Diagnose for Aneuploid Screening
Yin XueFeng
School of Basic Medical Science
Peking University
Professor Zhang Wei
Academic English Writing
June 10, 2007
Evaluation of PGD-AS methods- 2 -
Abstract
During the past decade, new techniques emerged rapidly in the preimplantation
genetic diagnose for aneuploid screening. The strengths and limitations of these PGD
protocols, is demonstrated by experiments and clinical cycles. By reviewing the
recent studies in this field, this paper briefly clarified the procedure and functions of
preimplantation genetic screening, introduced and evaluated several methods of
biopsy and then recommended the combination of approaches for further implement:
comparative genetic hybridization on first polar body and fluorescence in situ
hybridization in metaphase Ⅱoocyte .
Keywords: preimplantation genetic diagnose/aneuploidy screening/ comparative
genetic hybridization/ fluorescence in situ hybridization
Evaluation of PGD-AS methods- 3 -
Evaluation of PGD-AS methods
According to the data reported by European Society of Human Reproduction
and Embryology (Sermon, Moutou et al. 2005), preimplantation genetic diagnose for
aneuploid screening (PGD-AS) cycles have increased significantly during the past
several years. The advent of commercially available probes labeled with more
different fluorochromes (Committee 2002) and the common occurrence of infertility
related to aging in woman due to several social factors(Platteau, Staessen et al. 2005;
Van Voorhis 2007) have led to its possibilities and spreading. In PGD-AS, the
chromosomes is checked and the chromosomally normal embryos are selected to
transfer, aiming to increase the pregnancy rates in in vitro fertilization (IVF) patient
groups with a poor prognosis (Kahraman, Bahce et al. 2000; Gutierrez-Mateo, Benet
et al. 2005; Sermon, Moutou et al. 2005).
In the same time, new techniques are continually introducing into this field to
enhance the outcome. Various studies have identified the benefits and limitations of
these methods, either by conducting experiments or by collecting clinical data.
However, an integrated evaluation of the method and corresponding recommendation
on implication was still in lack. Based on the recent progress in this area, this paper
aimed to demonstrate the feature of several PGD-AS protocols currently adapted,
evaluating their performance, and indicate the alternative method that manifest the
predominance.
Introduction of PGD-AS
Aneuploidy occurrence
Evaluation of PGD-AS methods- 4 -
The incidence of chromosomal abnormalities in embryos varies greatly in
different published studies, mainly depending on the number of chromosomes being
investigated and the methods taken(Staessen, Platteau et al. 2004; Gutierrez-Mateo,
Benet et al. 2005). As generally believed, aneuploidy results from two mechanisms:
non-disjunction of bivalents and premature separation of sister chromatids. Both
mechanisms
can
operate
on
one
cell
and
causing
missing
or
extra
chromosome(Gutierrez-Mateo, Benet et al. 2004).
The embryo with aneuploidy usually gains a much lower implantation and
pregnancy rate, proving by the fact that much higher rate of aneuploidy is found in
blastocyst than in spontaneous aborted and live born fetus(Leeanda Wilton 2001).
This may be explained by the negative self-selection against chromosomal
abnormalities in the blastocyst stage of embryonic development that the aneuploidy
cells are undergoing programmed cell death (apoptosis) or its key functions
maintaining nuclear organization is altered(Kahraman, Bahce et al. 2000; Dagan
Wells 2002; Staessen, Platteau et al. 2004). This is proved by the observation that
chromosomes in aneuploid cells have significantly peripheral localization compared
with chromosomally normal ones (McKenzie, Carson et al. 2004; Diblik, Macek et al.
2005).
Function of PGD-AS
As aneuploidy are one of the major causes of early embryo wastage
(Gutierrez-Mateo, Benet et al. 2005), PGD-AS, which prevent the aneuploidy cells
from being transferred, naturally have the effect of increase pregnancy rate. In the
Evaluation of PGD-AS methods- 5 -
published studies, the majority report significant improvements in implantation rate
and reduction in abortion rate after PGD-AS patients compared with a matched
control group(Munne, Magli et al. 1999; Munne, Chen et al. 2005; Platteau, Staessen
et al. 2005; Munne, Fischer et al. 2006). In the study of Staessen (2004) no significant
difference is observed, probably owing to improper manipulation.
