* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Percutaneous Therapeutic Interventions for the Mitral Valve
Survey
Document related concepts
Saturated fat and cardiovascular disease wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Cardiothoracic surgery wikipedia , lookup
Coronary artery disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Myocardial infarction wikipedia , lookup
Jatene procedure wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Transcript
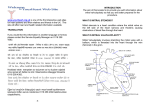
Vanderbilt Heart and Vascular Institute Semiannual Publication | Spring 2014 | Volume 12 | Issue 14 | VanderbiltHeart.com Percutaneous Therapeutic Interventions for the Mitral Valve By Robert N. Piana, M.D., Joseph Fredi, M.D., Michael Petracek, M.D., and Stephen Ball, M.D. Robert N. Piana, M.D. Joseph Fredi, M.D. Michael Petracek, M.D. Stephen Ball, M.D. Percutaneous balloon mitral valvuloplasty (PBMV) has long been utilized to treat rheumatic mitral valve stenosis, but transcatheter options to treat mitral regurgitation have not been available until now. In 2014 transcatheter interventions are emerging as a viable clinical option to treat mitral regurgitation in specific scenarios. Practitioners may now be able to consider these strategies as alternatives to the long-established gold standard of surgical mitral valve repair or replacement. Mitral Stenosis Current guidelines recognize PBMV as the preferred strategy for the treatment of rheumatic mitral stenosis in specific situations. Anatomic suitability of the mitral valve for balloon valvuloplasty is typically determined by an echocardiographic scoring system assigning 0 to 4 points for four parameters: mobility, subvalvular thickening, valve thickness and leaflet calcification. In general, a score ≤8 is considered reasonable for PBMV, provided there is less than moderate mitral regurgitation and no left atrial thrombus. In patients with noncalcified pliable valves, mild subvalvular fusion, and no calcium in the commissures, the procedure can be performed with a high success rate (greater than 90%), low complication rate (less than 3%), and sustained improvement in 80% to 90% of patients over a 3- to 7-year follow-up period.1 This complex technique should only be performed by experienced operators. From a technical standpoint, the intra-atrial septum is punctured to allow access from the right atrium into the left atrium. A large diameter balloon is then passed across the transseptal puncture into the left atrium, positioned across the mitral valve into the left ventricle, and the valve is then dilated to release the fusion of the mitral valve commissures responsible for the stenosis. Current indications for PBMV in symptomatic patients include: 1.Moderate to severe mitral stenosis (valve area ≤1.5 cm2, mean gradient ≥5 mmHg, with pulmonary artery systolic pressure ≥30 mmHg) in patients with New York Heart Association Class II-IV symptoms with appropriate valve morphology (Class I recommendation); 2.Moderate to severe mitral stenosis with non-pliable, calcified valves in patients at high/ prohibitive risk for surgery (Class II); 3.Valve area >1.5 cm2, but pulmonary artery systolic pressure ≥60 mmHg, pulmonary wedge pressure ≥20 mmHg, or transmitral gradient ≥15 mmHg with exercise (Class II) Mitral Regurgitation Mitral regurgitation (MR) can be classified (Table 1, Figure 1) as organic (regurgitation due to intrinsic structural abnormalities of the valve) or functional (structurally normal valve but with MR due to malcoaptation of the valve leaflets). In patients referred for surgery, the etiology of mitral regurgitation is more commonly organic than functional: (Continued on page 3) IN THIS ISSUE 5 Hospital to Home: Optimizing Cardiovascular Care After Hospital Discharge 7 Left Atrial Appendage (LAA) Management: The Non-Pharmacologic Prevention of Stroke in Atrial Fibrillation 10 Incorporating New Guidelines on Cholesterol Management into Clinical Practice VA N D E R B I L T H E A R T | SPRING 2014 Editorial By Robert N. Piana, M.D., Editor, Quinn Wells, M.D., Associate Editor, and Thomas Wang, M.D., Physician-in-Chief Vanderbilt Heart and Vascular Institute (VHVI) continues to grow. Since the last edition of Vanderbilt Heart, VHVI has increased the size and capabilities of its physical facilities, broadened the range of clinical options offered to patients, and accelerated the recruitment of leading physicians and researchers. Robert N. Piana, M.D. Quinn Wells, M.D. Thomas Wang, M.D. On Feb. 3, the VHVI Electrophysiology Lab, Cardiac Catheterization Lab and Cardiac Observation Unit moved to the fifth floor of the Vanderbilt University Hospital Critical Care Tower. The new space includes state-of-the-art angiography and electrophysiology labs, as well as two Hybrid OR suites that are fully equipped to serve as both cardiac catheterization labs and operating rooms. The procedure area utilizes the latest technologies for hemodynamic monitoring and cardiovascular imaging and intervention. The move also includes improvements to the overall experience of patients and their families. Individual holding and recovery rooms provide improved privacy, and a new waiting area is located nearby, affording greater comfort and convenience for family members. A new era in the Department of Cardiac Surgery began in December 2013, with the naming of Dr. Michael Petracek as the permanent chair. He has led the department as interim chair since January 2013. Dr. Petracek has been a national figure in cardiac surgery for more than 30 years, and has helped champion the development of minimally invasive surgical techniques for cardiac valve surgery. He has also been deeply involved in collaborative approaches to catheter-based mitral valve replacement and