* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
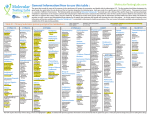
Download CARDIAC- PSYCHOTROPIC DRUG INTERVENTIONS Drug
Discovery and development of beta-blockers wikipedia , lookup
Pharmacognosy wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
Discovery and development of integrase inhibitors wikipedia , lookup
Toxicodynamics wikipedia , lookup
Discovery and development of ACE inhibitors wikipedia , lookup
Discovery and development of direct thrombin inhibitors wikipedia , lookup
Prescription costs wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Neuropharmacology wikipedia , lookup
Theralizumab wikipedia , lookup
Drug interaction wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
CARDIAC- PSYCHOTROPIC DRUG INTERVENTIONS Drug Interactions Facts Rating System (1): Major: The effects are potentially life-threatening or capable of causing permanent damage // (2): Moderate: The effects may cause a deterioration in a patient’s status. Additional treatment, hospitalization or extension of hospital stay may be necessary// (3) : Minor: The effects are usually mild; consequences may be bothersome or unnoticeable, but should not significantly affect the therapeutic outcome. Additional treatment is usually not required. Cholestyramine/Valproic Acid(VPA): (2): Cholestyramine interferes with the GI absorption of VPA, which reduces the concentration and therapeutic effects of VPA. // Action: Administer valproic acid at least three hours BEFORE, but NOT WITHIN three hours following cholestyramine. Monitor the patient’s clinical response and adjust the dose of VPA accordingly. Nifedipine/Fluoxetine:(2): Occasionally, there are increased calcium blocker effects when fluoxetine is administered simultaneously. Since nefazodone is a more potent inhibitor of cytrochrome P3A4 than fluoxetine, it could also inhibit the metabolism of nifedipine, verapamil, and other calcium blockers. There is a question if this interaction would apply to other SSRIs.// Action: monitor for increased effects of calcium blockers if fluoxetine is also prescribed. Propafenone/Fluoxetine: (2): Fluoxetine increases the concentration of propafenone (via CYP 2D6), and thereby markedly delays cardiac conduction leading to increased likelihood of pro-arrhythmia. Given fluoxetine’s and its active metabolite, norfluoxetine long half-life, their effects may appear only after a period of time with the concomitant administration of propafenone. Similarly, it is necessary to observe and monitor the patient after fluoxetine is withdrawn because propafenone’s concentration would decrease. // Action: Select antidepressants that do not inhibit cytochrome P2D6, for example, citalopram, nefazadone, venlafaxine. At the least, if this combination is prescribed, the patient should be monitored for heart rate and prolonged QRS Quinidine/Fluvoxamine: (2): Fluvoxamine coadministered with quinidine produces a modest increase in quinidine concentration (via CYP 3A). For the same reason nefazodone would be expected to have an even greater effect on quinidine than fluvoxamine// Action: Alternative antidepressants should be considered that do not affect cytochrome P3A4 metabolism (e.g.: venlafaxine, paroxetine. Or, another antiarrhythmic could be employed, e.g., procainamide that is not metabolized by the cytochrome P3A4 enzyme system. Monitor EKG for prolonged QT and increased quinidine concentrations. Due to marked pro-arrhythmia quinidine should be avoided if possible. Amiloride/Lithium(2): Caution is needed when Lithium is administered with diuretics, not only amiloride. Sodium loss may reduce the renal clearance of Lithium leading to toxicity. // Action: monitor lithium levels during the first week after starting Amiloride or discontinuing it. Atenolol/Verapamil (2): The effects of both drugs can be decreased by their concomitant use. It is uncertain if the mechanism(s) is an additive or synergistic occurrence. It is known that verapamil can diminish oxidative metabolism for certain beta blockers. // Action: it is essential to monitor cardiac functioning and adjust (decrease) the dose of both drugs as required. Atorvastatin/Hydantoins: (2): Increased metabolism of Atorvastation // Action: The patient should be monitored for clinical response and the atorvastatin appears to be decreased with diminished clinical effectiveness, then a change to pravastatin is suggested since it is less likely to interact with phenytoin. Gamze BALCI CAMSARI, M.D PGY3 Georgetown University Psychiatry 2/23/12 Page 1 Statins/Nefazodone (1): Nefazodone is a known inhibitor of CYP3A4 and atorvastatin is a substrate of the same enzyme. Myopathy and rhabdomyolysis have occurred in patients with HMG-CoA reductase inhibitors alone, or in conjunction with nefazodone. //Action: Monitor for signs and symptoms of myopathy and rhabdomyolysis. Monitor creatine kinase (CK) levels. Carvedilol/Fluoxetine: (2): Fluoxetine increases the plasma concentrations of carvedilol; although the clinical significance is uncertain, increased hypotension or bradycardia may result. // Action: First an alternative SSRI which do not inhibit cytochrome P2D6 should be considered, e.g., citalopram or nefazodone . Or, a beta blocker that does not employ cytochrome P2D6 metabolism, e.g., metoprolol could be considered. Monitor alpha or beta blocking effects if carvedilol and fluoxetine are administered simultaneously. Clopidogrel/Phenobarbital: (Non specified): There are no data to predict the reaction from the concomitant administration of these two drugs. However, since