* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Effects of calcium channel blockers on renal function, advanced
Survey
Document related concepts
NK1 receptor antagonist wikipedia , lookup
Discovery and development of antiandrogens wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Adherence (medicine) wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Transcript
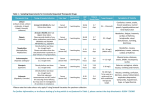
Effects of calcium channel blockers on renal function, advanced glycation end products (AGEs) and soluble receptor for AGEs in diabetic nephropathy Yoshiko Sakamoto, MD1, Nobuharu Fujiwara, MD 1, 2, Tsukasa Nakamura, MD 1, 2, Masayoshi Takeuchi, PhD3,Kazuhisa Kodama, MD 1, Yutaka Hikichi, MD1, Jun-ichi Oyama, MD1, Sho-ichi Yamagishi, MD 4, Koichi Node, MD 1 1 Department of Cardiovascular Medicine, Saga University, Saga, Japan 2 Division of Nephrology, Department of Internal Medicine, Shinmatsudo Central General Hospital, Matsudo, Chiba, Japan 3 Department of Advanced Medicine, Medical Research Institute, Kanazawa Medical University, Japan 4 Department of Pathophysiology and Therapeutics of Diabetic Vascular Complications, Kurume University School of Medicine, Kurume, Japan Address for correspondence: Koichi Node, MD Department of Cardiovascular Medicine, Saga University 5-1-1 Nabeshima, Saga 849-8501, Japan Tel: +81-952-34-2364 Fax: +81-952-34-2089 E-mail:[email protected] Short title: Renoprotection: Benidipine versus amlodipine Source of support: none We certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript. Abstract Objectives: This study was designed to compare the effects of the calcium channel blockers (CCBs), benidipine and amlodipine, on renal function, advanced glycation end products (AGEs) and the soluble receptor for AGE (RAGE) in patients with diabetic nephropathy associated with hypertension and microalbuminuria. Methods: Sixty patients who had been treated with angiotensin II receptor blockers (ARBs) were assigned randomly to also receive either amlodipine 5 mg/day (n=30) or benidipine 8 mg/day (n=30). Urinary albumin excretion (UAE), urinary liver-type fatty acid binding protein (L-FABP), serum AGEs, and serum soluble RAGEs were measured before and after 12 months of treatment. Results: Prior to CCB therapy, serum AGEs (R=0.814, p<0.001) and soluble RAGEs (R=0.696, p<0.001) correlated with urinary L-FABP, while serum RAGEs correlated with serum AGEs (R=0.887, p<0.001). In addition, serum AGEs (R=0.892, p<0.001) and serum RAGEs (R=0.787, p<0.001) correlated with UAE. After 12 months of treatment, systolic and diastolic blood pressures showed similar reductions in the two groups. Serum creatinine and estimated glomerular filtration rate (eGFR) showed no changes throughout the study period. Benidipine caused a significant reduction in UAE (p<0.001), urinary L-FABP (p<0.001), serum AGEs (p<0.001) and soluble RAGE (p<0.001), whereas amlodipine did not. Conclusions: These results suggested that L-FABP and the AGE/RAGE system are associated with progression of diabetic nephropathy, and that the addition of benidipine, but not of amlodipine, to an ARB ameliorated UAE, L-FABP and the AGE/RAGE system in hypertensive patients with diabetic nephropathy. Key words: chronic kidney disease, diabetic nephropathy, calcium channel blockers, advanced glycation end products, soluble receptor for advanced glycation end products Introduction Although it has been established that angiotensin converting enzyme inhibitors (ACEIs) and angiotensin receptor blockers (ARBs) reduce proteinuria/albuminuria and suppress the reduction in glomerular filtration rate (GFR) in patients with diabetic nephropathy, the renoprotective effects of calcium channel blockers (CCBs) remain to be established. Kumagai et al. (2) reported that the L-type CCB, amlodipine, had very similar effects on renal function to those of ACEIs, while Peng et al. (3) demonstrated that benidipine, an inhibitor of T-type as well as L- and N-type calcium channels (1), caused an equivalent reduction in proteinuria as the ARB, valsartan, in hypertensive patients with protein excretion of 1-3 g/day. Several investigators have reported that benidipine has greater beneficial effects than amlodipine on renal function in patients with either essential hypertension (4) or chronic kidney disease (CKD) (5). These findings suggest that benidipine may have potential benefits as an antihypertensive drug with a