In addition, PGD-AS is capable of reducing rate of multiple gestations, which is a
severe complication of IVF. To gain a higher rate of pregnancy, usually more than one
embryo is transferred in IVF, thus links to a much higher risk of the multiple
gestations (Committee 2002; Sermon, Moutou et al. 2005) which brings much danger
to infant health. In this circumstance], PGD-AS manifests its advantage of indicating
the suitable embryos to transfer and hence significantly reduce the number of embryos
to be transferred while keeping the same pregnancies rate(Santiago Munné and Cohen
2003; Staessen, Platteau et al. 2004).
Adaptive patients
The occurrence rate of aneuploid is significantly high in two group of people:
advanced maternal age (AMA) and recurrent IVF failure (RIF), who are therefore
suggested to perform PGD-AS treatment(Thornhill, deDie-Smulders et al. 2005). It
has been widely demonstrated that AMA is related with increased aneuploidy rates in
oocytes and embryos and thus correlated with reduced implantation and a high
abortion rate(Santiago Munné and Cohen 2003; Staessen, Platteau et al. 2004). This
maybe
attributed
to
reduced
endometrial
receptivity
or
reduced
oocyte
quality(Kahraman, Bahce et al. 2000) The latter is considered to be the more
Evaluation of PGD-AS methods- 6 -
influential(Santiago Munné and Cohen 2003), supported by the fact that with a donor
oocyte, the AMA couples may achieve successful pregnancy(Van Voorhis
2007)..Repetitive clinical pregnancy looses has been attributed to a host of anatomic,
endocrine and immunological causes(Munne, Chen et al. 2005).While the mechanism
is still lie in uncertainty, a preponderant genetic role is expected (McKenzie, Carson et
al. 2004).
Methods of PGD-AS
Methods adopted
The genetic analysis has been performed using several techniques, consists of
conventional
karyotyping,
microwave
hybridization(Bahce,
Escudero
et
al.
2000)R-banding(Gutierrez-Mateo, Wells et al. 2004), G-banding(Dagan Wells
2002),spectral karyotyping (SKY)(Gutierrez-Mateo, Gadea et al. 2005), fluorescence
in situ hybridization (FISH)(Kahraman, Bahce et al. 2000; Staessen, Platteau et al.
2004; Diblik, Macek et al. 2005; McArthur, Leigh et al. 2005; Munne, Chen et al.
2005; Platteau, Staessen et al. 2005), multiplex fluorescence in situ hybridization
(M-FISH), comparative genomic hybridization (CGH)(Dagan Wells 2002),
centromere specific multiplex fluorescence in situ hybridization (cenM-FISH)
(Gutierrez-Mateo, Benet et al. 2005), fluorescence in situ hybridization on three
dimensionally preserved nuclei (3D-FISH)(Irina Solovei 2002).
It is worthy noting there is still large variety among the same kind of techniques.
It mainly depends on the specific protocol of each laboratory, including the embryo
culture medium, the day and number of the cell removal(Cohen and Munne 2005), the
Evaluation of PGD-AS methods- 7 -
condition of manipulation. All these may impact the outcome of the PGD-AS, but the
exact quantity is unavailable, so that it may only be count into stochastic error.
FISH
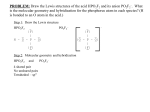
Fluorescence in situ hybridization study has the broadest application at present,
figure 1 shows a sample outcome of FISH. As the technique is well developed, there
are commercially available probes and detailed guidelines for implication. However
FISH has a severe limitation that only 5-9 of the whole 23 karyotype can be analyzed
simultaneously, as accuracy per probe is reduced when large numbers of the probes
are combined(Dagan Wells 2002; Gutierrez-Mateo, Wells et al. 2004). Thus the
analysis of only some selected chromosomes may underestimate the real aneuploidy
rate of human oocyte(Kahraman, Bahce et al. 2000; McKenzie, Carson et al. 2004;
Staessen, Platteau et al. 2004). For example, in a study by Gutierrez-Mateo, Benet et
al.(Gutierrez-Mateo, Benet et al. 2005), as high as 30% of the aneuploidy doublets
would have been incorrectly diagnosed as normal using current PGD panels which
includes nine chromosomes that are considered to be most frequently involved in
aneuploidy.
