* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Print - Circulation
Electrocardiography wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
History of invasive and interventional cardiology wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Coronary artery disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Atrial septal defect wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
1689
Results of the Arterial Switch Operation for
Transposition of the Great Arteries With
Ventricular Septal Defect
Surgical Considerations and Midterm Follow-up Data
Roberto M. Di Donato, MD, Gil Wernovsky, MD, Edward P. Walsh, MD,
Steven D. Colan, MD, Peter Lang, MD, David L. Wessel, MD, Richard A. Jonas, MD,
John E. Mayer Jr., MD, and Aldo R. Castafneda, MD, PhD
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
Between January 1983 and December 1987, 62 patients underwent an arterial switch operation
for transposition of the great arteries with ventricular septal defect or double outlet right or left
ventricle. There were three hospital deaths (4.8%), and no deaths occurred in neonates (<1
month of age, n = 18). There were three late deaths, one due to coronary obstruction and two due
to pulmonary vascular obstructive disease. One child has been lost to follow-up. We have
prospectively evaluated the remaining 55 survivors by clinical evaluation, echocardiography,
cardiac catheterization, ambulatory electrocardiographic monitoring, and limited electrophysiologic studies. The mean length of follow-up has been 27±16 months since surgery. One child has
required reoperation for a residual ventricular septal defect; no child has undergone reoperation
for supravalvar pulmonary or aortic stenosis. Aortic regurgitation was identified in 12 children
(22%), which was mild in 11 and moderate in one. One child has asymptomatic occlusion of the
left main coronary artery, one child has a tiny right coronary artery-to-pulmonary artery fistula,
and one child has abnormal left ventricular wall motion according to follow-up angiography. No
other abnormalities of systemic (left) ventricular function have been identified at late follow-up.
In addition to the two late deaths due to pulmonary vascular obstructive disease, three children,
all of whom were repaired at more than 6 months of age, have elevated pulmonary vascular
resistance. Notable postoperative arrhythmias include complete heart block in four patients and
nonsustained supraventricular or ventricular tachycardia early after surgery in eight patients (all
resolved without medication at later follow-up). Only two patients have evidence of sinus node
dysfunction and have not required treatment. The low hospital mortality and encouraging early
follow-up data represent a significant improvement over atrial level repairs, supporting the
arterial switch operation as the procedure of choice for children who have transposition of the
great arteries with ventricular septal defect or double outlet ventricle. Because of the potential for
the development of early pulmonary vascular obstructive disease in these patients, repair is
recommended within the first 2 months of life. (Circulation 1989;80:1689-1705)
recently as 25 years ago, a child born with
transposition of the great arteries (TGA)
had only a 10% chance of surviving to 1
year of age.' The pioneering work by Rashkind and
A
s
From the Departments of Cardiology and Cardiothoracic Surgery, The Children's Hospital, and the Departments of Pediatrics
and Surgery, Harvard Medical School, Boston, Massachusetts.
Supported in part by grant HL-41786 from the National Heart,
Lung, and Blood Institute, National Institutes of Health, Bethesda,
Maryland.
Address for correspondence: Gil Wernovsky, MD, Department of Cardiology, The Children's Hospital, 300 Longwood
Avenue, Boston, MA 02115.
Received May 31, 1989; revision accepted August 11, 1989.
Miller2 for initial palliation, along with the innovative surgical repairs by Senning3 and Mustard,4 has
dramatically improved the long-term prognosis for
these children.5 Early surgical repair has been advocated to reduce long-term complications, specifically the development of pulmonary vascular
obstructive disease6'7 and the long-term effects of
See p 1912
chronic cyanosis.8 A recent report of the Mustard
operation in neonates and infants has been particularly encouraging, with no deaths in 36 consecutive
neonates with TGA and an intact ventricular septum (IVS).9
1690
Circulation Vol 80, No 6, December 1989
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
Despite significant improvements in hospital mortality, long-term follow-up has revealed disturbing
incidences of arrhythmia,10-15 tricuspid regurgitation,1416-1 8ventricular dysfunction,19-24 and sudden
death5J3"18 after atrial level repair. Many of these
late complications seem to be inherent to the intraatrial repair itself, particularly the extensive atrial
incisions and suture lines and continued reliance on
the right ventricle and tricuspid valve as the systemic ventricle and atrioventricular valve. The coexistence of a ventricular septal defect (VSD) with
TGA adds to the above problems, including a higher
surgical mortality,13,25-30 an increased risk of pulmonary vascular obstructive disease,6'3' and tricuspid regurgitation. Closure of a VSD combined with
an atrial inversion repair frequently involves manipulation of the tricuspid (systemic atrioventricular)
valve, which may be structurally abnormal,32-33 or
occasionally a ventriculotomy in what will remain
the systemic ventricle.
For these reasons, the arterial switch operation
(ASO) has been proposed as an alternative procedure for the treatment of TGA with VSD.29-30-34-39
Compared with atrial level repairs, the major potential advantages of the ASO are establishment of the
left ventricle and mitral valve as the systemic ventricle and atrioventricular valve, and the maintenance of sinus node function by avoiding extensive
atrial surgery. Although TGA with VSD was originally believed to be the only condition suitable for
a primary ASO, many centers have also begun to
successfully perform an ASO in neonates with TGA
and IVS. However, when comparing earlier results
of an ASO in patients with VSD to those with IVS,
the association of a VSD with TGA has been
considered to be an incremental risk factor for the
ASO36,40
This report details our experience with the ASO
for TGA with VSD, including double outlet right or
left ventricle at The Children's Hospital in Boston.
We have offered an ASO to all patients with TGA
since 1983 and have continued prospective followup in all patients to serially and systematically
evaluate anastomotic growth, ventricular function,
and rhythm abnormalities.
TABLE 1. Patient Population
Characteristic
Group 1
Group 2
Group 3
n
18
31
13
Age
9+8 days
4+3 mo
17+18 mo
Weight (kg)
3.7+0.6
5.2+2.3
8.2+4.4
Balloon atrial
septostomy
17 (94)
19 (61)
7 (54)
Values are mean+SD when appropriate. Values in parentheses are percentages.
Group 1, primary repair in neonates; group 2, primary repair in
infants and children; group 3, repair after prior pulmonary artery
banding.
Methods
Surgical Management
The techniques used in our institution for the
arterial switch portion of the procedure,44,45 as well
as the VSD closure,46 have been reported previously. In two patients, excision of a small segment
of the posterior commissure of the native aortic
valve was necessary because of a paracommissural
location of the coronary ostia. In 12 patients, coronary transfer involved intentional division and ligation of a small conal branch to avoid tension on the
coronary anastomosis. Four patients required revision of the coronary anastomoses because of an
inability to be weaned from cardiopulmonary bypass.
One child with origin of the left circumflex coronary
Patient Population
From January 1983 through December 1987, 62
patients underwent combined ASO and VSD closure. Fifty-six (90%) had TGA with VSD, five (8%)
had double outlet right ventricle, and one (2%) had
double outlet left ventricle. There were 43 male and
19 female patients, and they have been divided into
three groups (Table 1). In group 1, 18 patients
underwent primary repair as neonates (range, 1-26
days; mean+SD, 9+8 days); in group 2, 31 patients
had primary repair in infancy (range, 1.5-17.5
months; mean, 4+3 months); and in group 3, 13
patients had a secondary repair after pulmonary
artery banding (range, 4-72 months; mean, 17 + 18
months).