reno-protective effect. However, only a few studies have compared the effects of benidipine and amlodipine on renal function in patients with diabetic nephropathy, including urinary albumin excretion (UAE) and urinary levels of liver-type fatty-acid binding protein (L-FABP). Advanced glycation end products (AGEs) are thought to be involved in the pathogenesis of diabetic nephropathy as a consequence of multifactorial mechanisms such as oxidative stress and overproduction of various cytokines (6). AGEs are heterogeneous sugar-derived proteins which accumulate in the glomerular basement membrane, mesangial cells, and podocytes in diabetic patients (6). Inhibition of AGE formation, blockade of the interaction between AGEs and the receptor for AGE (RAGE) and suppression of RAGE expression or its downstream pathways may therefore serve as therapeutic targets for treatment of vascular complications in diabetes (7). Matsui et al. (8) suggested that blockade of the renin angiotensin system (RAS) by ARBs may have a protective role against tubular injury in diabetes by attenuating the deleterious effects of AGEs via down-regulation of RAGE. However, the effects of CCBs on the AGE/RAGE axis in patients with diabetic nephropathy are not well known. In this study, we compared the effects of benidipine and amlodipine on renal function and the AGE/RAGE axis in patients with diabetic nephropathy with microalbuminuria. Patients and Methods Patients We enrolled 60 patients with diabetic nephropathy complicated by microalbuminuria and poorly controlled hypertension despite receiving the maximum dose of ARBs. The patients had a high systolic (>130 mmHg) and/or diastolic (>80 mmHg) blood pressure measured on 2 different days within 4 weeks of the start of the study (9). Diabetic nephropathy was diagnosed clinically as persistent microalbuminuria (20-200 g/min) in at least 2 of 3 consecutive 24-h urine samples in patients with diabetic retinopathy, but without kidney or urinary tract diseases. In patients with no signs of retinopathy, a kidney biopsy was required for the diagnosis of diabetic nephropathy (10). Exclusion criteria in the study were age younger than 20 years and older than 70 years, renal impairment (serum creatinine >1.2 mg/dL for women or >1.5 mg/dL for men), valvular heart disease, chronic lung disease, liver disease, collagen disease, recent stroke or myocardial infarction (within 1 year), or a clinical contra-indication to CCBs. Study design The patients were assigned randomly to two groups in a blinded fashion to receive either amlodipine 5 mg/day or benidipine 8 mg/day. These are the daily standard doses of both agents approved in Japan (11). Any other anti-hypertensive therapy could be added during the study in order to attain a blood pressure of < 130/80 mmHg, including alpha-blockers and diuretics, but not ACEIs, other ARBs, or other CCBs. The doses of these extra drugs were not changed during the study period. Table 1 summarizes the clinical and laboratory findings of the subjects. Treatment with the CCBs was continued for 12 months, with clinical and laboratory parameters being investigated every 3 months. The local ethical committee approved the study protocol, and written, informed consent was obtained from each patient at the start of the study. Measurements Blood pressure was measured 3 times with the patient in the sitting position, after 10 min of rest, and the average blood pressure used in the analyses. Serum creatinine, HbA1c, LDL-cholesterol, HDL-cholesterol, triglycerides, uric acid, and urinary creatinine were also measured. The estimated glomerular filtration rate (eGFR) was calculated in accordance with the Japanese Society of Nephrology CKD Practice Guidelines as; eGFR (mL/min/1.73 m2) = 194 (serum creatinine level [mg/dL])-1.094 (age [y])-0.287. The product of this equation was multiplied by a correction factor of 0.739 for women (12). Urinary L-FABP concentration was determined in duplicate using a specific enzyme immunoassay (CMIC, Tokyo, Japan) according to the instructions provided by the manufacturer (13, 14). The value was expressed as the ratio of L-FABP concentration to urinary creatinine concentration. Serum AGEs were measured by a enzyme-linked immunosorbent assay (ELISA), with one IU corresponding to 2 g of glyceraldehyde-derived AGE-bovine serum albumin standard as described previously (15, 16). Soluble RAGEs were measured using a