* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Pneumonitis
Survey
Document related concepts
Transcript
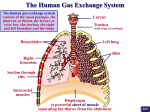
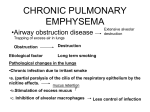
PNEUMONITIS What is it? What causes it? How do I identify and treat it? Our Lungs • The lungs take the oxygen we inhale and helps it enter the red blood cell via the alveoli. • Red blood cells then carry oxygen around the body and deliver to all cells. • When the blood returns to the lung, the CO2 is then transferred back to the alveoli and we exhale it. Alveoli are tiny air sacs located at the end of the bronchioles. They have a very thin layer of cells and an excellent blood supply. Pneumonitis-Pathophysiology A. Inflammation of the lung- in particular the alveoli B. The thin layers of cells in alveolus are 97% Type 1 pneumocytes and 3% type 2 pneumocytes. The beginning stages of the injury start with the death of Type 1 pneumocytes which makes the alveolar wall vulnerable. This allows protein-rich exudates to leak into the alveolar space. Hyaline membranes (fibrous membrane) then form and cover the empty and damaged alveolar wall. This temporarily walls the alveolus off from the rest of the body and inhibits oxygen and CO2 delivery. After approximately 7 days, a period of organization occurs and fibroblastic tissue fills the alveolar space and the intersitium. Alveoli eventually recover or progress to permanent fibrosis. Drugs may contribute to this pattern of toxicity by causing apoptosis of epithelial cells and/ or by inhibiting recovery during the organizing phase. Some drugs cause an affect in the immune pathway- the insult activates the coagulation pathway leading to the conversion of fibrinogen into fibrin plugs. Fibrin is then laid down in the alveoli and eventually becomes a mass mixed consisting of fibrin and histocytes. Causative Agents Chemotherapy Non-chemotherapy • All chemotherapies have the potential to cause pneumonitis, although some have a higher incidence. 1. Bleomycin 2. Busulfan 3. Carmustine 4. Cyclophosphamide 5. Taxanes – Paclitaxel, Docetaxel 6. Methotrexate 1. Radiation- either in thoracic guided treatments (e.g-lung, breast) or whole body rads in preparation for transplant. • Anti-tumor necrosis factor monoclonal antibodies 1. Cetuximab (Erbitux) 2. Bevacizumab (Avastin) 3. Trastuzumab (Herceptin) • PD-1 and PDL-1 1. Nivolumab 2. Pembrolizumab 3. Ipilumumab Symptoms DYSPNEA DRY COUGH FATIGUE MAY PRESENT WITH: LOW GRADE FEVER ANOREXIA Identifying Differential Diagnostics • Can be TRICKY!!!!! • Awareness of treatment modalities and drugs • Overall is a diagnosis of exclusion • Lab draws are overall not helpful with drug induced pneumonitis • X-Rays • CT • Bronchoscopy with lavage • Lung Biopsy Treatment 1. REMOVE the offending agent 1. Corticosteroids- mostly prednisone 2. At times mycophenalate Mofetil (MMF) will be used together with prednisone REMEMBER – EARLIER TREATMENT = BETTER OUTCOMES AND…. WHAT HAPPENS NEXT • Depending on the severity of the reaction - If patient was still on active treatment it is not uncommon to re-challenge them once symptoms have resolved and they have been weaned off steroids. Many patients with a minor reaction (grade 1-2) will go on to finish treatment without ever having another episode. • If they had a more severe reaction (grade3/4) the drug is permanently discontinued and should be placed on an allergy list. • Recurrence rates are not well documented, known or understood. Complications • If not recognized and left untreated pneumonitis can lead to pulmonary fibrosis- which can then lead to right heart failure, respiratory failure and death. • Pulmonary edema • Pulmonary hypertension • Hemorrhage and hemoptysis Questions???