In group 1, 17 (94%) underwent balloon atrial
septostomy, and eight (44%) also received prostaglandin El infusion before surgery for persistent
cyanosis. In group 2, 19 (61%) underwent balloon
atrial septostomy, and 21 children were older than 3
months of age, including six older than 6 months of
age. Previous operations in this group included
division of a vascular ring in one patient and aortic
coarctation repair in another.
Only seven of 13 (54%) patients in group 3
underwent balloon atrial septostomy. Ten patients
had previously undergone a pulmonary artery banding combined with repair of obstructive lesions of
the aorta (aortic coarctation in nine and interrupted
aortic arch in one), whereas three patients had
pulmonary artery banding alone. One of these had
mild hypoplasia of the right ventricle and tricuspid
valve. Other previous operations in this group
included a Blalock-Hanlon atrial septectomy in two
patients and a right Blalock-Taussig shunt in one.
Additional cardiac and noncardiac diagnoses for the
three groups are reported in Table 2.
The location of the VSD is shown in Table 3 and
was similar to other reported populations having
TGA with VSD.28,41 The aorta was directly anterior
to the pulmonary artery in 10 (16%), was anterior
and rightward in 44 (71%), and anterior and slightly
leftward in three (5%); the great vessels were side
by side in five (8%). The coronary arterial branching
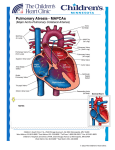
patterns and their frequency are schematically illustrated in Figure 1 and are similar to other reported
populations having TGA with VSD.42,43
Di Donato et al Arterial Switch Operation for TGA With VSD
TABLE 2. Additional Diagnoses
n
Diagnoses
Neuroblastoma
1
1
Hydronephrosis
6
Group 2
Subpulmonary stenosis
4
Dynamic
2
Atrioventricular valve tissue
3
Abnormal tricuspid valve
1
Straddling
1
Redundant tissue
1
Septal chordae
2
Left juxtaposition of the atrial appendages
1
Aortic coarctation
1
Vascular ring
Dextrocardia
1
1
Left superior vena cava
1
Bicuspid pulmonary valve
1
Neuroblastoma
1
Multiple congenital anomalies
Aortic coarctation
9
Group 3
1
Type A interrupted aortic arch
Left juxtaposition of the atrial appendages
1
1
Redundant mitral valve tissue
Group 1, primary repair in neonates; Group 2, primary repair
in infants and children; Group 3, repair after prior pulmonary
artery banding.
Group
Group 1
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
from the right coronary artery and one child with a
single right coronary artery required a second period
of cardiopulmonary bypass and revision of the right
coronary artery anastomosis to eliminate a kink in
the circumflex artery. Two children with origin of
the circumflex coronary from the right coronary
artery required revision of the left anterior descending coronary anastomosis. One patient required a
second period of cardiopulmonary bypass and circulatory arrest to close a residual VSD. In all cases,
the neopulmonary reconstruction was accomplished during core rewarming. Anterior translocation of the pulmonary artery (Lecompte maneuver47)
was performed in all but two patients (both with
side-by-side great arteries).
1691
Cardiopulmonary bypass was conducted in three
different ways depending on the date of operation
and size of the patient. In 17 patients, who were
operated upon early in our experience, the coronary
and aortic anastomoses, as well as closure of the
atrial defects and VSDs, were performed during one
or two periods of deep hypothermic circulatory
arrest totaling a mean of 83 14 minutes. In the
patients with two periods of circulatory arrest, brief
(approximately 10 minutes) periods of hypothermic
reperfusion were interposed between the two periods of circulatory arrest. In 39 patients, the circulatory arrest time was limited to the atrial defect and
VSD closure (mean, 46+22 minutes), whereas the
ASO was performed under continuous low flow (50
ml/kg/min) hypothermic perfusion. In six patients,
the entire procedure was performed under continuous low flow (50-75 ml/kg/min) cardiopulmonary
bypass with profound hypothermia, including five
patients with bicaval cannulation and a 17month-old child, without an atrial septal defect,
who underwent patch closure of the VSD through
the anterior semilunar valve. Details of cardiopulmonary bypass variables are shown in Table 4.
The type and method of cardioplegia administration varied throughout the time period of the study.
Crystalloid cardioplegia, 2.5% dextrose with 30
meq potassium chloride/l and 7 meq sodium bicarbonate/l or, more recently, Plegisol (Abbott) was
used primarily. Two patients had oxygenated blood
(100 ml per 1,000 ml of the dextrose cardioplegia)
added to the solution. In 47 patients, a single dose
(15-20 ml/kg) of cardioplegia was given after aortic
cross-clamping. In 16 patients, two doses of cardioplegia were administered; one before VSD closure and one before the completion of the coronary
and aortic anastomoses.
The VSD was exposed through the right atrium in
48, through the anterior (native aortic) semilunar
valve in six, through a combined (transatrial and
transaortic) approach in four, through the native
pulmonary valve in one, and through a right ventriculotomy in three (Table 3). The transpulmonary
valve approach was adopted in one patient with a
double outlet right ventricle and an L-malposed
±
TABLE 3. Ventricular Septal Defect Anatomic Types and Surgical Approach
Surgical approach
VSD anatomic types
Perimembranous
Malalignment
n
%
25
22
5
5
40.2
35.5
8.1
8.1
6.5
1.6
100
Muscular
Multiple
4
Atrioventricular canal type
1
Infundibular
62
Total
VSD, ventricular septal defect.
Right
atrium
22
14
5
3
Aortic
valve
3
3
Right atrium
and aortic valve
Pulmonary
Right
valve
ventricle
2
1
2
1
1
3
2
4
48
6
4
1692
Circulation Vol 80, No 6, December 1989
1
4
A
R+ L
Usual Coronary
Anatomy in TGA
40 (64.5%)
LAD
RCA.
LAD
Single Left
Coronary Artery
p
R
2
LCx
(3.2%)
LCx
RCA4
LCx
2
LAD
5
Circumflex Coronary
from the
Right Coronary Artery
RCA
12 (19.4%)
RCA
Inverted Origin
of the
Coronary Arteries
2 (3.2%)
LAD
LCx
LCx
3
6
RCA
LAD
Single Right
Coronary Artery
4 4
(8.5%)
(6.5%)RRCA
CA
L
LAD
Inverted Origin of the
Coronaryand
Artery
~~RightCircumflex
(3.2%)
~~~~~~2
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
~LCxLC
FIGURE 1. Distribution of coronary artery branching in 62 patients. TGA, transposition of the great arteries; LAD, left
anterior descending coronary artery; LCx, left circumflex coronary artery; RCA, right coronary artery.
aorta; the transventricular approach
In five patients, the sternum was not closed
primarily; the sternotomy was covered with a Silastic sheet without reapproximation of the bone edges
followed by secondary sternal closure 2-26 days
(median, 5 days) after surgery. These five patients
included three of the four who required intraoperative revision of a coronary anastomosis and the
patient who required a second period of cardiopulmonary bypass to close a residual VSD. All five
patients had significant myocardial edema, three of
whom had significant ventricular irritability during
the initial attempt to close the sternum. The mean
aortic cross-clamp time was 117 minutes for this
group of children.
was chosen in
patient with overriding tricuspid valve, in one
with right ventricular and tricuspid valve hypoplasia, and in one with the Taussig-Bing anomaly.