repair. Dr. Petracek’s appointment invigorates the Department of Cardiac Surgery and signals a continued commitment to the collaborative environment between cardiac surgery and cardiovascular medicine that has fueled the success of VHVI. A key component of VHVI’s growth is the recruitment of nationally and internationally recognized clinicians and physician scientists. VHVI has added nine faculty members since last summer, with six more to join in the coming months. These individuals will contribute to the further expansion of our cardiac transplantation program, the cardio-oncology program, the arrhythmia center and our translational research efforts. We will profile our new faculty members in the next issue of Vanderbilt Heart. VHVI continues to be a leading force regionally and nationally in the provision of cutting edge options for patients. In this edition of Vanderbilt Heart, a multidisciplinary team of cardiologists and cardiac surgeons describe catheter-based approaches for the management of mitral valve disease. Dr. Patrick Whalen and colleagues review the critical role of the left atrial appendage (LAA) in the pathogenesis of atrial fibrillation-related stroke and emerging minimally invasive techniques for LAA closure. Equally important to patient outcomes is the care they receive after hospital discharge. VHVI efforts to optimize this “hospital to home” transition are described by Dr. Muñoz and colleagues. We are excited about the continued growth at VHVI. Continue to follow our progress through Vanderbilt Heart. @ VA N D E R B I L T H E A R T | SPRING 2014 Percutaneous Therapeutic Interventions for the Mitral Valve Continued from page 1 60-70% of surgical referrals are for “degenerative” MR (e.g., myxomatous degeneration or mitral valve prolapse), and 20% for “ischemic” MR and MR due to non-ischemic dilated cardiomyopathy or hypertrophic cardiomyopathy (malcoaptation of the leaflets due to mitral annular dilation or tethering of the mitral leaflets because of ventricular remodeling with papillary muscle displacement). Figure 1: Normal Valve Degenerative MR- Degenerative MRProlapse Fail Table 1: Classification of Mitral Regurgitation Organic (Primary Pathology of the Valve Apparatus) • Degenerative (e.g., Myxomatous Degeneration) • Rheumatic • Endocarditis • Congenital (e.g., Mitral Cleft) • Ruptured Chordae Tendineae/Papillary Muscle Functional (Malcoaptation of the Leaflets Secondary to Myocardial Process) • Ischemic oLeft ventricular remodeling oPapillary muscle displacement with tethering of chordae tendineae oMitral annular dilatation • Dilated Cardiomyopathy • Hypertrophic Cardiomyopathy The timing of surgical repair or replacement for patients with mitral regurgitation is complex. Premature valve surgery exposes the patient to operative risks and the potential need for long-term anticoagulation. Deferring surgery too long could lead to heart failure and a dilated cardiomyopathy. When possible, repair of the mitral valve is preferred over replacement (Class I). However, surgical repair is highly technically demanding, and patients should be referred to experienced centers with excellent surgical outcomes for this procedure. At 10 years, there is a 7%-10% reoperation rate after mitral valve repair (similar to the rate after mitral replacement), and 70% of this is due to the original procedure while only 30% is due to progression of disease.1 The reoperation rate is lower after surgical repair of the posterior leaflet alone as compared to other leaflet abnormalities. If surgical replacement is performed, the chordal apparatus should be preserved in order to maximize preservation of left ventricular function. The advantage of mitral valve replacement with preservation of the chordal apparatus is that MV competence is nearly always assured, LV function is preserved, and postoperative survival is improved compared with MV replacement with chordal resection. The disadvantage of replacement is the use of a prosthetic valve, with the risks of deterioration inherent in tissue valves or the need for anticoagulation inherent in mechanical valves. Now, for the first time, percutaneous treatment of mitral regurgitation is emerging. The MitraClip Percutaneous Mitral Valve Repair System (MCS, Abbott Vascular) was designed to approximate a surgical technique (Alfieri) in which the anterior and posterior leaflets are stitched together at one spot, thereby creating a double orifice mitral valve with less MR (Figure 2). As mitral annular dilatation often contributes to functional MR, the surgical Alfieri technique also generally incorporates a mitral annuloplasty in which a ring is placed to shrink the dilated mitral annulus. In the emerging (Continued on page 4) Figure 2: Left panel shows MitraClip prior to deployment. Right panel shows schematic of resultant double orifice mitral valve after MitraClip deployment. (Used with permission from Abbott Vascular) # VA N D E R B I L T H E A R T | SPRING 2014 Percutaneous Therapeutic Interventions for the Mitral Valve Continued from page 3 transcatheter approach, a transseptal puncture is performed allowing access from the femoral vein to the left atrium. From this position, using transesophageal guidance, MCS is delivered through the catheter to pin the anterior and posterior mitral valve leaflets together in one spot. This technique does not incorporate mitral annuloplasty. In October 2013, the FDA approved the MCS for the treatment of degenerative MR in patients who are poor candidates for surgery, based on the Endovascular Valve Edge-to-Edge Repair Study (EVEREST) studies. EVEREST I was a single arm feasibility registry of 55 patients establishing safety of the MCS procedure.2 EVEREST II randomized 279 patients with moderately severe or severe (grade 3+ or 4+) mitral