* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download 6 ACE inhibitors and angio- tensin receptor blockers
Survey
Document related concepts
Transcript
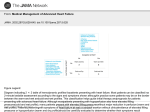
6 ACE inhibitors and angiotensin receptor blockers What will I learn? Inthissectionyouwilllearn: • WhatACEinhibitorsandARBsdo • Howtheyimprovesymptomsandoutcomesinpeoplewithheart failure • Howtostartandtitratethedose • Whatthepossiblesideeffectsareandwhattodoaboutthem Angiotensin converting enzyme inhibitors are the current first-line therapy for heart failure, as recommended by the ESC, due to the fact that they reduce mortality by up to 26%. They act on the part of the renin−angiotensin– aldosterone system (RAAS), which normally converts angiotensin I into angiotensin II. How do ACE inhibitors modify the activity of the RAAS? If you remember how the RAAS works, you will recall that it is the angiotensin converting enzyme (ACE) which turns the fairly inactive angiotensin I into the potent vasoconstrictor, angiotensin II. If angiotensin I cannot be converted into angiotensin II then all the effects associated with angiotensin II will be affected. For example, sodium and water retention, which are responsible for many of the congestive symptoms of heart failure, will be reduced. Therefore, to stop ACE from working, we need an ACE inhibitor (Fig. 1). Which ACE inhibitors are available? A number of different ACE inhibitors are available (Table 1). How do we use them? ACE inhibitors should be started at a low dose and increased slowly. Dose ACE inhibitors and angiotensin receptor blockers 9780620421645.indb 27 16/9/08 11:09:52 titration is important with ACE inhibitors as it ensures that patients are able to tolerate them well (‘start low, go slow but go up’). You will then have time to check with the patient for any possible side effects and also keep an eye on his biochemical status. The aim is to gradually get patients onto the optimum dose – this is the one that was used in clinical trials (or which is advised by the manufacturers if large studies have not been undertaken with the drug in question). Figure 1. Areas where drug treatment can modify the activity of the RAAS. Angiotensinogen Renin inhibition 1 Renin Angiotensin I ACE inhibitor ACE 2 Angiotensin II Angiotensin II blocker (ARB) X 3 Vasoconstriction Blood pressure End-organ damage 28 9780620421645.indb 28 Pocket Guide to Chronic Heart Failure 16/9/08 11:09:53 Table 1. ACE inhibitors often used in heart failure (all doses are once daily unless otherwise stated). Name Starting dose Target dose Ramipril 2.5 mg bd 5 mg bd Perindopril 2 mg 4 mg Lisinopril 2.5−5 mg 10−20 mg Enalapril 2.5−5 mg bd 10−20 mg bd Captopril 6.25−12.5 mg tid 50 mg tid Quinapril 2.5−5 mg 10−20 mg bd Trandolapril 1 mg 4 mg P reviously we met George, who had symptoms of heart failure. Following careful investigation, he was diagnosed with left ventricular systolic dysfunction with an ejection fraction of 32%. He is breathless when he exercises and tries to limit his activities because of this. He is currently taking ramipril 2.5 mg, which was prescribed following his diagnosis and after getting a baseline assessment of urea and electrolytes a month ago. What would you do now? George’s management plan The initial dose of 2.5 mg should be continued for at least 2 weeks After ten days or so on the drug, blood tests should be repeated to reassess the urea and electrolytes. If all is well, the dose may be increased to 5 mg, which can be described as being half the ‘normal’ dose. After a further two to four weeks, the dose will finally be increased to the full, evidence-based dose of 10 mg. Urea and electrolytes can then be assessed once the full dose has been reached and every six months or so thereafter, depending on George’s general condition. This is a useful approach as patients can become anxious at the thought that the dose of their treatment is being doubled and doubled again. This ‘quarter dose – half dose – full dose’ approach may improve compliance. ACE inhibitors and angiotensin receptor blockers 9780620421645.indb 29 29 16/9/08 11:09:54 What side effects should I look out for? Most people tolerate ACE inhibitors well and side effects occur in only a minority of people. However, it is important to monitor urea and electrolyte levels because of the way in which ACE inhibitors work on the RAAS. The most common side effect is cough. This is caused by the effect of ACE inhibitors on bradykinin levels. If an irritating cough occurs for which no other cause can be found, then the ACE inhibitor should be substituted with an ARB. Examples of ARBs that are licensed for heart failure treatment include candesartan and valsartan. Where do angiotensin receptor blockers fit in? Angiotensin receptor blockers work in a similar way to ACE inhibitors but at a different level in the RAAS (see Fig. 1 above). Unlike ACE inhibitors, they do not stop angiotensin II from developing but they do stop it from acting. ARBs have fewer side effects than ACE inhibitors, and in particular do not cause cough. Currently, candesartan and valsartan are ARBs licensed for use in heart failure but valsartan is only licensed for post-myocardial heart failure. Nonetheless it is common to see all the ARBs used. The European Society of Cardiology guidelines comment as follows on angiotensin II receptor blocker usage. For patients with left ventricular systolic dysfunction: • ARBs can be used as an alternative to ACE inhibition in symptomatic patients intolerant of ACE inhibitors to improve morbidity and mortality (class or recommendation I, level of evidence B). • ARBs and ACE inhibitors seem to have similar efficacy on mortality and morbidity in chronic heart failure (class of recommendation IIa, level of evidence B). • In acute myocardial infarction with signs of heart failure or left ventricular dysfunction, ARBs and ACE inhbitors have similar or equivalent effects on mortality (class of recommendation I, level of evidence A). • ARBs can be considered in combination with ACE inhibitors in patients who remain symptomatic, to reduce mortality (class of recommendation IIa, level of evidence B) and hospital admissions for heart failure (class recommendation I, level of evidence A). 30 9780620421645.indb 30 Pocket Guide to Chronic Heart Failure 16/9/08 11:09:54 For more information on drug treatments see www.besttreatments.co.uk For more detailed information on prescribing issues go to www.prescriber.org.uk For full details on licensed ACE inhibitors and ARBs access the British National Formulary on-line at www.bnf.org For an on-line tutorial and quiz on the action of ACE inhibitors on the RAAS, go to http://faculty.alverno.edu/bowneps/raa/raaproblem1.htm What you need to know ACE inhibitors ‘down regulate’ the activity of the RAAS and thus prevent fluid and salt retention. By doing this they improve symptoms of breathlessness and oedema, which are associated with heart failure, and mortality can be reduced by 25%. c ACE inhibitors should be started at a low dose and titrated up to the maximum tolerated dose where possible. c Cough is the commonest side effect of ACE inhibitors; if the cough is considered to be due to the ACE inhibitor, an ARB should be used instead. c Creatinine, urea and electrolyte levels should also be monitored. c Self-assessment questions Take a minute to test your knowledge: 1. Name three types of ACE inhibitor. 2. Describe which part of the RAAS is affected by ACE inhibitors. 3. What action would you take if George developed a dry, irritating cough after starting on ramipril? ACE inhibitors and angiotensin receptor blockers 9780620421645.indb 31 31 16/9/08 11:09:55