Small VSDs were closed by suture alone in six
neonates, and larger VSDs were closed by patch in
the remaining 56 patients (five of whom had additional small muscular defects closed primarily with
suture). An atrial septal defect was present in 55
patients and was closed primarily in 52 and with a
patch in three.
In addition to removal of the pulmonary artery
band in 13 patients, associated procedures included
right pulmonary artery plasty in four children (all
after prior pulmonary artery banding), pulmonary
("neoaortic") valvotomy in one, resection of a
subpulmonary (left ventricular outflow tract) fibrous
ridge in one, reduction arterioplasty of a massively
dilated main pulmonary artery that had been causing significant airway compression in one, division
and reattachment of straddling tricuspid valve chordae in two, excision of redundant atrioventricular
valve tissue in two (one mitral and one tricuspid),
and patch reconstruction of the right ventricular
outflow tract in one.
one
Postoperative Management
Patients were weaned from cardiopulmonary bypass
with inotropic support as dictated by heart rate, left
and right atrial pressures, and the systolic blood
pressure. In the latter half of our experience, patients
were kept sedated with a continuous Fentanyl (10
,ug/kg/min) infusion and neuromuscular blockade during the early (12-24 hours) postoperative period.
Parenteral nutrition was initiated in most cases beginning on the first postoperative morning. Inotropic and
TABLE 4. Perfusion Data
Total time
Patient
groups
n
on
cardiopulmonary
bypass
163.4+41.4
170.5-+35.1
Aortic
cross clamp
(min)
91.6+14.9
99.0+21.0
102.2+11.7
Deep hypothermic
circulatory arrest (min)
47.6+25.0
57.1+29.5
44.3+35.5
18
Group 1
31
Group 2
13
Group 3
173.2-+18.2
Total time on cardiopulmonary bypass includes circulatory arrest. Group 1, primary repair in neonates; Group 2, primary repair in
infants and children; Group 3, repair after prior pulmonary artery banding.
Di Donato et al Arterial Switch Operation for TGA With VSD
1693
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
ventilatory support were withdrawn as permitted by
clinical status. Digoxin and diuretics were routinely
instituted on the first postoperative day and were
usually continued after discharge.
heart block was present. The child died suddenly 12
hours after surgery. An autopsy revealed a residual
VSD, a restrictive left coronary anastomosis, and a
subendocardial infarction of the anterior septum.
Follow-up Protocol
Studies at hospital discharge included 12-lead
electrocardiography (ECG), 24-hour continuous
ambulatory ECG monitoring, and two-dimensional
echocardiography with Doppler, including analysis
of load-independent indexes of left ventricular
contractility.48,49 Outpatient follow-up included clinical evaluation and ECG at 6-month intervals, 24hour ambulatory electrocardiographic monitoring,
and two-dimensional echocardiography with Doppler every 1-2 years. A complete hemodynamic and
electrophysiologic evaluation was recommended
within 1 year of surgery. The detailed methods of
this protocol have been previously reported for
patients having TGA with IVS.49,50 The methods
used in our laboratory for quantifying valvar regurgitation by echocardiography with Doppler have
also been previously reported.51
The great majority of patients in this study population were referred from and continue to be
followed up at other institutions, which accounts
for variable protocol compliance and intervals of
follow-up. Only 10 of these children are primarily
cared for at The Children's Hospital in Boston,
although 10 additional patients did return for postoperative echocardiography and left ventricular function analysis, and five returned for cardiac catheterization. All of the referring cardiologists were
contacted; the clinical records, ECGs, and angiograms (through February 1989) were reviewed by
one of the authors (G.W.).
Hospital Morbidity
Among the 59 hospital survivors, the mean hospital stay was 18 ± 10 days (median, 16 days; range,
8-71 days). The duration of mechanical ventilation
and intravenous inotropic support was 5±3 days.
Eight reoperations were performed in seven patients:
two for postoperative bleeding, five for delayed
sternal closure, and one for a VSD that was believed
before surgery to be hemodynamically insignificant
and therefore was not initially repaired. This membranous VSD eventually required patch closure 37
days after the ASO because of congestive heart
failure associated with a pulmonary-to-systemic flow
ratio (Qp/Qs) of 3:1 at cardiac catheterization.
Four patients required permanent pacemaker
implantation for complete heart block. Two were
neonates who had a small perimembranous VSD
suture closed through the right atrium; one of these
neonates required intraoperative revision of the left
anterior descending coronary artery and was in
normal sinus rhythm before his second period of
cardiopulmonary bypass, suggesting that myocardial ischemia played a role in the development of
heart block. The other two patients with complete
heart block were infants who underwent VSD patch
closure; one had an anteriorly malaligned VSD, and
one had an atrioventricular canal-type VSD with a
straddling tricuspid valve. In addition, one neonate
developed complete left bundle branch block after
single-suture closure of a small VSD. Two neonates
had nonsustained supraventricular tachycardia, and
one had accelerated junctional rhythm early after
surgery while in the intensive care unit.
Five children had seizure activity in the immediate postoperative period that was controlled with
anticonvulsant medications. The mean circulatory
arrest time in these five patients was 64 minutes
(range, 41-89 minutes) compared with a mean of 50
minutes (range, 0-112 minutes) in the 54 survivors
who did not have seizures. No other neurologic
abnormalities such as abnormal movements, hemiparesis, or choreoathetosis were noted in the postoperative period.
Hospital and Discharge Studies
Two-dimensional echocardiography and Doppler. Early (days 1-3) postoperative echocardiograms were obtained in 35 patients. Ten studies
were technically inadequate for assessment of left
ventricular function, 15 patients had qualitatively
normal left ventricular function, and 10 had left
ventricular function abnormalities. One had marked
hypokinesia of the interventricular septum and diaphragmatic free wall in the postoperative period
that persisted for 12 days, gradually normalizing by
the time of hospital discharge (day 33 after surgery).
Results
Hospital Mortality
There were three hospital deaths (4.8%), all within
24 hours of surgery. The hospital mortality decreased
from 18.2% (two of 11) before June 1985 to 2.0%
(one of 51) after June 1985. There were no deaths in
the neonatal group. The two deaths early in our
experience were believed to be related to coronary
compression by a dilated left pulmonary artery.
This involved a single right coronary artery in a
1-month-old child with side-by-side great arteries in
whom the Lecompte maneuver was not performed
and the left anterior descending coronary in a
6-month-old child with the usual coronary anatomy
and an anterior and rightward aorta.
The third death occurred in a 5-month-old child
with multiple VSDs, the usual pattern of coronary
branching, and a previous coarctation repair and
pulmonary artery banding. After the ASO, the
pulmonary artery oxygen saturation was high, suggesting a significant residual VSD, and the pulmonary anastomosis was banded to facilitate withdrawal from cardiopulmonary bypass. Complete
1694
Circulation Vol 80, No 6, December 1989
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
One patient developed severe biventricular dysfunction 16 days after surgery (despite a normal echocardiogram at 12 days), which resolved rapidly during
the next 2 days with normal left ventricular function
at the time of discharge. Eight additional patients
manifested global left ventricular (n=5) or biventricular (n=3) dysfunction, which resolved by the
time of discharge in six patients.