To overcome this defect, a new technique, cenM-FISH has been introduced,
which can analyze the full set of chromosomes simultaneously. But it cannot analyze
the interphase cells like blastomeres due to high risk of overlapping signals
(Gutierrez-Mateo, Benet et al. 2005), thus the feasible application is fatally restricted.
Evaluation of PGD-AS methods- 8 -
Figure 1 The outcome of Fluorescence in situ hybridization. Arrows indicate
signals for each chromatid. Adapted from "Aneuploidy study of human
oocytes first polar body comparative genomic hybridization and metaphase II
fluorescence in situ hybridization analysis." by Gutierrez-Mateo, C., J. Benet,
et al., Hum. Reprod. 19(12): 2859-2868.
Like SKY and other methods, FISH depends on the spreading of chromosome
material on slides, which brings about problems as overlapping chromosomes,
excessive spreading and artefactual loss of chromosomes(Gutierrez-Mateo, Benet et al.
2005; Platteau, Staessen et al. 2005). The former two provide non-interpretable biopsy
outcome, thus reduce the overall efficiency to a large extent. Artefactual loss is
difficult to be distinguished from real hypohaplodies and leads to incorrect outcome.
An additional defect is that the prevalence of chromosomal mosaicism may hurt
the accuracy of biopsy. The rate of mosaicism in cleavage stage is comparatively high
(Staessen, Platteau et al. 2004), thus retrieving one cell from blastomere may not
represent the integrate genetic status of the embryo and give erroneous information
(Gutierrez-Mateo, Benet et al. 2004; McKenzie, Carson et al. 2004). While removal
of two cells may harm the embryo beyond repair
One redeeming strategy is using material other than blastomere cell, including polar
bodies and blastocyst. But it is not appropriate for FISH analysis of polar body which
is very small and accordingly requires very high level of skill in fixation (Kokkali,
Vrettou et al. 2005). And biopsy of the embryos at blastocyst stage need
cryopreservation which may reduce the vitality of embryo (McArthur, Leigh et al.
Evaluation of PGD-AS methods- 9 -
2005; Thornhill, deDie-Smulders et al. 2005).
CGH
Comparative genomic hybridization is a molecular cytogenetic technique that
allows the analysis of the full set of chromosomes in single cell. Figure 2 is a sample
outcome of CGH, providing information of complete karyotype. Unlike other
techniques of karyotyping that work only with very well spread metaphase
chromosomes, CGH is a DNA based method that doesn’t involve cell fixation. These
are the two significant advantages of CGH. (Gutierrez-Mateo, Benet et al. 2004).
Figure 2 The outcome of Comparative Genomic Hybridyzation. Adapted from
"Aneuploidy study of human oocytes first polar body comparative genomic
hybridization and metaphase II fluorescence in situ hybridization analysis." by
Gutierrez-Mateo, C., J. Benet, et al., Hum. Reprod. 19(12): 2859-2868.
The major disadvantage of CGH is that the time needed to perform the procedure
precludes its clinical application. To get implanted, the embryos needed to be
Evaluation of PGD-AS methods- 10 -
transferred to the ovary at day 4 of fertilization, while the blastomere can only be
removed on day 3, leaving 24 hours for diagnose. But CGH is a labor intensive
technique that requires as many as 4 to 5 days obtaining results. To overcome problem
generally three strategies is introduced.
The first involves cryopreservation, in which embryos are biopsied and then
frozen, allowing as much time as CGH analysis needed. However the
freezing-thawing process diminishes the embryos vitality to a great extent and reduce
the implantation potential by 30 percents(Elias 2001; Leeanda Wilton 2001;
Gutierrez-Mateo, Wells et al. 2004) therefore should be avoided.
The second is developing better protocols and reducing the time of biopsy. In the
study of Dagan Wells (2002), an accelerated CGH protocols produces the outcome
within 30 hours but it is uncertain to generalize.
