* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cardiac Amyloidosis
Remote ischemic conditioning wikipedia , lookup
Heart failure wikipedia , lookup
Coronary artery disease wikipedia , lookup
Echocardiography wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Electrocardiography wikipedia , lookup
Cardiothoracic surgery wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Cardiac surgery wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Jatene procedure wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Myocardial infarction wikipedia , lookup
Cardiac arrest wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
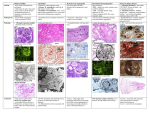
Cardiac Amyloidosis Sehrish Memon MD Case Presentation • 77 y.o M with PMHx of Diastolic CHF, moderate MVR, HLP, HTN, Mortons neuroma, Peyronie’s disease presented with progressive DOE and orthopnea • Diagnosed with Diastolic CHF about one year prior on demadex 20mg daily • Reports compliancy with medications, diet and exercise • Echo 11/13/15 • Overall left ventricular ejection fraction is estimated at 55 to 60%. • Normal global left ventricular systolic function. • (Grade 3) Severely abnormal left ventricular diastolic filling. • Moderate concentric left ventricular hypertrophy. • Severely dilated left atrium. Cardiac MRI • Referral to Cleveland Clinic • Underwent RV endomyocardial Bx: Tissue Dx of amyloidosis faintly positive for lamba light chains • BMB: Mildy Hypocellular BM (20%) with lambda predominant plasma cells (<5%) • Pro-BNP: 11477, TN-T: 0.042 • Serum Free lambda Chain: 48.4( 5.7-26.3), Free Serum Kappa Chain 39.6 (6.5 – 29.9) • CMT: Bortezomib + cyclophosphamide + Dexamethasone Definition • Deposition of extracellular misfolded proteinaceous material affecting multi-organ system • Cardiac manifestation maybe the predominant feature or found when investigating other major organ involvement • Amyloid deposition occurs in ventricles, atria, perivascularly, valves and the conduction system. • Amyloid deposits leads to increased myocardial stiffness and reduced contractility causing diastolic and progressing to systolic dysfunction B, Staining of the tissue using sulfated Alcian blue. The amyloid stains turquoise green and the myocytes stain yellow, characteristic of amyloid Rodney H. Falk Circulation. 2005;112:2047-2060 Congo Red staining of myocardial tissue from a patient with amyloid cardiomyopathy. Congo Red staining of myocardial tissue from a patient with amyloid cardiomyopathy. A, Light microscopy; B, polarized light microscopy, 400× magnification. Frederick L. Ruberg, and John L. Berk Circulation. 2012;126:1286-1300 Copyright © American Heart Association, Inc. All rights reserved. Figure 2. Myocardial biopsy in cardiac amyloidosis viewed under electron microscopy. Rodney H. Falk Circulation. 2005;112:2047-2060 Copyright © American Heart Association, Inc. All rights reserved. Type of Cardiac Amyloidosis 1) AL Amyloidosis: Acquired monoclonal light-chain 2) Senile Systemic Amyloidosis (Wild-Type ATTR) 3) Hereditary Amyloidosis (ATTR) AL Amyloidosis • estimated 2000 to 2500 new cases annually in the United States • Plasma cell clone produce a light chain prone to misfold into betapleated sheets • These light chains circulate in the bloodstream and deposit in one or more tissues • Monoclonal kappa or lambda LCs • Commonest plasma cell dyscrasia is multiple myeloma, can overlap with AL amyloidosis • Only a minority of myeloma patients develop amyloidosis, and most patients with AL amyloidosis do not have multiple myeloma Cardiac Involvement AL Amyloidosis • 50% of cases, underdiagnosed • Congestive heart failure is the presenting clinical manifestation in about half of these patients • Presence of cardiac amyloidosis is the worst prognostic factor • Once congestive heart failure occurs, the median survival is <6 months in untreated patients Pathogenesis and presentation of AL amyloidosis. Shameem Mahmood et al. Haematologica 2014;99:209-221 ©2014 by Ferrata Storti Foundation TTR Amyloidosis • Transthyretin (TTR), tetrameric protein with physiologic function of transporting thyroxine and retinolbinding protein • Synthesized by the liver • Able to aggregate into insoluble amyloid fibers depositing into variety of tissues • Familial form from mutated or variant TTR • Wild type, sporadic, nongenetic due to misaggregation of wild-type transthyretin (SSA) Diagnosis and Evaluation Electrocardiography • Low QRS voltages: <5mm in all limb leads with poor R-wave progression in chest leads (pseudoinfarction pattern) • Low ECG voltage with concentrically increased LV wall thickness • First-degree AV block (21%) • Nonspecific IVCD (16%) • Second- or third-degree AV block (3%) • Atrial fibrillation/flutter (20%) • Ventricular tachycardia (5%) • LBBB seen in 40% of wild-type ATTR, 