Complete two-dimensional echocardiography with
Doppler was performed on 55 (93%) patients before
hospital discharge. All of these patients were taking
digitalis and diuretics at the time of evaluation. A
small, hemodynamically insignificant residual VSD
was detected by pulsed or color Doppler in 23
patients, and a large, minimally restrictive VSD was
imaged in one. Mild regurgitation of the neoaortic
valve was noted in 12 patients (22%) with no
instances of moderate or severe aortic regurgitation. Mild stenosis (.35 mm Hg) at the aortic
anastomosis was found in three patients and at the
pulmonary anastomosis in six, and moderate (45
mm Hg) supravalvar pulmonary stenosis was found
in one. Regurgitation of the neopulmonary valve
was mild in 14 patients and moderate in two. Mitral
regurgitation was mild in eight patients and moderate in one; tricuspid regurgitation was mild in 14 and
moderate in two.
Systolic flattening of the interventricular septum,
indicating right ventricular systolic hypertension,52
was present in 12 patients. Four patients were noted
to have hypokinesia or dyskinesia of the basilar
septum, and two had mild global dysfunction that
could not be quantitatively assessed because of left
ventricular distortion by residual right ventricular
hypertension. In 14 patients without regional dysfunction who also had normal left ventricular configuration (i.e., no systolic or diastolic septal flattening), quantitative analysis of left ventricular
performance was performed (Table 5). Fractional
shortening (FS) was normal (>28%) in 11 patients
and was below normal in three. Ventricular enddiastolic dimension, the rate-corrected velocity of
shortening (VCFc), end-systolic stress (ESS, a quantitative measure of ventricular afterload48,49,53), and
the ESS-VCFc relation (a load-independent index of
contractility48,54) were normal in all patients (Figure
2). In contrast, the ESS-FS relation (a preloaddependent index of contractility48) was subnormal in
five patients (Figure 3). This pattern of a low ESS-FS
relation compared with the ESS-VCFc relation is
found uniquely with low preload status.48,49,54 Thus,
these subjects manifested normal afterload and contractility with reduced preload.
Electrocardiography and ambulatory monitoring. Predischarge 12-lead ECGs from the 59 hospital survivors revealed normal sinus rhythm in 91 %.
One patient had an ectopic atrial escape rhythm,
and four were paced for complete heart block.
Intraventricular conduction disturbances (usually
right bundle branch block) were observed in 63%
(Table 7).
TABLE 5. Echocardiographic Measurements in Patients Evalu.
ated at Hospital Discharge
BSA
EDD
FS
VCFc
ESS
(n2)
(cm)
(%)
(circ/sec)
(g/cm2)
0.27
1.83
43.7
1.57
13
0.36
2.21
33.5
1.13
27
0.24
2.10
31.0
1.14
23
0.46
2.95
33.9
1.10
29
0.29
1.97
36.5
1.26
22
0.27
2.29
37.1
1.33
37
0.26
2.38
34.9
1.29
22
0.29
1.90
37.8
1.35
16
0.25
1.83
26.2
1.18
28
0.28
2.09
27.8
1.20
37
0.26
2.20
34.1
1.21
21
0.22
1.62
33.3
1.33
20
0.29
2.45
26.3
0.96
43
0.19
2.19
30.1
1.11
33
33.3
1.23
27
4.6
0.14
8
BSA, body surface area; EDD, end-diastolic dimension; FS,
fractional shortening; VCFc, rate-adjusted velocity of fiber shortening; ESS, end-systolic wall stress.
Mean
SD
0.28
0.06
2.14
0.32
Predischarge ambulatory electrocardiographic
recordings were available for 49 patients (Table 8).
Physiologic sinus rates were present in 86%, and
10% had some episodic sinus slowing with junctional escape rhythm. Atrial ectopy was frequently
seen, but no sustained or symptomatic supraventricular tachycardias were recorded. The incidence
of ventricular ectopy was high and included couplets and nonsustained ventricular tachycardia in
24%. The longest salvo of ventricular tachycardia
was seven beats in duration. Because of the uncertain significance of this ventricular ectopic activity
in the early postoperative period, suppressive drug
therapy was not recommended, although such
patients were followed up more closely with serial
ambulatory recordings.
Clinical Status
Late mortality. Among the 59 hospital survivors,
three late deaths have occurred. One child who had
a primary ASO and VSD closure at 26 days of age
had a large coronary artery from the right posterior
sinus that gave rise to the right coronary, the left
circumflex, and left anterior descending coronary
arteries; only a small conal branch arose from the
left anterior sinus. The right coronary anastomosis
required intraoperative revision and two periods of
cardiopulmonary bypass; placement of a Silastic
sheet was necessary. The postoperative course was
complicated by a sternal wound infection. After
what appeared to be a stable recovery period, and
after documentation of normal ventricular contractility and function by echocardiography at discharge, he was admitted 6 weeks later with the
Di Donato et al Arterial Switch Operation for TGA With VSD
A
1695
B
I.D.
1.41
0
0)
0)
1.2
-_._
0
0
IL
1.0
CD)
L-
-_
0.8
o.6
%0.10
-
0
25
50
75
Meridional ESS (gm/cm2)
100
Meridional ESS (gm/cm2)
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
FIGURE 2. Plot ofthe relation ofrate-adjusted velocity ofcircumferential fiber shortening (VCFc) (Panel A) and percent
fractional shortening (FS) (Panel B) to afterload (end-systolic wall stress, ESS) in 14 subjects at hospital discharge. The
mean population regression line (solid line) and 95% confidence intervals (dashed lines) for nornal subjects in our
laboratory are displayed. Normal-to-increased contractility (Panel A) was typical in these patients. The ESS-FS relation
(Panel B) tended to be nornal or low, which is consistent with reduced preload. In three subjects, preload reduction was
of sufficient magnitude to result in abnornal (<28%) FS.
acute onset (<48 hours) of congestive heart failure.
Two-dimensional echocardiography revealed global
depression of myocardial function, and diffuse ischemic changes were seen on the electrocardiogram.
He died within hours while awaiting cardiac catheterization. Autopsy revealed narrowing at the single
right main coronary ostium, and histologic study of
the left ventricle showed findings of nontransmural
myocardial infarction.
One child referred from another institution, who
had previously undergone pulmonary artery banding at 6 months of age and a subsequent BlalockTaussig shunt at 8 months of age, developed progressive pulmonary vascular obstructive disease.
At catheterization 2 days before the ASO and VSD
closure (age, 19 months), the mean pulmonary
artery pressure was 48 mm Hg with a calculated
pulmonary vascular resistance of 6.2 Wood's units;
immediately after surgery, the peak systolic pulmonary artery pressure was about 1/2 systemic pressure. Signs and symptoms of right heart failure
developed 3 months after surgery, and cardiac
catheterization revealed suprasystemic pulmonary
artery pressure with minimal response to oxygen.
The patient died at home 6 months after surgery.