regurgitation in a 2:1 ratio to undergo either percutaneous repair or conventional surgery. The study was designed to show non-inferiority of MCS in terms of efficacy, and superiority in safety. Safety was superior with MCS (48% vs 15%), but this was driven entirely by more bleeding with surgery.3 There were no differences in death, stroke, myocardial infarction or infection. The efficacy of MCS proved inferior to surgery. The primary efficacy endpoint of freedom from death, from surgery or mitral-valve dysfunction, and from grade 3+ or 4+ mitral regurgitation at 12 months was achieved in 55% of the MCS group compared to 73% with surgery (p=0.007). Mitral valve surgery was required by one year in 20% after MCS versus 2% in the surgical arm (p<0.001). Thus, MCS was found to be inferior to surgical repair or replacement of the mitral valve in this population. Interestingly, at four-year followup very few additional surgeries were required in either group (cumulative rate at four years of 24.8% versus 5.5%, p<0.001) and there was no difference in the prevalence of moderate-severe and severe MR or mortality.4 This suggests that the results with MCS at one year are durable. Based on these findings, application of MCS has now been focused on patients considered too high risk for surgery. EVEREST II enrolled 78 patients in a High Risk Registry (EVEREST II HRR) and the Real World Expanded Multicenter Study of the MitraClip System High Risk (REALISM HR) included 273 patients. These were pooled and retrospectively analyzed to support FDA approval of the device. At one-year followup in this high-risk population, there was a statistically significant decrease in the left ventricular diastolic and systolic volumes, a 48% reduction in hospitalization rate, and a decrease in New York Heart Association class III/IV from 82% to 17%.5 As a result, the FDA advisory panel recommended approval of the premarket approval application (PMA) for MCS in March 2013, and in October 2013 the FDA followed suit. The MCS is indicated for the percutaneous reduction of significant symptomatic MR (≥ 3+) due to primary abnormality of the mitral apparatus (degenerative MR) in patients who have been determined to be at prohibitive risk for mitral valve surgery by a heart team (a cardiac surgeon experienced in mitral valve surgery and a cardiologist experienced in mitral valve disease) and in whom existing comorbidities would not preclude the expected benefit from reduction of the mitral regurgitation. Vanderbilt Heart and Vascular Institute plans to participate in the Clinical Outcomes Assessment of the MitraClip Percutaneous Therapy for Extremely High Surgical Risk Patients (COAPT) Trial. Key inclusion criteria include: • Symptomatic functional mitral regurgitation (≥3+) of either ischemic or non-ischemic etiology; • Not a suitable candidate for open mitral valve surgery in the judgment of the cardiothoracic surgeon investigator: • NYHA functional class II, III, or ambulatory IV; • At least one hospitalization for heart failure in the 12 months prior to enrollment and/or BNP ≥400 pg/mL or NT proBNP ≥1600 pg/mL measured within 90 days prior to enrollment; • Primary regurgitant jet from the A2 and P2 scallops (and if secondary jet exists, it is clinically insignificant) As commercialization of this device begins, experienced heart teams will need to apply this technology judiciously in patients to optimize outcomes. 1.Bonow RO, Carabello BA, Chatterjee K et al. 2008 focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1998 guidelines for the management of patients with valvular heart disease). Endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Journal of the American College of Cardiology 2008;52:e1-142. 2.Feldman T, Kar S, Rinaldi M et al. Percutaneous mitral repair with the MitraClip system: safety and midterm durability in the initial EVEREST (Endovascular Valve Edge-toEdge REpair Study) cohort. Journal of the American College of Cardiology 2009;54:686-94. 3.Feldman T, Foster E, Glower DD et al. Percutaneous repair or surgery for mitral regurgitation. The New England journal of medicine 2011;364:1395-406. 4.Mauri L, Foster E, Glower DD et al. 4-year results of a randomized controlled trial of percutaneous repair versus surgery for mitral regurgitation. Journal of the American College of Cardiology 2013;62:317-28. 5.Minha S, Torguson R, Waksman R. Overview of the 2013 Food and Drug Administration Circulatory System Devices Panel meeting on the MitraClip Delivery System. Circulation 2013;128:864-8. $ VA N D E R B I L T H E A R T | SPRING 2014 Hospital to Home: Optimizing Cardiovascular Care After Hospital Discharge By Daniel Muñoz, M.D., M.P.A., Robin Steaban, M.S.N., R.N., Keith Churchwell, M.D., F.A.C.C., Mark Glazer, M.D., F.A.C.C., and Brittany Cunningham, M.S.N., R.N. Daniel Muñoz, M.D., M.P.A. These are exciting times in cardiovascular patient care. We practice in an era of rapidly advancing cardiovascular therapeutics, but this progress comes with an increasingly important challenge: to ensure that patients continue to receive the right care upon discharge from the hospital, focusing on preventing avoidable and costly hospital readmissions.1 Across the United States, the readmission of Medicare patients alone is estimated to cost approximately $26 billion per year, of which $17 billion is spent on return trips to the hospital that might very well have been avoidable.2 The federal government has made reducing readmissions a central pillar of its approach to controlling costs while ensuring quality care, an approach codified in the Patient Protection and Affordable Care Act of 2010.3 In response, hospital systems around the country, including Vanderbilt, have embarked on an examination of how to systematically create effective care