commercially available ELISA kit (R & D System, Minneapolis, MN, USA) (17). Statistics The data were expressed as mean ± SE. Simple regression analysis was performed to assess the linear relationship between two variables. Intergroup comparisons were performed using unpaired t tests for parametric data or Mann Whitney’s U test for non-parametric data. Intragroup comparisons were assessed using a paired t test for parametric data or the Wilcoxon Rank Sum test for non-parametric data. The level of statistical significance was set at p<0.05. All calculations were performed with SPSS version 11.0 software (SPSS, Inc., Chicago, IL, USA). Results The baseline characteristics and concomitant medications including the type of ARBs were similar between the patients receiving either benidipine or amlodipine (Table 1). No adverse effects were observed in any patient during the study period and the study protocol was completed by all the patients. Prior to the start of CCB treatment, both serum AGEs (R=0.814, p<0.001) and serum soluble RAGEs (R=0.697, p<0.001) correlated with urinary L-FABP, while serum soluble RAGEs correlated with serum AGEs (R=0.887, p<0.001) (Fig. 1). In addition, serum AGEs (R=0.892, p<0.001) and serum soluble RAGEs (R=0.787, p<0.001) both correlated with UAE. Systolic and diastolic blood pressure both decreased after 12 months (p<0.001) in the benidipine (152.6±7.4/91.8±3.8 to 130.6±3.1/81.6±1.7 mmHg, p<0.001) and amlodipine (151.0±6.6/90.6±3.6 to 131.0±2.8/82.2±1.6 mmHg, p<0.001) groups. Serum creatinine and eGFR showed no significant differences during the study period in the benidipine group (creatinine, 0.763±0.082 to 0.771±0.066 mg/dL; eGFR, 74.71±8.11 to 75.12±7.40 mL/min) nor in the amlodipine group (creatinine, 0.760±0.080 to 0.796±0.058 mg/dL; eGFR, 75.72±6.04 to 73.28±7.13 mL/min). Figure 3 shows the changes in UAE and urinary L-FABP. UAE decreased significantly after 12 months in the benidipine group (124.9±24.8 to 86.2±28.4 g/min, p<0.001), whereas no significant change was observed in the amlodipine group (125.3±25.7 to 121.6±22.1 g/min, p=0.72). The UAE values after 12 months were significantly lower in the benidipine group compared to the amlodipine group (p<0.001). Urinary L-FABP levels decreased significantly after 12 months in the benidipine group (25.32±6.00 to 19.76±5.22 g/g.crea, p<0.001), whereas they remained unchanged in the amlodipine group (25.28±5.30 to 26.04±5.36 g/g.crea, p=0.82). The L-FABP levels after 12 months tended to be lower in the benidipine group compared to the amlodipine group (p=0.069). Serum AGE levels decreased significantly after 12 months in the benidipine group (12.5±2.4 to 9.6±1.6 U/mL, p<0.001), whereas they showed no difference in the amlodipine group (13.1±2.5 to 13.4±2.3 U/mL, p=0.84). The AGE levels after 12 months were lower in the benidipine group compared to the amlodipine group (p<0.001). Serum soluble RAGE levels decreased after 12 months in the benidipine group (2152.0±460.2 to 1680.6±266.6 pg/mL, p<0.001). However, this trend was not observed in the amlodipine group (2148.7±337.8 to 2120.2±312.2 pg/mL, p=0.82). Soluble RAGE levels in the benidipine group were also lower than in the amlodipine group (p<0.001) (Fig. 4). Discussion The role of CCBs on CKD has attracted considerable recent attention (18). Ichihara et al. (19) reported that the addition of the CCB, amlodipine, to ARB therapy was beneficial for vascular function and structure in hypertensive patients, with this effect occurring independent of the blood pressure-lowering effect. Kumagai et al. (2) reported that the effect of amlodipine on renal function was similar to that of the ACEI, enalapril, in patients with chronic glomerulonephritis. In animal models, the potentially protective effect of amlodipine against the loss of glomeruli in spontaneously hypertensive rats was shown to be a major additional effect of hypertensive treatment, especially when the renal lesions already existed (20). While amlodipine has only an L-type calcium channel blocking effect, benidipine lowers glomerular capillary hydraulic pressure by reducing the resistance of efferent arterioles due to its N-type and T-type calcium channel blocking effect, with a subsequent reduction in UAE (21). Therefore, benidipine is considered to have a more potent renoprotective effect than amlodipine, and therefore may be very effective for treating hypertensive patients with