A third child referred from another institution
had an ASO and VSD closure at 10 months of age
after an atrial septectomy and an ineffective pulmonary artery banding (systolic pulmonary artery
pressure, 82 mm Hg, pulmonary vascular resistance, 4.8 Wood's units). The ASO was complicated by complete heart block, and postoperative
peak systolic pulmonary artery pressure was equal
to systemic pressure. A permanent pacemaker
was placed before hospital discharge, and the
patient returned to his home country. Echocardiography performed 1 and 3 months after surgery
suggested right ventricular hypertension with dimin-
ished right ventricular function, presumably
because of pulmonary vascular disease. The patient
died suddenly 5 months after the ASO; the details
of his death and status of his pacemaker are
unknown; no autopsy was performed.
Clinical follow-up. One child has been lost to
follow-up out of the country. The remaining 55
survivors have been followed up for a mean of
27±16 months (range, 11-70 months) after surgery
(mean absolute age, 33+22 months). One child with
pulmonary vascular obstructive disease after primary repair at 6 months of age is mildly cyanotic
because of a right-to-left interventricular shunt. No
other patient has cardiovascular symptoms. Fortynine of 55 patients (89%) have normal (5th-95th
percentile) height and weight. Ten children continue to take digitalis, and three remain on diuretic
therapy, although none has clinical manifestations
of congestive heart failure. Two children have been
described by their referring physicians as having
moderate developmental delay, and one child continues to take anticonvulsant medication.
Although systolic murmurs at the base are a
typical finding, only two patients have murmurs
associated with a palpable thrill (grade 4); in one
patient, this is due to a subaortic membrane, and
in another, it is due to moderate supravalvar
pulmonary stenosis. Although 12 patients have
been shown to have aortic regurgitation by angiography or Doppler at later follow-up (see below),
only three patients have audible diastolic murmurs
of aortic regurgitation.
No child has required reoperation for supravalvar
pulmonary or aortic obstruction. One child required
reoperation to close a large residual VSD.
Hemodynamic Evaluation
Of the 55 known late survivors, 44 (80%) have
undergone cardiac catheterization: 15 of 17 (88%) in
Circulation Vol 80, No 6, December 1989
1696
PEAK SYSTOLIC GRADIENT
45#
40
0*
35
.
30
0)
m
25
E
.b
E 20
00
.
15
10
oh_
5
n.
U
__
.
_
:t
o
RV-PA
(distal)
--
LV-AO
*sub-aortic
membrane
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
FIGURE 3. Plot of the peak systolic ejection gradient
(mm Hg) from right ventricle (RV) to distal pulmonary
artery (PA) and left ventricle (LI) to ascending aorta
(AO) measured at cardiac catheterization. The RV-PA
gradient is a sum of the subvalvar, supravalvar, and
branch PA gradients in each patient (see teext). The open
circle represents subaortic obstruction in one patient.
group 1, 21 of 28 (75%) in group 2, and eight of 10
(80%) in group 3. One child (group 2) had only an
arterial study performed because of infrarenal
obstruction of the inferior vena cava. The catheterizations were performed at a mean of 10.6+4.7
months after surgery (mean absolute age, 17
months).
Great vessel anastomoses. The right ventricular
to distal pulmonary artery peak systolic ejection
gradient (PSEG) is shown in Figure 3. One patient
had a moderate degree (45 mm Hg PSEG) of obstruction at the suture line, whereas the remaining 43
patients had PSEGs of 35 mm Hg or less. Multiple
areas of potential obstruction were identified; one
patient (with the Taussig-Bing anomaly) had primarily subvalvar narrowing (PSEG, 27 mm Hg), one
had valvar obstruction (PSEG, 30 mm Hg), and five
had branch (four right and one bilateral) pulmonary
stenosis (>10 mm Hg PSEG). Most patients had
small (5-15 mm Hg) gradients measured at the
anastomosis.
The PSEG from the left ventricle to ascending
aorta is also shown in Figure 3. One patient had
moderate (PSEG, 42 mm Hg) subvalvar obstruction
due to a subaortic membrane, and one had moderate (PSEG, 38 mm Hg) obstruction at the aortic
suture line. The remaining 42 patients had PSEGs of
20 mm Hg or less, and 29 (66%) of these had a
PSEG of 5 mm Hg or less.
An incidental finding of aortic coarctation with a
PSEG of 15 mm Hg was found on pressure pullback measurements and angiography (Figure 4) in
one patient with no arch obstruction identified after
surgery, presumably because of late constriction of
ductal tissue. Of the eight patients studied with
preoperative arch obstruction, one had a residual
PSEG of 20 mm Hg, whereas the remaining seven
patients had PSEGs of 10 mm Hg or less.
FIGURE 4. Lateral projection of ascending aortogram in a patient 15 months after neonatal repair (age, 9 days). No
coarctation was identified before surgery. Note narrowing distal to the left subclavian artery, a 20-mm Hg peak systolic
gradient was measured at this site. (Photograph courtesy of Dr. Michael Snyder.)
Di Donato et al Arterial Switch Operation for TGA With VSD
END-DIASTOLIC PRESSURE
12
0
1697
80
20
10
0*
0*
15.
0@
60
8
E
I
E
E
10[
4:
0
0
0
Q 40
0:
mm
*00
41
20
5
..
~0
U.
an
RV
C
-.
LV
*large residual VSD
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
FIGURE 5. Plot of right (RP) and left (LV) ventricular
end-diastolic pressures measured at cardiac catheterization. The solid horizontal line represents the mean value.
VSD, ventricular septal defect.
Coronary anastomoses. The coronary anastomowell seen in all 44 children by aortic root
angiography (n=43) or left ventriculography (n =43).
One patient had complete occlusion of the left main
coronary artery; the left anterior descending and
left circumflex coronary arteries filled through collaterals from the right coronary artery. This patient
was asymptomatic and had a normal ECG, cardiac
index, and left ventricular end-diastolic pressure
(LVEDP). One patient had a tiny fistula from the
right coronary artery to the pulmonary artery without a significant left-to-right shunt. A small area of
dyskinesis in the apex of the left ventricle was seen
in one patient, who also had a normal ECG, cardiac
index, and LVEDP.
Oximetry and intracardiac shunting. The systemic oxygen saturation was 95% or more in all
patients except one child with severe pulmonary
vascular disease and a right-to-left shunt (arterial
saturation, 90%) through a small residual VSD.
Eight patients had trivial residual VSDs seen on left
ventriculography, but the Qp/Qs was less than 1.5
in all. One patient had a large residual VSD (Qp/
Qs=2.4) that was successfully closed at reoperation. One patient has a residual atrial septal defect
with QpIQs of 2.0, and another had a residual atrial
septal defect seen on the pulmonary venous phase
of the right ventriculogram with an insignificant
(Qp/Qs=1.2) shunt.
