* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Blood Pressure
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Myocardial infarction wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
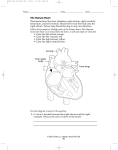
42 Circulation © 2014 Pearson Education, Inc. Concept 42.1: Circulatory systems link exchange surfaces with cells throughout the body In small or thin animals, cells can exchange materials directly with the surrounding medium by diffusion but diffusion is only efficient over small distances. In most animals, cells exchange materials with the environment via a fluid-filled circulatory system A circulatory system has A circulatory fluid A set of interconnecting vessels A muscular pump, the heart © 2014 Pearson Education, Inc. Open and Closed Circulatory Systems The circulatory system connects the fluid that surrounds cells with the organs that exchange gases, absorb nutrients, and dispose of wastes Circulatory systems can be open or closed and vary in the number of circuits in the body In insects, other arthropods, and some molluscs, circulatory fluid called hemolymph bathes the organs directly in an open circulatory system In a closed circulatory system, blood is confined to vessels and is distinct from the interstitial fluid. Annelids, cephalopods, and vertebrates have closed circulatory systems © 2014 Pearson Education, Inc. Figure 42.3 (a) An open circulatory system (b) A closed circulatory system Heart Heart Interstitial fluid Blood Hemolymph in sinuses Small branch vessels in each organ Pores Dorsal vessel (main heart) Tubular heart © 2014 Pearson Education, Inc. Auxiliary hearts Ventral vessels Organization of Vertebrate Circulatory Systems Humans and other vertebrates have a closed circulatory system called the cardiovascular system The three main types of blood vessels are arteries, veins, and capillaries. Blood flow is one way in these vessels Arteries and veins are distinguished by the direction of blood flow, not by O2 content Arteries branch into arterioles and carry blood away from the heart to capillaries Networks of capillaries called capillary beds are the sites of chemical exchange between the blood and interstitial fluid Venules converge into veins and return blood from capillaries to the heart © 2014 Pearson Education, Inc. Figure 42.4a Bony fishes, rays, and sharks have single circulation with a two-chambered heart In single circulation, blood leaving the heart passes through two capillary beds before returning (a) Single circulation: fish Gill capillaries Artery Heart: Atrium (A) Ventricle (V) Vein Body capillaries Key © 2014 Pearson Education, Inc. Oxygen-rich blood Oxygen-poor blood Double Circulation Amphibians, reptiles, and mammals have double circulation Oxygen-poor and oxygen-rich blood are pumped separately from the right and left sides of the heart In reptiles and mammals, oxygen-poor blood flows through the pulmonary circuit to pick up oxygen through the lungs In amphibians, oxygen-poor blood flows through a pulmocutaneous circuit to pick up oxygen through the lungs and skin Oxygen-rich blood delivers oxygen through the systemic circuit Double circulation maintains higher blood pressure in the organs than does single circulation © 2014 Pearson Education, Inc. Frogs and other amphibians have a three-chambered heart: two atria and one ventricle The ventricle pumps blood into a forked artery that splits the ventricle’s output into the pulmocutaneous circuit and the systemic circuit When underwater, blood flow to the lungs is nearly shut off Turtles, snakes, and lizards have a three-chambered heart: two atria and one ventricle, partially divided by an incomplete septum In alligators, caimans, and other crocodilians a septum divides the ventricles but pulmonary and systemic circuits connect where arteries exit the heart © 2014 Pearson Education, Inc. Figure 42.4b (b) Double circulation: amphibian Pulmocutaneous circuit Lung and skin capillaries Atrium (A) Atrium (A) Right Left Ventricle (V) Systemic capillaries Key © 2014 Pearson Education, Inc. Systemic circuit Oxygen-rich blood Oxygen-poor blood Mammals and birds have a four-chambered heart with two atria and two ventricles The left side of the heart pumps and receives only oxygen-rich blood, while the right side receives and pumps only oxygen-poor blood Mammals and birds are endotherms and require more O2 than ectotherms © 2014 Pearson Education, Inc. Figure 42.4c (c) Double circulation: mammal Pulmonary circuit Lung capillaries A A V V Right Left Systemic capillaries Systemic circuit Key © 2014 Pearson Education, Inc. Oxygen-rich blood Oxygen-poor blood Coordinated cycles of heart contraction drive double circulation in mammals Blood begins its flow with the right ventricle pumping