diabetes (1). While some investigators have reported favorable effects of benidipine on renal function in patients with hypertension or CKD (4, 5), Morikawa et al. (22) demonstrated that benidipine did not reduce proteinuria in patients with non-diabetic nephropathy. In the present study, we demonstrated that the addition of benidipine, but not of amlodipine, to an ARB ameliorated UAE and decreased urinary L-FABP levels in hypertensive patients with diabetic nephropathy. Urinary L-FABP is a novel urinary biomarker of renal tubulointerstitial function. Sasaki et al. (23) reported that urinary L-FABP levels reflected free fatty acid-induced proximal tubular stress that leads to tubulointerstitial damage. Kamijo-Ikemori et al. (24) showed that renal L-FABP ameliorated tubulointerstitial damage in diabetic mice, suggesting that L-FABP has a renoprotective effect. It was reported recently that urinary L-FABP may be a novel biomarker of chronic intrarenal ischemia in type 2 diabetes (25). In the present study, we demonstrated that urinary L-FABP level was associated with serum AGEs and soluble RAGEs in patients with diabetic nephropathy. There is evidence that AGEs accumulate in hypertrophied renal tubules of patients with diabetic nephropathy (26) and also modulate extracellular matrix turnover, with RAGEs being expressed on the surface of cultured mesangial cells. Therefore, the AGE/RAGE system may play an important role in the pathogenesis of diabetic nephropathy (27). Recently, Kerm et al. (28) reported that processing of AGE-modified proteins leads to renal tubular stress in patients with diabetic nephropathy, while Nakamura et al. (29) demonstrated that serum soluble RAGEs correlated positively with serum AGEs in patients with type 2 diabetes. Our finding of a correlation between the baseline levels of AGEs and soluble RAGEs is in accordance with these previous results. In addition, our study showed that baseline levels of serum AGEs and soluble RAGEs both correlated with urinary L-FABP. As pathophysiological crosstalk between the AGE/RAGE system and angiotensin II is considered to be involved in the progress of diabetic nephropathy, inhibition of AGE formation and/or their downstream pathway, in addition to inhibition of RAS, may be a novel therapeutic option for diabetic nephropathy (6). Targeting of RAGEs may also be a beneficial treatment strategy (30). Matsui et al. (31) showed a unique beneficial effect of telmisartan as an anti-inflammatory agent on AGE inhibition in diabetic nephropathy, with this effect being mediated by PPAR-gamma activation. In the present study, telmisartan had already been administered to several patients in both groups (amlodipine group: n=3, benidipine group: n=3). Matsui and coworkers (31) also demonstrated that irbesartan protected against tubular injury in diabetes by attenuating the deleterious effects of AGEs via down-regulation of RAGEs (8). In the present study, medication with ARBs was similar in the amlodipine and benidipine groups. Therefore, our findings appeared to be dependent on differences in the effects of amlodipine and benidipine. Matsui et al. (32) reported that nifedipine, but not amlodipine, down-regulated RAGE mRNA and subsequently reduced generation of reactive oxygen species in AGE-exposed mesangial cells. In our study, we demonstrated that 12 months of treatment with benidipine reduced the levels of serum AGE and soluble RAGEs in diabetic patients with microalbuminuria. Limitations/conclusions The present study had several limitations. First, the sample size was relatively small and therefore a large-scale, multicentered, double-blind study is required to confirm our findings. Second, whether the present results were a class effect of T-type CCBs or alternatively were specific to benidipine also remains to be determined. Third, we did not determine whether the effects were dose-dependent, as the standard doses of amlodipine and benidipine approved in Japan were used in the study (11). Fourth, we did not determine the effects of these drugs in diabetic patients with macroalbuminuria, and/or renal insufficiency. It is therefore necessary in future studies to determine whether benidipine is effective at different stages of diabetic nephropathy. In conclusion, the present study indicates that benidipine is more effective than amlodipine for ameliorating UAE, urinary L-FABP, and the AGE/RAGE system in patients with