Ventricular function. The mean right ventricular
end-diastolic pressure (RVEDP) was 5±2 mm Hg,
whereas the mean LVEDP was 7+2 mm Hg (Figure
5). The patient with a large residual VSD had
markedly elevated filling pressures (RVEDP and
LVEDP, 16 mm Hg). Only three other patients had
an LVEDP greater than 10 mm Hg, one of whom
had ventricular pacing due to complete heart block
and one who had moderate supravalvar aortic
obstruction (38 mm Hg). The mean systemic carses were
0
rI
2
0
S
0
.rARiduni VSD
FIGURE 6. Plot of the pulmonary vascular resistance
(PVR) measured in Wood's units (wu) and the mean
pulmonary artery pressure (PAp) measured at cardiac
catheterization. Group I, primary repair in neonates;
group II, primary repair in infants and children; group
III, repair after prior pulmonary artery banding. The
solid horizontal lines represent the mean values for each
group; there were no significant differences detected
between groups. The open circles represent a patient with
a large residual ventricular septal defect (VSD).
diac index was determined in 41 patients (by thermodilution in six and the Fick method in 35) and
measured 4.1±+1.1 1/min/m2.
Pulmonary hypertension. The mean pulmonary
arteiy pressure and pulmonary vascular resistance
was measured in 43 patients and is shown in Figure
6. In addition to the two patients who died within 6
months of surgery because of progressive pulmonary vascular disease (both in group 3), two additional patients (one in group 2 and one in group 3)
had markedly elevated pulmonary vascular resistance. No patient who underwent repair during the
neonatal period (group 1) had an elevated pulmonary vascular resistance.
Semilunar and mitral valve regurgitation. Ascending aortograms were obtained in 43 patients. Catheter position precluded adequate evaluation of
neoaortic valve competence in eight patients (one of
whom had aortic regurgitation by clinical evaluation
and echocardiography). Of the remaining 35 patients,
eight (23%) had aortic regurgitation, including four
of eight patients in group 3 who had previous
pulmonary artery banding. The regurgitation was
trivial or mild in seven patients and moderate in
one. Left ventriculography in 43 patients revealed
mild mitral regurgitation in two, one of whom had
ventricular pacing for complete heart block.
Late Follow-up
Two-dimensional echocardiography and Doppler
and ventricular function. Noninvasive studies were
performed at The Children's Hospital in 20 patients
at a mean of 20±18 months (range, 6-73 months)
after surgery (mean absolute age, 23 months). Small
1698
Circulation Vol 80, No 6, December 1989
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
FIGURE 7. Echocardiographic
stop-frame of an apical twochamber view in a 2.2-yearold patient after neonatal (4
days) repair. An echogenic, dyskinetic segment in the basilar
portion of the interventricular
septum represents myocardial
infarction (MI), thought to be
the cause of this patient's complete heart block. LA, left
atrium; LV left ventricle.
residual VSDs were noted in two children. Mild
aortic regurgitation was detected in four patients,
all of whom had this finding at the time of hospital
discharge and at cardiac catheterization. A mild
gradient (<35 mm Hg) was present across the aortic
anastomosis in three patients. One patient had a
discrete subaortic membrane with a 50-60 mm Hg
maximum instantaneous gradient (40 mm Hg PSEG
at catheterization) that was not present at the time
of discharge. The degree of obstruction had slowly
progressed in the 2 years since surgery.
There were four instances of mild (<35 mm Hg)
and two of moderate (35 60 mm Hg) supravalvar
pulmonary stenosis. Mild pulmonary regurgitation
was found in six patients, mild tricuspid regurgitation in four, and mild mitral regurgitation in two. No
patient had systolic flattening of the IVS, suggestive
of significant right ventricular hypertension, including the two patients with moderate supravalvar
pulmonic stenosis and the four who had systolic
septal flattening at the time of discharge.
Only one of the four patients with regional abnormalities at the time of discharge had late echocardiographic data available; this patient continues to
show septal akinesis consistent with septal infaretion (Figure 7). This patient developed complete
heart block after a second period of cardiopulmonary bypass to revise the left anterior descend-
ing coronary anastomosis. Quantitative assessment
of left ventricular performance could not be obtained
in four additional patients because of poor echocardiographic windows but was obtained in the other
15 patients (Table 6). Left ventricular end-diastolic
dimension and wall thickness, FS, VCFe, and ESS
were normal in all. In addition, the ESS-VCFe and
ESS-FS relations were normal and concordant in
all, indicating normal contractility and normal preload status (Figure 8).
Late (mean, 11±10 months; range, 5-56 months
after surgery) echocardiograms were obtained at
outside institutions in 16 additional patients, including seven of the 11 patients who had not had a
hemodynamic evaluation by cardiac catheterization. A tiny residual VSD was noted in two patients
and a residual atrial defect in one. Mild aortic
regurgitation was noted in four patients, which was
present at hospital discharge in all. No patient had
significant (>35 mm Hg) supravalvar pulmonary
stenosis, although one had a supravalvar aortic
gradient of 38 mm Hg confirmed at catheterization.
Mild tricuspid regurgitation was identified in two
patients, and mild pulmonary regurgitation was
seen in another two patients.
Arrhythmia and conduction evaluation. On followup ECG (Table 7), sinus rhythm was preserved in
88% of patients. One had ectopic atrial escape, and
Di Donato et al Arterial Switch Operation for TGA With VSD
1699
TABLE 6. Echocardiographic Measurements in Patients Evaluated at Follow-up Examinations
BSA
(i2)
0.80
0.67
0.89
0.46
0.58
0.61
0.44
0.49
0.44
0.52
0.47
0.53
0.45
0.56
0.46
EDD
(cm)
4.05
3.55
2.30
2.49
3.26
2.76
2.45
3.09
2.85
2.83
2.92
2.50
2.48
2.74
2.37
EDWth
(cm)
0.69
0.58
0.49
0.59
0.58
0.60
0.55
0.61
0.58
0.62
0.61
0.50
0.54
0.68
0.54
FS
VCFc
ESS
(%)
(circ/sec)
(g/cm2)
35.3
37.2
31.4
42.6
34.4
34.4
38.8
32.0
36.8
43.8
35.6
42.0
35.9
39.8
43.0
1.05
1.15
0.94
1.30
0.98
1.18
1.12
1.02
1.07
1.12
1.01
1.22
1.05
1.11
1.27
52
44
51
23
51
31
34
48
39
18
33
33
34
27
18
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
2.84
Mean
0.56
0.58
37.5
1.11
36
0.13
0.47
3.8
SD
0.05
0.10
11
Following examination was at Children's Hospital, Boston.
BSA, body surface area; EDD, end-diastolic dimension; EDWth, end-diastolic wall thickness; FS, fractional
shortening; VCFc, rate-adjusted velocity of fiber shortening; ESS, end-systolic wall stress.
two had junctional escape rhythm. Of the patients
with postoperative complete heart block, one died,
and three had functioning ventricular pacemakers.
No progression of atrioventricular or intraventricular conduction disturbances was noted.
Follow-up ambulatory electrocardiographic
recordings (Table 8) showed evidence of sinus node
dysfunction in two asymptomatic patients who spent
large portions of the monitoring period in junctional
rhythm. Atrial and ventricular ectopy had largely
resolved. No patient received specific antiarrhythmic medication at any time during the follow-up.
Limited electrophysiologic data were collected
from 18 patients at the time of their hemodynamic
evaluation 7-21 months (mean, 10.3 months) after
operation. Corrected sinus node recovery time was
prolonged to 400 msec in one patient who had no
other evidence of sinus node dysfunction on ECG or
ambulatory recordings. Sinus node recovery time
was normal for the remaining patients. The AH
interval was normal for all. The HV interval was
prolonged to 90 msec in one patient, without other
clinical evidence of impaired atrioventricular conduction. Right ventricular apex activation time was
B
A
a
0
0
0
I,)
I._0
LL
0
..