blood to the lungs via the pulmonary arteries In the lungs, the blood loads O2 and unloads CO2 Oxygen-rich blood from the lungs enters the heart at the left atrium via the pulmonary veins It is pumped through the aorta to the body tissues by the left ventricle The aorta provides blood to the heart through the coronary arteries Blood returns to the heart through the superior vena cava (blood from head, neck, and forelimbs) and inferior vena cava (blood from trunk and hind limbs) The superior vena cava and inferior vena cava flow into the right atrium © 2014 Pearson Education, Inc. Figure 42.5 Superior vena cava Capillaries of head and forelimbs 7 Pulmonary artery Capillaries of right lung Pulmonary artery Aorta 9 Capillaries of left lung 6 2 3 3 4 11 Pulmonary vein Right atrium Right ventricle 1 Pulmonary vein Left atrium Left ventricle 5 10 Aorta Inferior vena cava 8 © 2014 Pearson Education, Inc. Capillaries of abdominal organs and hind limbs The Mammalian Heart: A Closer Look A closer look at the mammalian heart provides a better understanding of double circulation The two atria have relatively thin walls and serve as collection chambers for blood returning to the heart The ventricles have thicker walls and contract much more forcefully © 2014 Pearson Education, Inc. Figure 42.6 Aorta Pulmonary artery Pulmonary artery Right atrium Left atrium Semilunar valve Semilunar valve Atrioventricular (AV) valve Atrioventricular (AV) valve Right ventricle © 2014 Pearson Education, Inc. Left ventricle The heart contracts and relaxes in a rhythmic cycle called the cardiac cycle The contraction, or pumping, phase is called systole The relaxation, or filling, phase is called diastole © 2014 Pearson Education, Inc. Figure 42.7-3 2 Atrial systole and ventricular diastole 1 Atrial and ventricular diastole 0.1 sec 0.4 sec 0.3 sec 3 Ventricular systole and atrial diastole © 2014 Pearson Education, Inc. The heart rate, also called the pulse, is the number of beats per minute The stroke volume is the amount of blood pumped in a single contraction The cardiac output is the volume of blood pumped into the systemic circulation per minute and depends on both the heart rate and stroke volume © 2014 Pearson Education, Inc. Four valves prevent backflow of blood in the heart The atrioventricular (AV) valves separate each atrium and ventricle The semilunar valves control blood flow to the aorta and the pulmonary artery The “lub-dup” sound of a heart beat is caused by the recoil of blood against the AV valves (lub) then against the semilunar (dup) valves Backflow of blood through a defective valve causes a heart murmur © 2014 Pearson Education, Inc. Maintaining the Heart’s Rhythmic Beat Some cardiac muscle cells are autorhythmic, meaning they contract without any signal from the nervous system The sinoatrial (SA) node, or pacemaker, sets the rate and timing at which cardiac muscle cells contract Impulses that travel during the cardiac cycle can be recorded as an electrocardiogram (ECG or EKG) © 2014 Pearson Education, Inc. Figure 42.8-4 1 Signals (yellow) from SA node spread through atria. SA node (pacemaker) ECG © 2014 Pearson Education, Inc. 2 Signals are delayed at AV node. AV node 3 Bundle branches pass signals to heart apex. Bundle branches Heart apex 4 Signals spread throughout ventricles. Purkinje fibers Impulses from the SA node travel to the atrioventricular (AV) node At the AV node, the impulses are delayed and then travel to the Purkinje fibers that make the ventricles contract The pacemaker is regulated by two portions of the nervous system: the sympathetic and parasympathetic divisions The sympathetic division speeds up the pacemaker The parasympathetic division slows down the pacemaker The pacemaker is also regulated by hormones and temperature © 2014 Pearson Education, Inc. Blood Vessel Structure and Function A vessel’s cavity is called the central lumen The epithelial layer that lines blood vessels is called the endothelium The endothelium is smooth and minimizes resistance Capillaries are only slightly wider than a red blood cell Capillaries have thin walls, the endothelium plus its basal lamina, to facilitate the exchange of materials Arteries and veins have an endothelium, smooth muscle, and connective tissue Arteries have thicker walls than veins to accommodate the high pressure of blood pumped from the heart In the thinner-walled veins, blood flows back to the heart mainly as a result of muscle action © 2014 Pearson Education, Inc. Figure 42.9a Valve Basal lamina Endothelium Smooth muscle Connective Capillary tissue Endothelium Smooth muscle Connective tissue Artery Vein Arteriole © 2014 Pearson Education, Inc. Venule Figure 42.9b Vein LM Artery Capillary © 2014 Pearson Education, Inc. LM Red blood