hypertensive diabetic nephropathy and microalbuminuria. Acknowledgements We thank Dr. Shingo Yamada, Central Institute, Shino-Test Corp, Sagamihara, for measuring serum HMGB1. We also thank Dr. Takeshi Sugaya, Department of Medicine, St. Marianna University School of Medicine, Kawasaki, for helpful suggestions concerning L-FABP, and Dr. Hikaru Koide, Department of Medicine, Koto Hospital, Tokyo, for helpful suggestions about the manuscript in general. We certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript. This word was supported by Grant-in-Aid for Scientific Research on Priority Areas (C) (No.21590901) from the Ministry of Education, Culture, Sports, Science and Technology, Japan. References 1. Seino H, Miyaguchi S, Yamazaki T, et al. Effect of benidipine hydrochloride, a long-acting T-type calcium channel blocker, on blood pressure and renal function in hypertensive patients with diabetes mellitus. Analysis after switching from cilnidipine to benidipine. Arzneimittelforschung 2007;57:526-31. 2. Kumagai H, Hayashi K, Kumamaru H, et al. Amlodipine is comparable to angiotensin-converting enzyme inhibitor for long-term renoprotection in hypertensive patients with renal dysfunction: a one-year, prospective, randomized study. Am J Hypertens 2000;13:980-5. 3. Peng T, Hu Z, Xia Q, et al. A comparative study of the renoprotective effects of benidipine and valsartan in primary hypertensive patients with proteinuria. Arzneimittelforschung 2009;59:647-50. 4. Ohta M, Sugawara S, Sato N, et al. Effects of benidipine, a long-acting T-type calcium channel blocker, on home blood pressure and renal function in patients with essential hypertension: a retrospective, 'real world' comparison with amlodipine. Clin Drug Investig 2009;29:739-46. 5. Abe M, Okada K, Maruyama T, et al. Comparison of the antiproteinuric effects of the calcium channel blockers benidipine and amlodipine administered in combination with angiotensin receptor blockers to hypertensive patients with stage 3-5 chronic kidney disease. Hypertens Res 2009;32:270-5. 6. Fukami K, Yamagishi S, Ueda S, et al. Role of AGEs in diabetic nephropathy. Curr Pharm Des 2008;14:946-52. 7. Yamagishi S, Nakamura K, Matsui T, et al. Agents that block advanced glycation end product (AGE)-RAGE (receptor for AGEs)-oxidative stress system: a novel therapeutic strategy for diabetic vascular complications. Expert Opin Investig Drugs 2008;17:983-96. 8. Matsui T, Yamagishi S, Takeuchi M, et al. Irbesartan inhibits advanced glycation end product (AGE)-induced proximal tubular cell injury in vitro by suppressing receptor for AGEs (RAGE) expression. Pharmacol Res 2010;61:34-9. 9. Sasaki H, Saiki A, Endo K, et al. Protective effects of efonidipine, a T- and L-type calcium channel blocker, on renal function and arterial stiffness in type 2 diabetic patients with hypertension and nephropathy. J Atheroscler Thromb 2009;16:568-75. 10. Lajer M, Tarnow L, Jorsal A, et al. Plasma concentration of asymmetric dimethylarginine (ADMA) predicts cardiovascular morbidity and mortality in type 1 diabetic patients with diabetic nephropathy. Diabetes Care 2008;31:747-52. 11. Ohishi M, Takagi T, Ito N, et al. Renal-protective effect of T- and L-type calcium channel blockers in hypertensive patients: an Amlodipine-to-Benidipine Changeover (ABC) study. Hypertens Res 2007;30:797-806. 12. Matsuo S, Imai E, Horio M, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 2009;53:982-92. 13. Nakamura T, Sugaya T, Kawagoe Y, et al. Azelnidipine reduces urinary protein excretion and urinary liver-type fatty acid binding protein in patients with hypertensive chronic kidney disease. Am J Med Sci 2007;333:321-6. 14. Tanaka T, Doi K, Maeda-Mamiya R, et al. Urinary L-type fatty acid-binding protein can reflect renal tubulointerstitial injury. Am J Pathol 2009;174:1203-11. 15. Takeuchi M, Makita Z, Bucala R. Immunological evidence that non-carboxymethyllysine advanced glycation end-products are produced from short chain sugars and dicarbonyl compounds in vivo. Mol Med 2000;6:114-25. 16. Yamagishi S, Adachi H, Nakamura K, et al. Positive association between serum levels of advanced glycation end products and the soluble form of receptor for advanced glycation end products in nondiabetic subjects. Metabolism 2006;55:1227-31. 