Meridional ESS (gm/cm2)
..
--
.
.
_
__,---2%
Meridional ESS (gm/cm)
FIGURE 8. Plot of the relation of rate-adjusted velocity of circumferentialfiber shortening (VCFc) (Panel A) and percent
fractional shortening (FS) (Panel B) to afterload (end-systolic wall stress, ESS) in 15 patients at late (20+18 months)
follow-up. The mean population regression line and 95% confidence intervals for nornal subjects in our laboratory are
displayed as described in Figure 2. Normal contractility (Panel A) and FS (Panel B) were present in all patients.
1700
Circulation Vol 80, No 6, December 1989
TABLE 7. Early and Late Electrocardiographic Findings
Hospital discharge
0.4+0.3
59
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
Months after surgery (mean+SD)
Patients (n)
Basic rhythm (n)
Normal sinus rhythm
Ectopic atrial pacemaker
Junctional rhythm
Paced
AV conduction (n)
Normal
First-degree AV block
Second-degree AV block
Third-degree AV block
Ventricular conduction (n)
Normal
Complete RBBB
Left anterior hemiblock
Bifascicular block
Complete LBBB
Paced
Values in parentheses are percentages.
AV, atrioventricular; RBBB, right bundle branch block;
hemiblock; LBBB, complete left bundle branch block.
normal in all patients, including those with ECG
patterns of right bundle branch block, suggesting
only "peripheral" right ventricular conduction injury.
Discussion
The low surgical mortality rate, excellent clinical
status of the survivors, low incidence of late reoperation, and the midterm follow-up data showing
preservation of sinus rhythm and systemic ventricular function support our policy to perform an ASO
54 (91)
1 (2)
0 (0)
4
(7)
Last follow-up
20.4+ 15 .9
52
46
1
2
3
(88)
(2)
(4)
(6)
54 (91)
1 (2)
0 (0)
4 (7)
48 (92)
1 (2)
0 (0)
3 (6)
(30)
(45)
(2)
(14)
(2)
19 (37)
21 (40)
1 (2)
7 (13)
1 (2)
3 (6)
18
27
1
8
1
4
(7)
bifascicular block, complete RBBB+left anterior
for patients having TGA with VSD or double outlet
ventricle. For the purposes of this study, we have
included all patients in whom surgical closure of a
VSD was performed, regardless of preoperative
determination of VSD size, pulmonary blood flow,
or pulmonary arterial pressure. This is an operational definition; children with small restrictive VSDs
in whom no surgical attempt is made to close the
defect are considered in the group of patients having TGA with intact ventricular septum; seven such
TABLE 8. Early and Late Ambulatory Electrocardiographic Monitoring
Hospital discharge
Months after surgery (mean+SD)
Patients (n)
Basic rhythm (n)
Normal sinus rhythm
Episodic sinus bradycardia
with junctional escape
Paced
Atrial ectopy (n)
None
Atrial premature beats
Nonsustained supraventricular
tachycardia
Ventricular ectopy (n)
None
Ventricular premature beats
Couplets
Nonsustained ventricular
tachycardia
Values in parentheses are percentages.
0.4+0.4
49
Last follow-up
12.0±9.0
28
42 (86)
26 (93)
5 (10)
2 (4)
2 (7)
(0)
0
10 (20)
35 (71)
16 (57)
11 (39)
4 (8)
1 (4)
11 (22)
26 (54)
8 (16)
21 (75)
7 (25)
4 (8)
0
(0)
0
(0)
Di Donato et al Arterial Switch Operation for TGA With VSD
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
children have been previously reported.50 The closure of a VSD of any size prolongs the ASO and
adds to the potential risk of conduction system
injury; thus, all children who had ASO and VSD
closure are included in this report.
Hospital Mortality
In our initial experience with ASO and VSD
closure (from January 1983 to June 1985), hospital
mortality (18.2%) was similar to that previously
reported with both Senning and Mustard operations combined with VSD closure.1325-28 However, in the second half of this experience (from
June 1985 to December 1987), the early mortality
after the ASO has been very low (2.0%), establishing a clear superiority over the atrial level repair
for TGA with VSD.
Furthermore, unlike the experience of others,36,37,40,55 our recent results with the ASO for
TGA with VSD have been similar to the results for
the ASO for TGA with intact ventricular septum.50
Therefore, the higher incidence of associated cardiac and noncardiac anomalies seen in patients with
TGA with VSD36 may be a less significant risk
factor than previously reported.30
The absence of hospital deaths in the neonatal
group is consistent with the experience of
others38,40,56 and is very encouraging. Early repair
should decrease the incidence of pulmonary vascular disease and minimize the adverse effects of
cyanosis or congestive heart failure. Early repair
would also decrease the likelihood of spontaneous
closure of small membranous or muscular VSDs;
spontaneous VSD closure could reduce left ventricular pressure, thereby leading to a loss of adequate
myocardial mass and potentially rendering the
patient unsuitable for a primary ASO. We therefore
recommend that patients having TGA with VSD
undergo repair soon after the diagnosis is made,
generally within the first 2 months of life. If surgery
is to be delayed much beyond the immediate neonatal period, balloon atrial septostomy should be
considered to allow for better intercirculatory mixing and to "decompress" the left atrium.
Technical Considerations
In most patients, the VSD was approached
through the right atrium (75%), native aortic valve
(10%), or both (6%). During an ASO, any surgical
manipulation of the tricuspid or native aortic valve
during VSD closure is of lesser concern than in the
case of an intra-atrial operation because both
valves will be in the low-pressure, pulmonary
circulation after the ASO. On the other hand, the
transpulmonary approach should probably be
avoided to lessen the risk of damaging the future
aortic valve. The transventricular approach is a
useful alternative for VSD closure, although unnecessary in most occasions.
Coronary translocation has been possible with all
of the described branching patterns. When the
1701
circumflex
coronary
coronary artery arises from the right
artery, the site of implantation in the
neoaortic wall has been placed slightly more superiorly to avoid kinking of this vessel. The rarer
variations (single coronary ostia and forms of "inverted" origin) occurred too infrequently in this series
to allow for a formal statistical comparison of the
relative risks of the various branching patterns.
The recent use of deep hypothermic low flow (50
ml/kg/min) cardiopulmonary bypass has resulted in
shorter periods of circulatory arrest. Although
shorter periods of circulatory arrest may be beneficial to later central nervous system function, studies of neurologic sequelae after prolonged, continuous low flow cardiopulmonary bybass are lacking,
and the issue of circulatory arrest and long-term
neurologic outcome remains unresolved. Although
the five patients in this report who had postoperative seizures had moderately long periods of circulatory arrest, the wide range of circulatory arrest
times in this patient group and the relatively low
incidence of postoperative seizures prohibit a reliable assessment regarding their etiology. Finally, a
detailed evaluation of later development was not
undertaken as part of this study; however, a formal
assessment of developmental, cognitive, and neurologic sequelae of circulatory arrest and cardiopulmonary bypass is currently underway.