cell 15 µm Red blood cells 100 µm Figure 42.10 © 2014 Pearson Education, Inc. Systolic pressure Venae cavae Veins Venules Capillaries Diastolic pressure Arterioles 120 100 80 60 40 20 0 Arteries 50 40 30 20 10 0 Aorta Velocity (cm/sec) Blood flow in capillaries is necessarily slow for exchange of materials 5,000 4,000 3,000 2,000 1,000 0 Pressure (mm Hg) Velocity of blood flow is slowest in the capillary beds, as a result of the high resistance and large total crosssectional area Area (cm2) Blood Flow Velocity Blood Pressure Blood pressure is the pressure that blood exerts in all directions, including against the walls of blood vessels. Blood flows from areas of higher pressure to areas of lower pressure The recoil of elastic arterial walls plays a role in maintaining blood pressure The resistance to blood flow in the narrow diameters of tiny capillaries and arterioles dissipates much of the pressure Systolic pressure is the pressure in the arteries during ventricular systole; it is the highest pressure in the arteries Diastolic pressure is the pressure in the arteries during diastole; it is lower than systolic pressure A pulse is the rhythmic bulging of artery walls with each heartbeat © 2014 Pearson Education, Inc. Regulation of Blood Pressure Homeostatic mechanisms regulate arterial blood pressure by altering the diameter of arterioles Vasoconstriction is the contraction of smooth muscle in arteriole walls; it increases blood pressure Vasodilation is the relaxation of smooth muscles in the arterioles; it causes blood pressure to fall Nitric oxide is a major inducer of vasodilation The peptide endothelin is a strong inducer of vasoconstriction Vasoconstriction and vasodilation are often coupled to changes in cardiac output that affect blood pressure Fainting is caused by inadequate blood flow to the head © 2014 Pearson Education, Inc. Figure 42.11 Blood pressure is generally measured for an artery in the arm at the same height as the heart Pressure in cuff greater than 120 mm Hg Cuff inflated with air Pressure in cuff drops below 120 mm Hg 120 Pressure in cuff below 70 mm Hg 120 70 Artery closed 1 2 Sounds audible in stethoscope Sounds stop 3 Blood pressure for a healthy 20-year-old human at rest is about 120 mm Hg at systole and 70 mm Hg at diastole © 2014 Pearson Education, Inc. Figure 42.12 Blood is moved through veins by smooth muscle contraction, skeletal muscle contraction, and expansion of the vena cava with inhalation One-way valves in veins prevent backflow of blood © 2014 Pearson Education, Inc. Direction of blood flow in vein (toward heart) Valve (open) Skeletal muscle Valve (closed) Capillary Function Blood flows through only 5–10% of the body’s capillaries at any given time. While capillaries in major organs are usually filled to capacity, blood supply varies in many other sites Two mechanisms regulate distribution of blood in capillary beds Constriction or dilation of arterioles that supply capillary beds Precapillary sphincters that control flow of blood between arterioles and venules Blood flow is regulated by nerve impulses, hormones, and other chemicals © 2014 Pearson Education, Inc. Figure 42.13 Precapillary sphincters Arteriole Thoroughfare channel Capillaries Venule (a) Sphincters relaxed Arteriole (b) Sphincters contracted © 2014 Pearson Education, Inc. Venule The exchange of substances between the blood and interstitial fluid takes place across the thin endothelial walls of the capillaries The difference between blood pressure and osmotic pressure drives fluids out of capillaries at the arteriole end and into capillaries at the venule end Most blood proteins and all blood cells are too large to pass through the endothelium © 2014 Pearson Education, Inc. Figure 42.14 INTERSTITIAL FLUID Net fluid movement out Body cell Blood pressure Osmotic pressure Arterial end of capillary © 2014 Pearson Education, Inc. Direction of blood flow Venous end of capillary Fluid Return by the Lymphatic System The lymphatic system returns fluid that leaks out from the capillary beds Fluid lost by capillaries is called lymph The lymphatic system drains into veins in the neck Valves in lymph vessels prevent the backflow of fluid Edema is swelling caused by disruptions in the flow of lymph Lymph nodes are organs that filter lymph and play an important role in the body’s defense When the body is fighting an infection, lymph nodes become swollen and tender © 2014 Pearson Education, Inc. Concept 42.4: Blood components function in exchange, transport, and defense The closed circulatory systems of vertebrates contain a more highly specialized fluid called blood Blood in vertebrates is a connective tissue consisting of several kinds of cells suspended in a liquid matrix called plasma The cellular elements