Clopidogrel may interfere with CYP2C9 enzymes, and phenobarbital is partially metabolized by the same enzyme system, an adverse reaction may be reported and this is a potential reaction to be cognizant of. // Action: observe for changes that may occur from coadministration. Digoxin/Fluoxetine: (2): The mechanism for increased digoxin toxicity when fluoxetine was added to a previously stabilized patient is unknown. //Action: Although this is from one case report in a 93 year old female, the increased use of SSRI for depression in the elderly should be cautiously undertaken when the patient is on digoxin. Diltiazem/Buspirone: (2): Diltiazem increases the concentration of buspirone 3.3 to 7.4 times. (via inhibiting CYP3A4 enzymes). Coadminis- tration of buspirone with verapamil, diltiazem, erythromycin and itraconazole substantially increased the plasma concentration of busprione. Action: The use of dihydropyridine calcium channel blockers could prevent this reaction, or the use of an anxiolytic drug that does not employ cytochrome P3A4 enzymes, e.g., lorazepam, diazepam. Monitor for increased buspirone effects, e.g., sedation. Flecainide/Paroxetine: (2): No data available related to the combined use of flecainide and paroxetine, concern does prevail in that paroxetine is a potent inhibitor of cytochrome P2D6 which is how flecainide is metabolized. Action: Monitor QRS duration. Doses may have to be reduced. Mibefradil/Triazolam: (2): Mibefradil markedly increases the plama concentrations of triazolam secondary to its potent inhibition of cytochrome P3A4. Action: Prescribe another hypnotic and try to avoid using mibefradil and triazolam concomitantly. Nefazodone/Sildenafil: (2): Nefazodone and Sildenafil use the same cytochrome P450 metabolic pathways (mainly CYP3A4). Therefore, the practitioner must know that either drug may have less effect than expected for the dosage administered. // Action: Attempt to use an alternative antidepressant. If you need to employ nefazodone with sildenafile, ensure blood levels and/or effectiveness is monitored routinely to achieve expected result. Nitrates/Sildenafile: (1): Sildenafil causes a decrease in systemic arterial pressure and a synergistic and often major decrease in systemic arterial pressure in the presence of nitrates. //Action: Do not concomitantly administer nitrate containing medications and sildenafil. Although other vasodilating agents have different pharmacology, it may be prudent to avoid agents that cause vasodilation when administering sildenafil until more information is available. In addition, patients’ cardiac status needs to be evaluated when administering any erectile dysfunction treatment that may have systemic vasodilatory properties that may potentially lower blood pressure. . Gamze BALCI CAMSARI, M.D PGY3 Georgetown University Psychiatry 2/23/12 Page 2 Verapamil/Oxcarbazepine: (2): Reduction of the 10-monohydroxy metabolite of oxcarbaxzeine that possesses pharmacological activity. The clinical significance of this interaction has not been determined as yet. Action: Monitor clinical effectiveness of oxcarbazepine when coadministered with verapamil. Warfarin/Barbiturates: (1): Warfarin’s clinical efficacy is reduced with the addition and concomitant utilization of barbiturates. Addition of barbiturates to warfarin will decrease its clinical effectiveness, while the withdrawal of barbiturates from the anticoagulant will increase its effectiveness and produce toxicity. Action: It is necessary to monitor anticoagulant therapy when adding or discontinuing barbiturates as either insufficient or excessive anticoagulation activity may occur. It is important to monitor patients for several weeks. Benzodiazepines would have less effect on warfarin. Warfarin/Fluvoxamine: (2): Low dose fluvoxamine can interact significantly with warfarin in the elderly and the effect may persist for up two weeks after stopping the antidepressant. Action: Monitor the effects on warfarin, e.g., increase of INR Warfarin/Quetiapine: (2): Quetiapine competetively inhibits CYP 3A4 and cytochrome 2C9, resulting in increased warfarin activity. Interactions of this type present problems when the enzyme-altering drugs are added to a previously stable patient and may take a few days to two weeks to become evident or dissipate, before the enzyme alteration occurs or resolves. // Action: Warfarin(stable pt)+ Quetiapine Warfarin activity may be increased. Quetiapine +Warfarin No intervention would be required, as the dose of warfarin would be determined by PT and INR Angiotensin Converting Enzyme Inhibitors (ACEI)/Desipramine(TCAs): (2): TCAs decrease ACEI function, especially desipramine that displaces ACE from its receptors. Fluoxetine or tranylcypromine do not change ACEI levels. // Action: close BP monitoring Beta Blockers/Fluvoxamine: (Not applicable significance level): Because atenolol is renally excreted fluvoxamine added to it did not affect the plasma concentration of atenolol. In contrast fluvoxamine does have an impact upon metoprolol and pronolol (both of which are metabolized hepatically).// Action: note the difference in reaction when fluvoxamine administered concomitantly with atenolol then when it is with metoprolol and propanolol. Metoprolol/Diphenhydramine (2): Diphenhydramine inhibits the metabolism of metoprolol (CYP 2D6) Consequently the negative chronotropic and inotropic effects of the drug are prolonged. Action: Monitor for adverse chronotropic and inotropic effects. Gamze BALCI CAMSARI, M.D PGY3 Georgetown University Psychiatry 2/23/12 Page 3