* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Pancreas Part 1
Survey
Document related concepts
Transcript
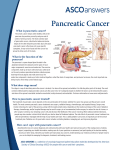
Holdorf ULTRASOUND OF THE ABDOMEN PART 1 LECTURE 4 PANCREAS PART 1 PANCREAS Outline Normal anatomy Spatial relationships of pancreatic anatomy Acute pancreatitis Chronic Pancreatitis Pancreatic cysts Cystic fibrosis Pancreatic Pseudocysts Pancreas divisum Annular pancreas pancreatic adenocarcinoma Serous cystadenoma Mucinous cystic neoplasms Islet Cell Tumors (Endocrine Tumors) Multiple Endocrine Neoplasia (MEN) Laboratory Values Summary of Anatomical spatial relationships Normal Anatomy The pancrease is a nonencapsulated, retroperitoneal structure that lies between the duodenal loop and the splenic hilum. The pancreas is divided into the head, uncinate process, neck, body, and tail. The EXOCRINE function of the pancreas is to secrete trypsin, lipase and amylase through the ductal system. Netter diagram of the Pancreas Endocrine vs. Exocrine Exocrine glands have ducts to carry their secretions to specific locations. In the pancreas, the pancreatic duct carries pancreatic fluid to the duodenum. Endocrine glands are glands of internal secretion, whose secretions are usually spread directly into the blood. Most hormones are secreted in this manner. The endocrine function (non-ductal) of the pancreas is to secrete insulin via the islets of Langerhans. On Cross-sectional images, the normal pancreas should measure < 3 cm. The posterior wall of the stomach overlies the anterior border of the pancreatic body and tail. To better visualize the pancreas (specifically the pancreatic tail), a technique is used in which the patient in left lateral decubitus position, drinks water to fill the stomach. While scanning the pancreas, the patient is then turned to the supine or right lateral decubitus position. Water in the stomach and duodenum is used as an acoustic window. Spatial Relationships of Pancreatic Anatomy Head of the pancreas is anterior to the IVC. Head of the pancreas is medial to the duodenum. CBD is posterior / lateral to the pancreatic head. Gastroduodenal artery is anterior / lateral to the pancreatic head. Spatial Relationships of the pancreatic anatomy GDA-CBD Spatial Relationships of Pancreatic Anatomy SMV-SMA-IVC Cartoon-GDA, CBD Pancreas - longitudinal Blood supply to the pancreas Spatial Relationships Aorta Cartoon- Celiac Axis Superior mesenteric artery and vein are posterior to the neck of the pancreas. Superior mesenteric artery and vein are anterior to the uncinate process. Aorta is posterior to the body of the pancreas. Celiac axis arises from the aorta at the superior border of the pancreas Superior mesenteric artery arises from the aorta at the inferior border of the pancreas. The celiac axis gives off the left gastric artery and then divides into the common hepatic artery and the splenic artery. The splenic artery follows a tortuous course along the superior border of the body and tail of the pancreas. The common hepatic artery divides into the proper hepatic and the Gastroduodenal arteries. The proper hepatic artery travels superiorly toward the liver anterior to the portal vein and left of the bile duct. The right gastric artery is a branch of proper hepatic artery. The gastroduodenal artery (GDA) travels posterior to the first portion of the duodenum than anterior to the head of the pancreas. The GDA then divides into the: Right gastroepiploic artery Superior pancreaticoduodenal artery The superior mesenteric artery is located: Inferior to the pancreas Anterior to the uncinate process Anterior to the 3rd portion of the duodenum The splenic vein is located on the posterior aspect of the pancreas. The splenic vein joins the superior mesenteric vein to create the main portal vein. The superior mesenteric vein is located: To the right of the superior mesenteric artery Anterior to the 3rd portion of the duodenum Anterior to the uncinate process. Spatial relationships GDA Spatial Relationships-Splenic vein Cartoon-Main portal vein The Common bile duct travels posterior to the 1st portion of the duodenum and the head of the pancreas to lie to the right of the main pancreatic duct. The common bile duct and the duct of Wirsung (main pancreatic duct) join to become the hepaticpancreatic ampulla (ampulla of Vater) which opens into the 2nd portion of the duodenum at the major papilla. The accessory pancreatic duct (duct of Santorini) opens into the 2nd portion of the duodenum at the minor papilla. 50% of the population has complete regression of the duct of Santorini. Spatial relationships Spatial Relationships Duct of Wirsung Duct of Santorini Duct of Santorini Pancreas cartoon The duodenum is divided into 4 portions: 1st and 3rd portions are transverse. 2nd and 4th portions are longitudinal. The normal pancreatic duct may be imaged. The pancreatic duct is considered abnormal if it is >2.0 mm. Pancreatic duct dilation is typically due to stones within Wirsung’s duct from chronic pancreatitis or a stone in the ampulla of Vater. Cartoon- Duodenum Dilated pancreatic duct Acute Pancreatitis Inflammatory disease producing temporary pancreatic changes. Diagnosis is usually based on clinical and laboratory findings. The most common causes of acute pancreatitis are: Biliary tract disease Chronic alcohol abuse. Acute pancreatitis Sonographic findings: Enlarged hypoechoic gland Acute Pancreatitis can take several directions: Resolution Pseudocyst formation Chronic pancreatitis Acute pancreatitis Complications of acute pancreatitis include: Pseudocyst formation Abscess Pancreatic necrosis Hemorrhage Venous thrombosis Pseudoaneurysm formation Pancreatic phlegmon (focal pancreatitis) An inflammatory mass formed by edema and leakage of pancreatic enzymes. It forms as a complication of acute pancreatitis. Definition of a Phlegmon A spreading diffuse inflammatory reaction to an infection which forms a isolated lesion. Acute Pancreatitis Chronic pancreatitis Irreversible destruction by repeated bouts of pancreatic inflammation. Patient presents with intermittent attacks of severe pain. Causes of chronic pancreatitis include: Alcoholism (most common) Cystic fibrosis Hereditary pancreatitis Congenital abnormalities (Pancreas divisum) Blunt abdominal trauma Idiopathic chronic pancreatitis Elevation of serum amylase and lipase are found only during acute attacks of pancreatitis. Sonographic findings include: Small and echogenic gland Calcifications Pancreatic duct dilatation Pseudocyst formation Bile duct dilatation Portal vein thrombosis Chronic Pancreatitis