4% AL type Echocardiography • Increased LV wall thickness ≥ 12 mm with ‘brilliant’ speckled appearance of the myocardium • Amyloid fibrils deposits are more echogenic than normal myocardium • Mean LV wall thickness > 15 mm was independently associated with worse outcome • normal or small LV cavity Early Stage Cardiac Amyloidosis Imaired relaxation with reversal of E/A ratio Late Stage Cardiac Amyloidosis Severe Restrictive Filling Pattern -E/A ratio > 2, increased E/E’ and small A wave due to atrial dysfunction -Short DT <150ms -Short IVRT <60ms • elevated LV filling pressure may lead progressively to left atrial enlargement (diameter > 23 mm/m2, area > 20 cm2 or maximal volume > 28 mL/m2), independently associated with worse outcome in AL • right atrial enlargement and dilated vena cave reflecting right ventricular (RV) filling pressure • increased interatrial septal thickness • increased RV free wall thickness (> 7 mm) with RV systolic and diastolic dysfunctions associated with worse survival • Left and right valve thickening, usually responsible for mild regurgitation The right ventricle in cardiac amyloidosis. Copyright © American Heart Association, Inc. All rights reserved. Rodney H. Falk et al. Circ Cardiovasc Imaging. 2014;7:552562 Left ventricular strain imaging in cardiac amyloidosis. • Well preserved apical straining, with significant mid and basal ventricle may help distinguish cardiac amyloid from LVH from other causes Rodney H. Falk et al. Circ Cardiovasc Imaging. 2014;7:552562 Copyright © American Heart Association, Inc. All rights reserved. Loss of atrial function in cardiac amyloidosis. Rodney H. Falk et al. Circ Cardiovasc Imaging. 2014;7:552562 Copyright © American Heart Association, Inc. All rights reserved. Depressed E’ Low Stroke Volume Figure 3. A. Typical echocardiography findings in cardiac amyloidosis: thickened and sparkled left ventricular (LV) walls, thickened interatrial septum, mitral and tricuspid valves, thickened right ventricular free wall, small pericardial effusion, normal LV c... Dania Mohty, Thibaud Damy, Pierre Cosnay, Najmeddine Echahidi, Danielle Casset-Senon, Patrice Virot, Arnaud Jaccard Cardiac amyloidosis: Updates in diagnosis and management Archives of Cardiovascular Diseases, Volume 106, Issue 10, 2013, 528–540 http://dx.doi.org/10.1016/j.acvd.2013.06.051 Definitive Dx Stanfordhealthcare.org Positive for amyloid deposits in >70% of patients with AL amyloid Figure 7. Simultaneous right and left ventricular pressure tracings in a patient with AL amyloidosis and atrial fibrillation. Rodney H. Falk Circulation. 2005;112:2047-2060 Copyright © American Heart Association, Inc. All rights reserved. Cardiac Biomarkers • BNP, NT-pro BNP and Troponins T prognostic importance in AL amyloidosis • Elevated NT-proBNP in AL amyloisis sensitive marker for cardiac involvement, >152 pmol/L associated with higher mortality rate (72% vs 7/6% per year) • High filling pressures, however local affect of amyloid deposits, BNP granules found in higher quantities in myocytes adajcent to amyloid deposits • Elevated TNI marker of poor prognosis • Combination of BNP/NT-proBNP plus troponin measurements is used to stage and risk-stratify patient and follow response to treatment in pts with AL amyloidosis at diagnosis CMR with the classic amyloid global, subendocardial late gadolinium enhancement pattern in the left ventricle with blood and mid-/epimyocardium nulling together. • Global, subendocardial late gadolinium enhancement is highly characteristic of cardiac amyloid • and correlates with prognosis. • Faster washout of gadolinium from myocardium and blood pool compared to non-amyloid control subjects Sanjay M. Banypersad et al. J Am Heart Assoc 2012;1:e000364 © 2012 Sanjay M. Banypersad et al. Cardiac Amyloidosis Biatrial enlargement, moderate concentric LVH, small pleural effusion, large bilateral pleural effusions and moderate global left ventricle (LV) and right ventricle (RV) systolic dysfunction Late gadolinium diffuse subendocardial involvement of the LV and left atrium with sparing of the RV T1 scout images demonstrate nulling of the blood pool (dark) before the myocardium (bright). This is a characteristic finding, with the myocardium having shorter T1 values than blood due to extensive extracellular space expansion and rapid myocardial gadolinium uptake. Iron Overload Cardiomyopathy Severe left ventricular (LV) enlargement with moderate global biventricular dysfunction (LV ejection fraction 32%, right ventricular ejection fraction 36%) with definite iron overload in the liver (T2* 4 msec) and borderline iron overload in the myocardium (T2* 18 msec). Cardiac Sarcoidosis -Localized areas of wall thinning and regional WMA due to inflammation on T2 weighted images –LGE may help guide the site for endomyocardial