transitions out of the hospital. Robin Steaban, M.S.N., R.N. Keith Churchwell, M.D., F.A.C.C. Several studies offer key insights into the scope and complexity of the readmission challenge. First, the data make clear that the readmission challenge is not disease-specific. Patients admitted with heart failure, acute myocardial infarction, or pneumonia are more often readmitted for a different diagnosis, a phenomenon that speaks to their generalized vulnerability to illness.4 Second, the data also show that reducing readmissions requires a multidisciplinary approach anchored in both the inpatient and outpatient realms, rather than a narrow approach that exclusively focuses on a single element of care.5 Third, the evidence supports the idea that timely outpatient follow-up, ideally within two weeks of hospital discharge, may help patients avoid readmission.6 From these lessons have emerged several patient-centered quality initiatives at the Vanderbilt Heart & Vascular Institute. Vanderbilt Acute MyocardiaI Infarction Task Force In spring 2012, the Vanderbilt Acute Myocardial Infarction (MI) Task Force was formed to tackle the problem of hospital readmissions after MI. Under the capable leadership of Brittany Cunningham, MSN, RN, this committee formulated a patient-centered plan to lower readmission rates. A review of the literature at the time suggested that there was no (Continued on page 6) Figure 1: AMI 30 Day All Cause Unplanned Readmission Rates: Medicare 65+ (Readmission back to Vanderbilt only) 14.0% • • • • • • • • • • •• • • • • • • • • • • • • • • • Dec-13 • • Nov-13 •• Oct-13 • • • Sep-13 • Aug-13 10.0% Jul-13 12.0% Jun-13 Mark Glazer, M.D., F.A.C.C. 8.0% 6.0% • Rolling 12 month readmission rate • VUMC Pillar Goal: All Payors 4.0% 2.0% May-13 Apr-13 Mar-13 Feb-13 Jan-13 Dec-12 Nov-12 Oct-12 Sep-12 Aug-12 Jul-12 0.0% Brittany Cunningham, M.S.N., R.N. % VA N D E R B I L T H E A R T | SPRING 2014 Hospital to Home: Optimizing Cardiovascular Care After Hospital Discharge Continued from page 5 Following hospital discharge, each post-MI patient receives a phone call from an office nurse within 72 hours to review and confirm medications, answer any questions, and to ensure proper, timely outpatient follow-up. The program aims to have every post-MI patient seen in the office by a provider within 10 days of discharge. Using this approach, there has been a significant observed decline in MI readmission rates at Vanderbilt. (Figure 1) single identifiable intervention to achieve the goal. Consequently, the Vanderbilt approach has been deliberately multi-faceted, with a major emphasis on discharge planning and closer follow-up after discharge. Daily transition "huddles" of nurses, social workers and physicians occur to identify those patients with MI and to begin assessing personalized, patient-specific discharge needs. These needs often include home health nursing care and cardiac rehabilitation. Extra time is devoted at discharge to two key areas: 1) discussing the proper administration of home medications, and 2) proactively addressing any patient questions or concerns related to medication list, a list that has often undergone modification during a hospital stay. Following hospital discharge, each post-MI patient receives a phone call from an office nurse within 72 hours to review and confirm medications, answer any questions, and to ensure proper, timely outpatient follow-up. The program aims to have every post-MI patient seen in the office by a provider within 10 days of discharge. Using this approach, there has been a significant observed decline in MI readmission rates at Vanderbilt. Efforts continue to further reduce MI readmissions at Vanderbilt and to apply lessons learned to help guide institutional approaches to a host of other cardiovascular conditions. American College of Cardiology Patient Navigator Program Vanderbilt is one of 11 hospitals nationwide chosen to participate in the innovative, recently unveiled Patient Navigator Program (PNP). Sponsored by the American College of Cardiology with founding support from AstraZeneca, the PNP was developed to help hospitals address high readmission rates by increasing the focus on the needs of vulnerable heart disease patients not only while they are in the hospital but following discharge (American College of Cardiology: Patient Navigator Program, 2013). The hope is that Vanderbilt, with the help of PNP, can develop and enhance a culture of patientcentered care that can be used in other hospitals around the country. Hospitals selected to participate in the PNP will be provided improvement strategies and toolkits developed from other ACC programs such as the Hospital to Home (H2H) Initiative and the Get With the Guidelines Registry. These ACC programs include more than 1,500 participant hospitals in the United States. Conclusion Institutional and national focus on safe, effective transitions out of the hospital while preventing readmissions not only makes sound financial sense, but most importantly, is in the best interest of our patients. To learn more about the ongoing initiatives at Vanderbilt, please visit us at: VanderbiltHealth.com/heart. 1.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. The New England journal of medicine 2009; 360:1418-28. 2.The Revolving Door Syndrome: A Report on U.S. Hospital Readmissions, : The Robert Wood Johnson Foundation; February 2013. 3.Kocher RP, Adashi EY. Hospital readmissions and the Affordable Care Act: paying for coordinated quality care. JAMA : the journal of the American Medical Association 2011; 306:1794-5. 4.Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA : the journal of the American Medical Association 2013; 309:355-63. 5.Lindenfeld J, Albert NM, Boehmer JP, et al. HFSA 2010 Comprehensive Heart Failure Practice Guideline. Journal of cardiac failure 2010; 16:e1-194. 