The third is employing biopsy on polar body which is released on day 0 of
fertilization. Though polar body provide only the maternal genetic information, the
study still produce meaningful data, for most aneuploidies are originated in female
meiosis(Gutierrez-Mateo, Benet et al. 2005). And the oocyte will have a reciprocal
loss or gain in chromatid if the polar body is chromosomally abnormal, as shown in
figure 3. However, a number of meiosis errors are expected to be corrected later, thus
Figure 3 The aneuploidy originated in female meiosis. Adapted from "
Reliability of comparative genomic hybridization to detect chromosome
abnormalities in first polar bodies and metaphase II oocytes" by
Gutierrez-Mateo, C., D. Wells, et al. Hum. Reprod. 19(9): 2118-2125.
Evaluation of PGD-AS methods- 11 -
the CGH on polar body may over estimate the aneuploidy rate if no confirmation is
made(Dagan Wells 2002).
Besides, if CGH is performed on blastomere cells, the inherent risk of
misdiagnose due to high level of mosaicism cannot be avoided as well(Leeanda
Wilton 2001). Also, CGH cannot detect alterations that do not involve gain or loss of
DNA and therefore is unable to differentiate between balanced gametes, which is
prone to aneuploidy from normal ones (Gutierrez-Mateo, Gadea et al. 2005).
Conclusion
In summary, each of FISH and CGH has their own feature, as shown in table 1.
Table 1
The comparison of PGD-AS by FISH and CGH
Indication
Time needed for biopsy
detecting range
requirement of fixation
most suitable material
distinguish the mechanism
FISH
1 day
5-9 chromosomes
high
blastomere
able
CGH
4-5 days*
all chromosomes
none
polar body
unable
*
maybe reduced to 30 hours by using better protocol
To combine their advantage and overcome the defects, a combination of CGH
and FISH is recommended. CGH analysis on polar body can detect almost all the
chromosome and chromatid errors with enough time for biopsy. And FISH analysis on
blastomere cells, using the probes of the chromosome which is reported abnormal by
CGH can greatly increase the pertinence of FISH remedying its limitation of detecting
range. Moreover, FISH can confirm the results of CGH, avoiding the overestimation
of CGH and distinguish the balanced gametes. Also by employing biopsy on two
Evaluation of PGD-AS methods- 12 -
different materials, the mosaicism can be alleviated to a significant extent, while not
harming the vitality of embryo.
Currently, there is few experiment practicing the combination suit of methods,
future study may identify this theoretical superiority. If expected improvement is
observed, the following clinical implement is suggested.
Evaluation of PGD-AS methods- 13 -
References
Bahce, M., T. Escudero, et al. (2000). "Improvements of preimplantation diagnosis of aneuploidy by
using microwave hybridization, cell recycling and monocolour labelling of probes." Mol. Hum.
Reprod. 6(9): 849-854.
Cohen, J. and S. Munne (2005). "Comment 2 on Staessen et al. (2004). Two-cell biopsy and PGD
pregnancy outcome." Hum. Reprod. 20(8): 2363-2364.
Committee, E. P. C. S. (2002). "ESHRE Preimplantation Genetic Diagnosis Consortium: data
collection III (May 2001)." Hum. Reprod. 17(1): 233-246.
Dagan Wells, T. E., Brynn Levy,Kurt Hirschhorn, Joy D. A. Delhanty, and Santiago Munne´ (2002).
"First clinical application of comparative genomic hybridization and polar body testing for
preimplantation genetic diagnosis of aneuploidy." FERTILITY AND STERILITY VOL. 78(NO.
3).
Diblik, J., M. Macek, Sr., et al. (2005). "Topology of Chromosomes 18 and X in Human Blastomeres
from 3- to 4-Day-old Embryos." J. Histochem. Cytochem. 53(3): 273-276.
Elias, S. (2001). "Preimplantation genetic diagnose by comparative genomic hybridization." The New
England Journal of Medicine 345(21): 1569-1571.
Gutierrez-Mateo, C., J. Benet, et al. (2005). "Karyotyping of human oocytes by cenM-FISH, a new
24-colour centromere-specific technique." Hum. Reprod. 20(12): 3395-3401.
