* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Replaced Common Hepatic Artery From Superior Mesenteric Artery
Survey
Document related concepts
Transcript
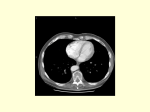
Replaced Common Hepatic Artery From Superior Mesenteric Artery During Pancreaticoduodenectomy M. Wood, C. Lazo, V. Hassid, Z.T. Awad Department of Surgery, University of Florida College of Medicine, Jacksonville, USA Abstract dissected and preserved as it passed dorsal to the pancreas. Preservation of the blood supply to the liver and biliary tree is important after PD to prevent biliary fistula and hepatic ischaemia. The hepatic arterial anatomy is highly variable. A 67 year female with pancreatic mass and replaced common hepatic artery originating from the superior mesenteric artery underwent pancreaticoduodenectomy (PD). The anomalous vessel was discovered on preoperative CT scan and MRI. The vessel was Keywords Replaced common hepatic Pancreaticoduodenectomy, Whipple Introduction artery, that time that the CHA originated from the SMA (Fig. 1). CT pancreas protocol confirmed the MRI finding. The patient underwent an exploratory laparotomy and PD. Intra-operatively, the CHA was identified to the left of the common bile duct, and it was carefully dissected downstream where it gave origin to the gastroduodenal artery (GDA) at the upper border of the gland before coursing dorsal to the neck of the pancreas. The common bile duct was divided, and its distal end was retracted caudally to expose the portal vein. The pancreatic neck tunnel was created and the pancreas was transected exposing the RCHA which was anterior to the portal vein – superior mesenteric vein (SMV) confluence before it courses behind the SMV to its origin from the SMA (Fig. 2). The patient postoperative course was unremarkable and was discharged home on 12. Pathology was consistent with chronic pancreatitis. The hepatic arterial anatomy is anomalous in nearly 50% of all individuals(1). The most common anomalies include the right hepatic artery arising from the superior mesenteric artery and the left hepatic artery arising from the left gastric artery. The incidence of the replaced common hepatic artery (RCHA) originating from the superior mesenteric artery (SMA) has been estimated to be 1.5% - 4.0%(2). Pancreatoduodenectomy (PD) is the standard operative procedure for periampullary cancer and other pancreatic diseases. When planning for PD, knowledge of the hepatic arterial blood supply is essential to avoid unnecessary surgical complications, and this can best be achieved by preoperative imaging evaluation of the vasculature. Case Report A 67 year-old woman presented with few weeks history of epigastric pain and weight loss. EGD showed duodenal stenosis, MRI of the abdomen revealed a three-centimeter discrete pancreatic mass. Also, it was noted at Discussion Understanding the variant patterns in anatomy around the porta hepatis can aid in preventing injury to ducts and blood vessels during surgery. The importance of sparing the CHA during PD lies in preventing possible hepatic ischemia as well as in preventing breakdown of biliaryenteric anastomosis(3). Correspondence: Ziad T. Awad, M.D, FRCSI, FACS, Assistant Professor of Surgery, Director of Minimally Invasive Surgery, University of Florida College of Medicine Jacksonville, 653 West 8th Street, 3rd Floor Faculty Clinic, Jacksonville, FL 32209, USA, Phone: 001 904 244 3971 Fax: 001 904 244 3870, Email: [email protected] 60 Historically, visceral angiography was used for preoperative evaluation of patients with pancreatic neoplasrns, and was felt to provide G. J. O. Issue 11, 2012 useful information in regard to tumor staging (extension to portal vein and SMA) as well as the presence of anomalous hepatic arterial vessels(4). Among the multiple modalities that exist, there is no single gold standard staging approach adopted by all. However, multidetector CT allows comprehensive preoperative assessment of pancreatic adenocarcinoma. Carefully timed scan acquisition maximizes the difference in attenuation between the neoplasm and the pancreatic parenchyma and allows accurate local and distant staging as well as assessment of local resectability. In addition, angiographic data sets can be rendered to create displays of the local venous and arterial anatomy that are familiar to surgeons(5-6). If a RCHA is known preoperatively, one should delay ligation of the GDA until the retropancreatic dissection (through the posterior approach) and proper identification of the RCHA is completed. This is followed by division of the pancreatic neck over the RCHA and proximal SMA rather than the superior mesenteric veinportal vein confluence. Yamamoto et al. have described five different methods for dealing with a RCHA, which can also be applied to a replaced right hepatic artery (RRHA)(7). A RCHA that courses through the pancreatic parenchyma can be preserved by dividing the pancreas. With this strategy, there is a risk of not achieving tumorfree margins because the division line of the pancreas is likely to be lateral or to the right of the standard pancreatic division line. Often, a RCHA or RRHA that courses ventral to the pancreas can be displaced and dissected from the surface of the pancreatic parenchyma and a standard PD can be performed. When a RCHA is known to have an anastomotic connection to the LGA or another accessory artery, ligation resulted in no compromise to the arterial blood supply of the liver or extrahepatic biliary tree. A fourth approach involves division of the RCHA or RRHA and reconstruction using an autologous vascular graft such as the GDA or saphenous vein. We advocate direct anastomosis to the aorta with construction and caution that anastomosis to the SMA should be avoided due to technical difficulties and the risk of mesenteric ischemia. Finally, the surgeon should remember 61 that a pylorus-preserving PD, which preserves the right gastric artery can often be performed with subsequent division of the RCHA if collateral communication to the RCHA has been demonstrated preoperatively. Surgeons should have knowledge of the anatomical vasculature variations when planning PD. Preoperative imaging studies can aid and should be performed in anticipation of the potential vascular variations during PD. Fig. 1 : CT pancreas protocol reconstruction of the CHA originating from the SMA. Fig. 2 : Intra-operative photograph of the CHA dissected from its origin at the SMA. Replaced Common Hepatic Artery, M. Wood, et. al. References 1.Michels NA. Newer anatomy of the liver and its variant blood supply and collateral circulation. Am J Surg. 1966; 112:337-347. 5.Horiguchi A, Ishihara S, Ito M, Nagata H, Asano Y, Yamamoto T, Kato R, Katada K, Miyakawa S. Multislice CT study of pancreatic head arterial dominance. J Hepatobiliary Pancreat Surg. 2008;15(3):322-6 2.Yang SH, Yin YH, Jang JY et al. Assessment of hepatic arterial anatomy in keeping with preservation of the vasculature while performing pancreatoduodenectomy: an opinion. World J Surg. 2007; 12:2384-2391. 6.Brennan DD, Zamboni GA, Raptopoulos VD, Kruskal JB. Comprehensive preoperative assessment of pancreatic adenocarcinoma with 64-section volumetric CT. Radiographics. 2007 NovDec;27(6):1653-66. 3.Woods MS, Traverso LW. Sparing a replaced common hepatic artery during pancreaticoduodenectomy. Am Surg. 1993; 59:719–721. 7.Yamamoto S, Kubota K, Rokkaku K, et al. Disposal of replaced common hepatic artery coursing within the pancreas during pancreatoduodenectomy: report of a case. Surg Today 2005;35:984-7. 4.Volpe CM, Peterson S, Hoover FL, et al. Justification for visceral angiography prior to pancreaticoduodenectomy. Am Surg 1998;64:758-61. 62