6.Hernandez AF, Greiner MA, Fonarow GC, et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA : the journal of the American Medical Association 2010; 303:1716-22. ^ VA N D E R B I L T H E A R T | SPRING 2014 Left Atrial Appendage (LAA) Management: The Non-Pharmacologic Prevention of Stroke in Atrial Fibrillation S. Patrick Whalen, M.D., Marshall Crenshaw, M.D., Christopher Ellis, M.D., and Robert N. Piana, M.D. S. Patrick Whalen, M.D. Marshall Crenshaw, M.D. Christopher Ellis, M.D. Robert N. Piana, M.D. Atrial fibrillation (AF) is the most common sustained arrhythmia. It has an estimated prevalence of 1% in the adult population and affects more than 2.5 million in the United States. AF is responsible for 17% of all strokes (or 135,000 annually).1,2 Whether paroxysmal or persistent, the two guiding principles in AF treatment are symptom control and stroke prevention. A majority of strokes in non-valvular AF originate in the left atrial appendage (LAA). The LAA is a long, tubular structure with a narrow neck and large surface area prone to stasis and thrombus formation (See Figure 1). Up to 90% of thrombi visualized by transesophageal echo in AF patients are in the LAA.3.4 Stroke risk in AF is driven largely by patient comorbidities and may involve LAA morphology, abnormal endothelial function and platelet Figure 1: Cast of left activation.5,6 Standard practice involves oral anticoagulation atrial appendage (OAC) for the prevention of systemic thromboembolism in a majority of AF patients. This has traditionally involved warfarin but has expanded to include novel oral anticoagulants. The CHADS2 and CHA2DS2-VASc scoring systems use patient comorbidities to predict embolic risk and the HAS-BLED scoring system may aid in risk assessment for adverse effects of systemic anticoagulation.7,8 A large percentage of patients who are candidates for OAC are not prescribed, do not take, or discontinue therapy due to real or perceived risk of bleeding or falls, difficulty with monitoring, non-compliance, patient preference, physician awareness, dietary or drug interactions, or gender disparities.9-11 Given the morbidity of AF-associated stroke and the challenges of OAC therapy, an effective non-pharmacologic option is appealing. Surgical Approaches to LAA Closure The surgical approach to LAA management involves amputation or occlusion and has traditionally been performed at the time of cardiac surgery. While several studies have shown safety and feasibility of LAA closure,12,13 the effectiveness of surgical closure has been questioned and is often incomplete at follow-up.14 Additionally, no large-scale randomized trials have tested the efficacy of surgical closure of the LAA for stroke prevention. A new device (Atriclip, AtriCure Inc, Westchester, Ohio) specifically designed for LAA closure is now being used. The clip is composed of two parallel, straight, rigid titanium tubes covered with a knit-braided polyester. It is designed to be implanted from outside the heart through a thoracoscopic approach and can be done as a stand-alone procedure or in combination with minimally invasive MAZE surgery for AF.15 (See Figure 2) (Continued on page 8) Figure 2: Left: Atriclip; Right: thoracoscopic approach & VA N D E R B I L T H E A R T | SPRING 2014 Left Atrial Appendage (LAA) Management: The Non-Pharmacologic Prevention of Stroke in Atrial Fibrillation Continued from page 7 Non-Surgical Approaches to LAA Closure Non-surgical LAA closure may be accomplished using one of several devices implanted percutaneously. Depending on which device is used, this is done with a purely endocardial or a combined endocardial/epicardial approach. Endocardial: Early studies providing proof of concept and feasibility of percutaneous LAA occlusion utilized the PLAATO System (eV3, Plymouth, Minn.) and the Amplatzer Septal Occluder (AGA Medical Corp., Golden Valley, Minn.), initially designed for closure of atrial septal defects (ASDs) and patent foramen ovale (PFO). The Amplatzer Cardiac Plug (St. Jude Medical, Minneapolis, Minn.) has evolved out of the septal occluder technology, and is dedicated for LAA closure. The WATCHMAN (Boston Scientific, Maple Grove, Minn.) device is also used for this purpose. Epicardial: The LARIAT (SentreHEART Inc. Redwood City, Calif.) device is used for epicardial LAA ligation via subxiphoid access. During the procedure, a 40-mm pre-tied radiopaque suture loop is used to ligate the LAA. The LARIAT device has been approved for tissue approximation and is currently available at Vanderbilt Heart. LAA closure appears to be feasible with appropriate anatomy and 96% implant success has been reported with 98% complete occlusion at one year including those with initial leaks.16,17 (See Figure 3) In December 2013, the FDA's Circulatory System Devices Panel voted 13-1 to recommend marketing approval for the WATCHMAN device. Watchman consists of a self-expanding nitonol frame which is delivered via transseptal access to the left atrium and secured into the LAA via fixation barbs. The device surface facing the atrial wall is covered by a porous polyethylene terephthalate membrane. Final FDA approval is pending. Figure 3: Procedural fluoroscopic images of LARIAT LAA closure and appearance of closure from left atrial side two months after implant. The WATCHMAN Left Atrial Appendage System for Embolic Protection in Patients with AF (PROTECT-AF) study provides us with randomized data comparing LAA occlusion to warfarin in 542 patients. Subjects in the device arm were on warfarin briefly, and then treated with dual anti-platelet therapy for six months after implant. The device was successfully implanted in 88% of cases and 92% of patients discontinued warfarin within