occupy about 45% of the volume of blood Suspended in blood plasma are two types of cells Red blood cells (erythrocytes) transport O2 White blood cells (leukocytes) function in defense Platelets are fragments of cells that are involved in clotting © 2014 Pearson Education, Inc. Figure 42.16 Plasma 55% Constituent Major functions Water Solvent Ions (blood electrolytes) Sodium Potassium Calcium Magnesium Chloride Bicarbonate Osmotic balance, pH buffering, and regulation of membrane permeability Plasma proteins Albumin Cellular elements 45% Separated blood elements Osmotic balance, pH buffering Fibrinogen Clotting Functions Defense and immunity Lymphocytes Eosinophils Immunoglobulins Defense (antibodies) Lipid transport 5,000–10,000 Leukocytes (white blood cells) Basophils Apolipoproteins Number per µL (mm3) of blood Cell type Neutrophils Platelets Monocytes 250,000–400,000 Blood clotting Substances transported by blood Nutrients (such as glucose, fatty acids, vitamins) Waste products of metabolism Respiratory gases (O2 and CO2) Hormones © 2014 Pearson Education, Inc. Erythrocytes (red blood cells) 5,000,000–6,000,000 Transport of O2 and some CO2 Plasma Plasma contains inorganic salts as dissolved ions, sometimes called electrolytes Plasma proteins influence blood pH and help maintain osmotic balance between blood and interstitial fluid Particular plasma proteins function in lipid transport, immunity, and blood clotting Plasma is similar in composition to interstitial fluid, but plasma has a much higher protein concentration © 2014 Pearson Education, Inc. Erythrocytes Red blood cells, or erythrocytes, are the most numerous blood cells They contain hemoglobin, the iron-containing protein that transports O2 Each molecule of hemoglobin binds up to four molecules of O2 In mammals, mature erythrocytes lack nuclei and mitochondria © 2014 Pearson Education, Inc. Leukocytes There are five major types of white blood cells, or leukocytes: monocytes, neutrophils, basophils, eosinophils, and lymphocytes They function in defense either by phagocytizing bacteria and debris or by mounting immune responses against foreign substances They are found both in and outside of the circulatory system © 2014 Pearson Education, Inc. Stem Cells and the Replacement of Cellular Elements Erythrocytes, leukocytes, and platelets all develop from a common source of stem cells in the red marrow of bones, especially ribs, vertebrae, sternum, and pelvis The hormone erythropoietin (EPO) stimulates erythrocyte production when O2 delivery is low Physicians can use recombinant EPO to treat people with conditions such as anemia © 2014 Pearson Education, Inc. Figure 42.17 Stem cells (in bone marrow) Myeloid stem cells Lymphoid stem cells B cells T cells Erythrocytes Neutrophils Basophils Lymphocytes Monocytes Platelets © 2014 Pearson Education, Inc. Eosinophils Blood Clotting Coagulation is the formation of a solid clot from liquid blood A cascade of complex reactions converts inactive fibrinogen to fibrin, forming a clot A blood clot formed within a blood vessel is called a thrombus and can block blood flow Red blood cells caught in threads of fibrin © 2014 Pearson Education, Inc. 5 µm Figure 42.18a 1 2 3 Platelet plug Collagen fibers Platelet Clotting factors from: Platelets Damaged cells Plasma (factors include calcium, vitamin K) Enzymatic cascade Prothrombin Thrombin Fibrinogen © 2014 Pearson Education, Inc. Fibrin Fibrin clot Fibrin clot formation Cardiovascular Disease Cardiovascular diseases are disorders of the heart and the blood vessels These diseases range in seriousness from minor disturbances of vein or heart function to life-threatening disruptions of blood flow to the heart or brain One type of cardiovascular disease, atherosclerosis, is caused by the buildup of Endothelium fatty deposits (plaque) within arteries Lumen Cholesterol is a key player Thrombus in the development of Plaque atherosclerosis Inflammation plays a role in atherosclerosis and thrombus formation © 2014 Pearson Education, Inc. Coronary circulation © 2014 Pearson Education, Inc. A heart attack, or myocardial infarction, is the damage or death of cardiac muscle tissue resulting from blockage of one or more coronary arteries A stroke is the death of nervous tissue in the brain, usually resulting from rupture or blockage of arteries in the head Aspirin inhibits inflammation and reduces the risk of heart attacks and stroke Angina pectoris is chest pain caused by partial blockage of the coronary arteries Hypertension, or high blood pressure, also contributes to heart attack and stroke, as well as other health problems. Hypertension can be controlled by dietary changes, exercise, and/or medication © 2014 Pearson Education, Inc. © 2014 Pearson Education, Inc.