17. Nakamura K, Yamagishi S, Adachi H, et al. Circulating advanced glycation end products (AGEs) and soluble form of receptor for AGEs (sRAGE) are independent determinants of serum monocyte chemoattractant protein-1 (MCP-1) levels in patients with type 2 diabetes. Diabetes Metab Res Rev 2008;24:109-14. 18. Gashti CN, Bakris GL. The role of calcium antagonists in chronic kidney disease. Curr Opin Nephrol Hypertens 2004;13:155-61. 19. Ichihara A, Kaneshiro Y, Sakoda M, et al. Add-on amlodipine improves arterial function and structure in hypertensive patients treated with an angiotensin receptor blocker. J Cardiovasc Pharmacol 2007;49:161-6. 20. Bezerra DG, Pires KM, Mandarim-de-Lacerda CA. Amlodipine preserves the glomerular number in spontaneously hypertensive rats. J Cell Mol Med 2005;9:966-71. 21. Uzu T, Nishimura M, Fujii T, et al. Benidipine attenuates glomerular hypertension and reduces albuminuria in patients with metabolic syndrome. Hypertens Res 2007;30:161-5. 22. Morikawa T, Okumura M, Konishi Y, et al. Effects of benidipine on glomerular hemodynamics and proteinuria in patients with nondiabetic nephropathy. Hypertens Res 2002;25:571-6. 23. Sasaki H, Kamijo-Ikemori A, Sugaya T, et al. Urinary fatty acids and liver-type fatty acid binding protein in diabetic nephropathy. Nephron Clin Pract 2009;112:c148-56. 24. Kamijo-Ikemori A, Sugaya T, Sekizuka A, et al. Amelioration of diabetic tubulointerstitial damage in liver-type fatty acid-binding protein transgenic mice. Nephrol Dial Transplant 2009;24:788-800. 25. von Eynatten M, Baumann M, Heemann U, et al. Urinary L-FABP and anaemia: distinct roles of urinary markers in type 2 diabetes. Eur J Clin Invest 2010;40:95-102. 26. Huang JS, Chuang LY, Guh JY, et al. Effects of nitric oxide and antioxidants on advanced glycation end products-induced hypertrophic growth in human renal tubular cells. Toxicol Sci 2009;111:109-19. 27. Berrou J, Tostivint I, Verrecchia F, et al. Advanced glycation end products regulate extracellular matrix protein and protease expression by human glomerular mesangial cells. Int J Mol Med 2009;23:513-20. 28. Kern EF, Erhard P, Sun W, et al. Early urinary markers of diabetic kidney disease: a nested case-control study from the Diabetes Control and Complications Trial (DCCT). Am J Kidney Dis 2010; 55:824-34. 29. Nakamura K, Yamagishi S, Adachi H, et al. Serum levels of soluble form of receptor for advanced glycation end products (sRAGE) are positively associated with circulating AGEs and soluble form of VCAM-1 in patients with type 2 diabetes. Microvasc Res 2008;76:52-6. 30. Yan SF, Ramasamy R, Schmidt AM. Receptor for AGE (RAGE) and its ligands-cast into leading roles in diabetes and the inflammatory response. J Mol Med 2009;87:235-47. 31. Matsui T, Yamagishi S, Ueda S, et al. Telmisartan, an angiotensin II type 1 receptor blocker, inhibits advanced glycation end-product (AGE)-induced monocyte chemoattractant protein-1 expression in mesangial cells through downregulation of receptor for AGEs via peroxisome proliferator-activated receptor-gamma activation. J Int Med Res 2007;35:482-9. 32. Matsui T, Yamagishi S, Takeuchi M, et al. Nifedipine, a calcium channel blocker, inhibits advanced glycation end product (AGE)-elicited mesangial cell damage by suppressing AGE receptor (RAGE) expression via peroxisome proliferator-activated receptor-gamma activation. Biochem Biophys Res Commun 2009;385:269-72. Figure legends Fig. 1. Correlation between urinary liver-type fatty acid binding protein (L-FABP) and serum advanced glycation end products (AGEs), and serum soluble receptor for AGEs (soluble RAGEs); and between serum AGEs and serum soluble RAGEs. Significant linear correlations were observed between these parameters. Fig. 2. Effect of benidipine and amlodipine on blood pressure. Both drugs had a similar blood pressure-lowering effect. Fig. 3. Changes in urinary albumin excretion (UAE) and urinary L-FABP after 12 months. UAE and urinary L-FABP decreased significantly in the benidipine group (p<0.001), whereas no difference was observed in the amlodipine group. The levels of UAE and urinary L-FABP after 12 months were significantly lower in the benidipine group than in the amlodipine group (p<0.001). Fig. 4. Changes in serum AGEs and serum soluble RAGEs after 12 months. Serum AGEs and soluble RAGEs decreased significantly in the benidipine group (p<0.001), whereas they remained unchanged in the amlodipine group. The levels of serum AGEs and soluble RAGEs after 12 months were significantly lower in the benidipine group than in the amlodipine group.