six months. At 1065 patient-years of follow-up the study showed device closure to be noninferior to warfarin. There was a significant decline in procedure-related complications (largely pericardial effusion) with operator experience from 7.7% to 3.7%.18 Preliminary results from the WATCHMAN LAA Closure Device in Patients with AF Versus Long Term Warfarin Therapy (PREVAIL) showed implant success of 95% and adverse safety events only occurring in 2.2% of patients.19 Four-year follow-up data from the PROTECT AF trial have demonstrated a 40% relative risk reduction (stroke, cardiovascular/unexplained death, systemic embolization) relative to warfarin.20 There are limited data to suggest that the WATCHMAN device may be implanted safely in patients with absolute contraindications to OAC by placing them on Plavix for six months and aspirin for life.21 These studies represent compelling data that LAA occlusion may change the natural history of stroke in patients with non-valvular AF. The results are encouraging, but enthusiasm should be tempered as it does not include comparison to novel oral anticoagulant therapy, which has changed this landscape over the last few years. AF is a common condition and AF-related stroke has catastrophic consequences. The LAA is critical to the pathogenesis of stroke and as such has been called “our most lethal human attachment.”22 Medical therapy is effective but there are significant barriers, both real and perceived to OAC in AF patients. LAA occlusion using surgical and catheter techniques may reduce long-term stroke risk without the adverse effects of chronic anticoagulation and is a rapidly evolving area of research and clinical practice at Vanderbilt Heart and Vascular Institute. * VA N D E R B I L T H E A R T | SPRING 2014 All Cause Mortality Hazard Ratio with Watchman, 0.66 (95% CI, 0.45 – 0.98) Patients with Events - % 0.30 0.20 • Watchman • Control P = 0.0379 0.10 0.00 No. at Risk Watchman Control 0 6 12 18 24 30 36 Time in Months 42 48 54 60 463 244 404 233 389 222 381 216 373 204 341 163 330 150 294 125 202 92 360 193 352 177 Figure 3: The WATCHMAN Device (left) and All-cause mortality data from PROTECT AF trial at four years (right) (used with permission, Boston Scientific) 1. Go, A. S., et al. (2001). "Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study." Jama 285(18): 2370-2375. 2. Roger, V. L., et al. (2011). "Heart disease and stroke statistics--2011 update: a report from the American Heart Association." Circulation 123(4): e18-e209. 3. Thambidorai, S. K., et al. (2005). "Utility of transesophageal echocardiography in identification of thrombogenic milieu in patients with atrial fibrillation (an ACUTE ancillary study). ." J Am Coll Cardiol 96: 945-941 4. Beinart, R., et al. (2011). "Left atrial appendage dimensions predict the risk of stroke/TIA in patients with atrial fibrillation." J Cardiovasc Electrophysiol 22(1): 10-15. 5. Al-Saady, N. M., et al. (1999). "Left atrial appendage: structure, function, and role in thromboembolism." Heart 82(5): 547-554. 6. Di Biase, L., et al. (2012). "Does the left atrial appendage morphology correlate with the risk of stroke in patients with atrial fibrillation? Results from a multicenter study." J Am Coll Cardiol 60(6): 531-538. 7. Pisters, R., et al. (2010). "A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey." Chest 138(5): 1093-1100. 8. Fuster, V., et al. (2011). "2011 ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 Guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines developed in partnership with the European Society of Cardiology and in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society." J Am Coll Cardiol 57(11): e101-198. 9. Camm, A. J., et al. (2012). "2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association." Eur Heart J 33(21): 2719-2747. 10. Hart, R. G., et al. (2007). "Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation." Ann Intern Med 146(12): 857-867. 11. Contractor, T. and A. Khasnis (2011). "Left Atrial Appendage Closure in Atrial Fibrillation: A World without Anticoagulation?" Cardiol Res Pract 2011: 752808. 12. Crystal, E., et al. (2003). "Left Atrial Appendage Occlusion Study (LAAOS): a randomized clinical trial of left atrial appendage occlusion during routine coronary artery bypass graft surgery for long-term stroke prevention." Am Heart J 145(1): 174-178. 13. Garcia-Fernandez, M. A., et al. (2003). "Role of left atrial appendage obliteration in stroke reduction in patients with mitral valve prosthesis: a transesophageal echocardiographic study." J Am Coll Cardiol 42(7): 1253-1258. 14. Katz, E. S., et al. (2000). "Surgical left atrial appendage ligation is frequently incomplete: a transesophageal echocardiograhic study." J Am Coll Cardiol 36(2): 468-471. 15. Ailawadi, G., et al. (2011). "Exclusion of the left atrial appendage with a novel device: early results of a multicenter trial." J Thorac Cardiovasc Surg 142(5): 1002-1009, 1009. e1001. 16. Bartus, K., et al. (2013). "Percutaneous left atrial appendage suture ligation using the LARIAT device in patients with atrial fibrillation: initial clinical experience." J Am Coll Cardiol 62(2): 108-118. 17. Massumi, A., et al. (2013). "Initial experience with a novel percutaneous left atrial appendage exclusion device in patients with atrial fibrillation, increased stroke risk, and contraindications to anticoagulation." Am J Cardiol 111(6): 869-873. 18. Holmes, D. R., et al. (2009). "Percutaneous closure of the left atrial appendage versus warfarin therapy for prevention of stroke in patients with atrial fibrillation: a randomised non-inferiority trial." Lancet 374(9689): 534-542. 19. Holmes, D. (2013). "Randomized Trial of LAA Closure vs Warfarin for Stroke/Thromboembolic Prevention in Patients with Non-valvular Atrial Fibrillation (PREVAIL)." Interventional Innovation Summit Lecture. CIT. CNCC, Beijing, China. 