Gutierrez-Mateo, C., J. Benet, et al. (2004). "Aneuploidy study of human oocytes first polar body
comparative genomic hybridization and metaphase II fluorescence in situ hybridization
analysis." Hum. Reprod. 19(12): 2859-2868.
Gutierrez-Mateo, C., L. Gadea, et al. (2005). "Aneuploidy 12 in a Robertsonian (13;14) carrier: Case
report." Hum. Reprod. 20(5): 1256-1260.
Gutierrez-Mateo, C., D. Wells, et al. (2004). "Reliability of comparative genomic hybridization to
detect chromosome abnormalities in first polar bodies and metaphase II oocytes." Hum.
Reprod. 19(9): 2118-2125.
Irina Solovei, A. C., Lothar Schermelleh,Francoise Jaunin, Catia Scasselati (2002). "Spatial
Preservation of Nuclear Chromatin." Experimental Cell Research 276: 10-23.
Kahraman, S., M. Bahce, et al. (2000). "Healthy births and ongoing pregnancies obtained by
preimplantation genetic diagnosis in patients with advanced maternal age and recurrent
implantation failure." Hum. Reprod. 15(9): 2003-2007.
Kokkali, G., C. Vrettou, et al. (2005). "Birth of a healthy infant following trophectoderm biopsy from
blastocysts for PGD of {beta}-thalassaemia major: Case report." Hum. Reprod. 20(7):
1855-1859.
Leeanda Wilton, R. W., John McBain, David Edgar, Lucille Voullaire (2001). "Birth of a Healthy Infant
after Preimplantation Confirmation of Euploidy by Comparative Genomic Hybridyzation."
The New England Journal of Medicine 345(21): 1539-1541.
McArthur, S. J., D. Leigh, et al. (2005). "Pregnancies and live births after trophectoderm biopsy and
preimplantation genetic testing of human blastocysts." Fertility and Sterility 84(6): 1628-1636.
McKenzie, L. J., S. A. Carson, et al. (2004). "Nuclear chromosomal localization in human
preimplantation embryos: correlation with aneuploidy and embryo morphology." Hum.
Reprod. 19(10): 2231-2237.
Munne, S., S. Chen, et al. (2005). "Preimplantation genetic diagnosis reduces pregnancy loss in women
Evaluation of PGD-AS methods- 14 -
aged 35 years and older with a history of recurrent miscarriages." Fertility and Sterility 84(2):
331-335.
Munne, S., J. Fischer, et al. (2006). "Preimplantation genetic diagnosis significantly reduces pregnancy
loss in infertile couples: a multicenter study." Fertility and Sterility 85(2): 326-332.
Munne, S., C. Magli, et al. (1999). "Positive outcome after preimplantation diagnosis of aneuploidy in
human embryos." Hum. Reprod. 14(9): 2191-2199.
Platteau, P., C. Staessen, et al. (2005). "Preimplantation genetic diagnosis for aneuploidy screening in
women older than 37 years." Fertility and Sterility 84(2): 319-324.
Santiago Munné, M. S., Tomas Escudero, Esther Velilla, Renee Walmsley, Sasha Sadowy, Jacques and
D. S. Cohen (2003). "Improved implantation after preimplantationgenetic diagnosis of
aneuploidy." Reproductive BioMedicine Online Vol 7(No 1. 91–97):
Sermon, K., C. Moutou, et al. (2005). "ESHRE PGD Consortium data collection IV: May-December
2001." Hum. Reprod. 20(1): 19-34.
Staessen, C., P. Platteau, et al. (2004). "Comparison of blastocyst transfer with or without
preimplantation genetic diagnosis for aneuploidy screening in couples with advanced maternal
age: a prospective randomized controlled trial." Hum. Reprod. 19(12): 2849-2858.
Thornhill, A. R., C. E. deDie-Smulders, et al. (2005). "ESHRE PGD Consortium 'Best practice
guidelines for clinical preimplantation genetic diagnosis (PGD) and preimplantation genetic
screening (PGS)'." Hum. Reprod. 20(1): 35-48.
Van Voorhis, B. J. (2007). "In Vitro Fertilization." N Engl J Med 356(4): 379-386.