biopsy. -patchy, midwall, subepicardial, or even subendocardial, LGE with a predilection to involve the basal and mid-septal segments Radionuclide imaging • Single photon emission computed tomography (SPECT) or positron emission tomography (PET) based radiotracers • SPECT tracers: 1) I-123 labeled serum amyloid P component, SAP- Direct amyloid imaging agent -non-cardiac amyloid affected organs, calcium mediated mechanism 2) Tc-99m pyrophosphate (PYP) or Tc-99m 3,3-diphosphono-1,2propanodicarboxylic acid (DPD)- bone imaging agent 3)I-123 Metaiodobenzylguanidine(MIBG )- agent to image cardiac sympathetic innervation -Norepi analog taken up by cardiac sympathetic nerve Tc-99m pyrophosphate (PYP) SPECT in cardiac ATTR amyloidosis • Tc-99m PYP or Tc-99m DPD helpful to distinguis ALL from ATTR amyloidosis • In one study, Tc-99m DPD was able to noninvasively differentiate between AL and ATTR amyloidosis, all ATTR patients showing DPD uptake and none of the AL patients showing DPD uptake • Tc-99m PYP/DPD scan may be preferable to a CMR study for ATTRAmyloid; however a negative Tc-99m PYP/DPD scan does not rule out AL cardiac amyloid Circ Cardiovasc Imaging. 2014 May; 7(3): 552–562 PET Scans - F-18 florbetapir • PET tracers of C-11 Pittsburgh B compound and F-18 florbetapir under investigation • Direct amyloid imaging agents quantitation of amyloid burden and early cardiac involvement before overt cardiac structural changes General Treatment Principles • Volume management (diuretics/salt restriction) and arrhythmia management • Standard HF medications, B-blocker, Ace-i/ARB poorly tolerated due to hypotension from ANS dysfunction, small LV cavity and inability to augment SV in response to vasodilation • B-blocker can exacerbate arrhythmias • Digoxin bind to amyloid fibrils leading to potential Digoxin toxicity with normal circulating levels • Pacemaker often indicated due to conduction disease • Atrial fibrillation common and poorly tolerated req DCCV/anti-arrhythmics (amiodarone preferred) • Ventricular arrhythmias and SCD common • ICDS in past were discouraged due to poor prognosis, but can be effective with reasonable prognosis (>1 year) • Cardiac transplantation given irreversible nature, severe Sx’s high mortality rates Tx AL Amyloidosis • Goal achieve reduction and normalization of pathologic light chains • CMT agents: -Combination of multiple classes of antineoplastics, including alkylators (e.g., melphalan or cyclophosphamide), steroids (e.g., dexamethasone), proteasome inhibitors (e.g., bortezomib or carfilzomib), and/or immunomodulators (e.g., lenalidomide or pomalidomide) • Alternative strategy: auto-stem-cell transplant utilizing high-dose chemotherapy with an alkylating agent Pathway for a patient with suspected AL amyloidosis. Giampaolo Merlini et al. Blood 2013;121:5124-5130 ©2013 by American Society of Hematology ATTR amyloidosis • No role for CMT, not a malignant process • Diflunisal: nonsteroidal anti-inflammatory drug approved for arthritis pain stabilizes tetrameric form of transthyretin -A randomized trial demonstrated slowing of disease progression among patients with polyneuropathy due to mutant ATTR amyloidosis - nonsteroidal anti-inflammatory drugs are relatively contraindicated in HF, not likely to be a good option for ATTR cardiomyopathy. • Tafamidis: -Approved in Europe and Japan for mutant ATTR amyloidosis causing polyneuropathy -Binds thyroxine binding site to stabilize tetramer and block amyloid cascade - A Phase 3 study investigating its utility in ATTR cardiomyopathy (both wild-type ATTR and mutant ATTR) has finished enrollment, with results expected in 2018 • RNA interference approaches: Two agents that work via small-interfering RNA or RNA interference (decreasing production of transthyretin by the liver) are in Phase 3 trials for ATTR amyloidosis, including both polyneuropathy and cardiomyopathy form Prognosis • Dependent primarily on the degree of cardiac involvement and, in AL amyloidosis, on circulating light-chain levels • Prognosis for AL amyloidosis has markedly improved with life expectancy of most patients measured in years rather than months due to expanded CMT options • Prognosis in ATTR amyloidosis is generally better than in AL amyloidosis References • Falk, Rodney. Diagnosis and Management of Cardiac Amyloidosis. Contemporary Reviews in Cardiovascular Medicine. Sept, 2005. Vol 112:13. • Banypersad, Sanjay MRCP; Moon, James MRCP; Whelan, Carol MD et al. Updates in Cardiac Amyloidosis: A Review. JAHA. April 23, 2012: 10.1161 • Falk, Rodney MD, Quarta, Candida MD, Dorbala, Sharmila MD. How to Image Cardiac Amyloidosis. Circulation: Cardiovascular Imaging. 2014; 7:552-562 • Kassi, Mahwash MD, Nabi, Faisal. Role of Cardiac MRI in the Assessment of Nonischemic Cardiomyopathies. Debakeyheartcenter.com/journal. 2013 IX (3).