20 March 2013. 20. Reddy V, D. S., Sievert H, et al (2013). "Long term results of PROTECT-AF: the mortality effects of left atrial appendage closure versus warfarin for stroke prophylaxis in AF. ." Heart Rhythm Society LBCT Scientific Sessions, May 9, 2013, Denver, Colorado. 21. Reddy, V. Y., et al. (2013). "Left atrial appendage closure with the Watchman device in patients with a contraindication for oral anticoagulation: the ASAP study (ASA Plavix Feasibility Study With Watchman Left Atrial Appendage Closure Technology)." J Am Coll Cardiol 61(25): 2551-2556. 22. Johnson, W. D., et al. (2000). "The left atrial appendage: our most lethal human attachment! Surgical implications." Eur J Cardiothorac Surg 17(6): 718-722. ( VA N D E R B I L T H E A R T | SPRING 2014 Incorporating New Guidelines on Cholesterol Management into Clinical Practice By Raphael See, M.D., and Sergio Fazio, M.D., Ph.D. Raphael See, M.D. Sergio Fazio, M.D., Ph.D. While the 2013 updated guidelines bear a number of similarities to NCEP-ATP III, there are several key differences which should be taken into account when deciding how to best manage a patient’s cholesterol and CV risk in the clinical setting. In November 2013 new American College of Cardiology/American Heart Association (ACC/AHA) guidelines were published regarding cholesterol management for the prevention of cardiovascular (CV) events1, 2 as a proposed update to the previous National Cholesterol Education Program and Adult Treatment Program III guidelines (NCEP-ATP III) published in 2002.3 While the 2013 updated guidelines bear a number of similarities to NCEP-ATP III, there are several key differences which should be taken into account when deciding how to best manage a patient’s cholesterol and CV risk in the clinical setting. Key differences in the 2013 guidelines The guiding and fundamental principle of NCEP-ATP III is individually tailored low-density lipoprotein cholesterol (LDL-C) treatment goals in proportion to an individual’s predicted CV risk. In brief, NCEP-ATP III suggests that all subjects with prior atherosclerotic CV disease or with diabetes be placed in the high-risk category, and recommends using the Framingham Risk Score to assess the 10-year risk for CV events in all other patients. Escalating levels of predicted risk (i.e. low, moderate, or high) warrant increasingly aggressive LDL-C treatment goals (i.e. <160 mg/dL, <100-130 mg/dL, or <70100 mg/dL). Like NCEP-ATP III, the 2013 ACC/AHA guidelines also begin with an estimation of 10year CV risk; however, this risk estimate is now made using a new tool called the Pooled Cohort Equation (PCE).4, 5 The Framingham Risk Score has been previously criticized due to the Framingham original cohort being a relatively homogeneous population. The PCE attempts to reflect a more diverse, contemporary United States population by incorporating additional data from several large racially and geographically diverse cohort studies and also adds ethnicity and diabetes as additional clinical factors. As the PCE is mathematically complex, a spreadsheet-based online calculator (http://my.americanheart. org/cvriskcalculator) is available and several unofficial applications for smartphones and tablets exist as well. Following CV risk assessment with the PCE, lipid-lowering therapy is then chosen according to the level of 10-year risk. In contrast to NCEP-ATP III, the 2013 guidelines no longer recommend specific LDL-C target levels but instead propose fixed-dose statin treatment with potency in proportion to the predicted 10-year CV risk (Table 1). Using this strategy, it is recommended that the highest risk individuals – either clinical atherosclerotic CV disease or LDL-C levels >190 mg/dL – receive high-potency statin treatment. Otherwise, individuals with predicted 10-year risk for CV events >7.5% by the PCE qualify for moderate-potency statin treatment. Moderate-potency statin therapy is recommended for diabetics in general, but higher risk individuals with diabetes (10-year risk >7.5%) should receive a high-potency statin. Lower-potency statin treatment is only recommended when otherwise indicated higher potency treatments are not tolerated. In addition, nonstatin treatments are not recommended as first-line agents due to lack of evidence clearly associating decreased adverse CV outcomes with their use. This new dosing strategy reflects the greatest departure from NCEP-ATP III as the emphasis was previously on achieving specific LDL-C targets, with the specific choice of drug being less important. The authors of the 2013 guidelines cite two main reasons for this new approach. First, by simplifying the recommended statin treatment regimens (and removing the need for dose titration), the authors hope to make lipid management more accessible to BL VA N D E R B I L T H E A R T | SPRING 2014 Table 1: Clinical characteristics warranting either high- or low-potency statin treatment. When not specified otherwise, these recommendations cover individuals 40-75 years of age. High-potency statin indicated (>50% LDL-C expected reduction) atorvastastin 40-80 mg, rosuvastatin 20-40 mg • Clinical atherosclerotic coronary artery disease (any age) • Fasting LDL-C >190 mg/dL (age >20 years) • Diabetes AND 10-year risk >7.5% Moderate-potency statin indicated (35-50% LDL-C expected reduction) atorvastatin 10-20 mg, rosuvastatin 5-10 mg, simvastatin 20-40 mg, pravastatin 40-80 mg, lovastatin 40 mg, fluvastatin 40 mg BID • Diabetes AND 10-year risk <7.5% • 10-year risk >7.5% • Age >75 years all health care providers. Second, the pivotal randomized clinical trials (RCT) demonstrating benefit with statin treatment did not target specific LDL-C levels but instead used fixed statin dosing in their primary design. In a sense, using fixed-dose statin treatment may therefore represent evidence-based practice more reflective of RCT data. The only statement about LDL-C lowering in these guidelines is the expected range of 35% -50% reduction for the moderate potency regimen and >50% reduction for the high potency regimen, which can be used to determine patient adherence. Special exceptions Of note, the 2013 guidelines are purposefully silent regarding statin use in patients receiving hemodialysis or with systolic congestive heart failure despite clinically apparent high CV risk. In these populations, RCTs of statin use have not clearly demonstrated a preventative benefit.6, 7 Similarly, high-potency statin use has not consistently demonstrated a preventative benefit above and beyond moderate-potency regimens in individuals >75 years of age, and an individualized approach is recommended, taking potential risk for drug interactions, toxicity, and patient preferences into account. Points to consider Though intended to simplify and facilitate appropriate statin treatment, controversy remains concerning the 2013 update. The PCE has been criticized due to lack of prospective validation and an apparent tendency to overestimate CV event risk.8 Others have taken issue with the decision to exclusively use RCT-derived evidence in the formulation of these recommendations despite the existence of other high-quality, non-RCT data. As with any set of consensus guidelines, it is always important to consider the individual being treated, taking care not to let guidelines replace or supersede clinical judgment. For example, according to the 2013 guidelines, statin therapy would not be recommended for a normotensive 65-year-old woman with total cholesterol of 220 mg/dL, HDL-C of 40 mg/dL, and LDL-C of 180 mg/dL as her 10-year CV risk is 5.9% by the PCE. Similarly, a 52-year-old man with multiple coronary stents who is tolerating high potency statin treatment with an LDL-C of 120 mg/dL (from a baseline of 205 mg/dL) would not receive additional therapy to drive the LDL lower according to these new guidelines. Reflecting the controversial nature of the new guidelines, it is important to note that they have not been endorsed by the American Diabetes Association, the Endocrine Society, or the National Lipid Association, who all continue to support a strategy based on targeting riskappropriate LDL-C goals. Conclusion The updated 2013 cholesterol treatment guidelines attempt to address a changing United States demographic and simplify decision-making in primary and secondary prevention. While the impact of these changes remains to be seen, the importance of personalizing the care of each patient has not changed. (Continued on page 12) BM VA N D E R B I LT U N I V E R S I T Y Vanderbilt Heart Communications MCE, 5th floor, Ste. 5140 1215 21st Ave. S. Nashville, TN 37232-8802 NONPROFIT ORG. U.S. POSTAGE PAID NASHVILLE, TN PERMIT NO. 3432 Incorporating New Guidelines on Cholesterol Management into Clinical Practice Continued from page 11 1. Stone NJ, Robinson J, Lichtenstein AH, Bairey Merz CN, Lloyd-Jones DM, Blum CB, McBride P, Eckel RH, Schwartz JS, Goldberg AC, Shero ST, Gordon D, Smith SC, Jr., Levy D, Watson K, Wilson PW. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: A report of the American College of Cardiology/American Heart Association task force on practice guidelines. Journal of the American College of Cardiology. 2013 2. Stone NJ, Robinson J, Lichtenstein AH, Merz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd-Jones DM, McBride P, Schwartz JS, Shero ST, Smith SC, Jr., Watson K, Wilson PW. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: A report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation. 2013 3. Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel iii) final report. Circulation. 2002;106:3143-3421 4. Goff DC, Jr., Lloyd-Jones DM, Bennett G, Coady S, D'Agostino RB, Sr., Gibbons R, Greenland P, Lackland DT, Levy D, O'Donnell CJ, Robinson J, Schwartz JS, Shero ST, Smith SC, Jr., Sorlie P, Stone NJ, Wilson PW. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: A report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation. 2013 5. Goff DC, Jr., Lloyd-Jones DM, Bennett G, O'Donnell CJ, Coady S, Robinson J, D'Agostino RB, Sr., Schwartz JS, Gibbons R, Shero ST, Greenland P, Smith SC, Jr., Lackland DT, Sorlie P, Levy D, Stone NJ, Wilson PW. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: A report of the American College of Cardiology/American Heart Association task force on practice guidelines. Journal of the American College of Cardiology. 2013 6. Kjekshus J, Apetrei E, Barrios V, Bohm M, Cleland JG, Cornel JH, Dunselman P, Fonseca C, Goudev A, Grande P, Gullestad L, Hjalmarson A, Hradec J, Janosi A, Kamensky G, Komajda M, Korewicki J, Kuusi T, Mach F, Mareev V, McMurray JJ, Ranjith N, Schaufelberger M, Vanhaecke J, van Veldhuisen DJ, Waagstein F, Wedel H, Wikstrand J. Rosuvastatin in older patients with systolic heart failure. The New England journal of medicine. 2007;357:2248-2261 7. Fellstrom BC, Jardine AG, Schmieder RE, Holdaas H, Bannister K, Beutler J, Chae DW, Chevaile A, Cobbe SM, Gronhagen-Riska C, De Lima JJ, Lins R, Mayer G, McMahon AW, Parving HH, Remuzzi G, Samuelsson O, Sonkodi S, Sci D, Suleymanlar G, Tsakiris D, Tesar V, Todorov V, Wiecek A, Wuthrich RP, Gottlow M, Johnsson E, Zannad F. Rosuvastatin and cardiovascular events in patients undergoing hemodialysis. The New England journal of medicine. 2009;360:1395-1407 8. Ridker PM, Cook NR. Statins: New american guidelines for prevention of cardiovascular disease. Lancet. 2013;382:1762-1765 Visit VanderbiltHeart.com for more information on Vanderbilt Heart programs