Hospital Morbidity
The average length of hospitalization was about
21/2 weeks, and reoperation and prolonged mechanical ventilation were the major causes of a prolonged stay in the intensive care unit. Twelve early
reoperations, most notably delayed sternal closure
and pacemaker implantation, were performed in 11
(19%) patients, which represents a higher incidence
of early reoperation compared with atrial level
repairs at our institution.28 Intraoperative revision
of a coronary anastomosis or VSD patch led to
extended periods of myocardial ischemia and cardiopulmonary bypass, which resulted in myocardial
edema, necessitating delayed sternal closure in five
patients. This was well tolerated, and in four of five
patients, the secondary closure was within 5 days of
the ASO.
Five (8.0%) patients developed complete heart
block, two of whom died (one shortly after surgery
and one 5 months after surgery). A similar incidence (8.7%) of complete heart block was found in
our institution with the Senning operation and VSD
closure,28 which appears to be somewhat higher
than in simple VSD closure.46,57,58 One welldescribed risk factor for the development of complete heart block is an inlet VSD with or without a
straddling tricuspid valve,36 which was present in
two of the children who developed complete heart
block. Another possible explanation is an abnormal
location of the bundle of His59 in children with
TGA. Finally, complete heart block may occur after
the ASO because of infarction of the basal portion
1702
Circulation Vol 80, No 6, December 1989
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
of the interventricular septum as was suggested by
the clinical course and postoperative echocardiogram in one child. Although the incidence of complete heart block may be somewhat higher, the
incidence of lower grade atrioventricular conduction abnormalities (right bundle branch block, left
anterior hemiblock, and bifascicular block) after the
ASO with VSD closure appears to be similar to that
reported for simple VSD closure.57,58,60
Ventricular dysfunction (as shown by twodimensional echocardiography) was a fairly common early finding and can be attributed to a variety
of factors, including the effects of cardioplegia and
aortic cross clamping, possible coronary insufficiency, and the effects of transfer of the systemic
arterial load to the left ventricle that had previously
supported the pulmonary circulation. The early
postoperative echocardiographic studies were not
performed on all patients, and clinical abnormalities
were often the reason for obtaining these studies.
This bias precludes an accurate assessment of the
incidence of transient early postoperative abnormalities of left ventricular function in this patient group.
Late Complications of the Arterial
Switch Operation
Aortic regurgitation is a common finding after
arterial repair36'61-63 and was detected in this series
by angiography or color Doppler examinations in a
total of 12 of 55 late survivors (22%). No patient has
been found to have the new appearance of aortic
regurgitation or progression of its severity throughout follow-up. The severity of the aortic regurgitation was mild in most patients as determined by
clinical evaluation, Doppler echocardiography, and
angiography and appears at present to be of little
hemodynamic significance. A recent report by Martin et a161 using quantitative radionuclide angiography showed similar findings. A prior pulmonary
artery banding probably plays a role in the development of aortic regurgitation62 and should be
avoided if possible in this patient group to reduce
the potential for aortic regurgitation as well as
pulmonary artery distortion. Aortic regurgitation
has also occurred after a primary ASOS5 as well,
and native pulmonary valve regurgitation has occasionally been noted before surgery.64 The ultimate
impact of aortic regurgitation after the ASO on
ventricular size and function remains unknown, and
long-term, serial follow-up will be necessary.
Coronary translocation remains the most technically challenging aspect of the ASO and may contribute significantly to perioperative mortality and
morbidity. In this series, coronary obstruction was
implicated in all three early deaths, but increased
experience with coronary transfer has reduced the
incidence of this complication. Because of the high
incidence of complete right bundle branch block or
bifascicular block after VSD closure, the ECG is of
limited help in the postoperative period for diagnosing ischemia. Hemodynamic instability may be a
marker for coronary compromise, and further investigation with echocardiography or angiography is
indicated in these cases. Furthermore, the appearance of congestive heart failure in a previously well
child after the ASO can be an indication of coronary
compromise and should be investigated and treated
promptly.
The late implications of neonatal coronary translocation remain unknown. Asymptomatic coronary
occlusion was previously documented in survivors
of the ASO for TGA with IVS50 and was seen in one
child in this series as well. The length of follow-up
and age of this patient population prevent formal
evaluation of ventricular function with stress exercise testing, and long-term follow-up and investigation is clearly necessary before final recommendations can be made. At present, we continue to
recommend follow-up cardiac catheterization and
angiography for this group of patients as well as
serial evaluations of ventricular function.
Comparison of the Arterial Switch Operation in
Patients With Either Ventricular Septal Defect or
Intact Ventricular Septum
Children having TGA with VSD or double outlet
ventricle form a heterogeneous group because of
many factors, including location and size of the
VSD and a variety of associated intracardiac and
extracardiac defects. In contrast, children having
TGA with IVS represent a much more homogeneous group of patients, and comparison of a mode
of surgical repair between groups may not be warranted. Some centers have reported that the presence of a VSD is a risk factor for the ASO;
however, we have found that hospital mortality is
similar and late supravalvar pulmonary stenosis has
been less common in patients with a VSD. This may
reflect in part the "learning curve" achieved early
in our experience with patients having TGA with
IVS. Significant late systemic ventricular dysfunction has not been identified in either group. Other
late complications such as rare sinus node dysfunction and incidences of aortic regurgitation and coronary obstruction were similar in patients with VSD
and IVS.50 Pulmonary hypertension, complete heart
block, and lower grade ventricular conduction abnormalities are more common in patients with a VSD
than with an IVS, but are unlikely to be arterial or
atrial level repair per se. Rather, the presence of a
VSD may be better considered as a risk associated
with TGA that is independent of the mode of
surgical correction. In our experience, the increase
in risk associated with a VSD is limited to the
development of pulmonary vascular disease or atrioventricular conduction abnormalities and not to
hospital mortality or late reoperation.
Comparison of Atrial With Arterial Repair
The low hospital mortality and encouraging midterm follow-up data support the notion that a primary ASO is the preferred method of repair for
Di Donato et al Arterial Switch Operation for TGA With VSD
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
children having TGA with VSD or double outlet
ventricle. Late complications related to the great
vessel and coronary anastomoses (supravalvar or
coronary obstruction and semilunar valve regurgitation) have been, for the most part, hemodynamically insignificant or very infrequent. In contrast to
atrial level repairs, resting ventricular function and
systemic atrioventricular valve competence have
been preserved during the short-term, as documented by cardiac catheterization and (in a more
limited number of patients) two-dimensional echocardiography. Complications related to VSD closure (conduction abnormalities, tricuspid or anterior semilunar valve regurgitation, and residual
defects) are likely to occur with either atrial or
arterial repair; however, the hemodynamic effects
of tricuspid regurgitation or a right ventriculotomy
are of more significance after intra-atrial repairs that
rely on the tricuspid valve and right ventricle to
function in the systemic circulation. Because the
VSD must be closed, the ASO offers the potential
for a better hemodynamic result.
Importantly, sinus node dysfunction, which is so
common after the Mustard or Senning operations,
appears to be a rare finding after ASO. Although
arrhythmias are not completely absent with the
ASO, significant arrhythmias have been infrequent
and limited to the immediate perioperative period.
Most arrhythmias after the ASO have been transient and benign.50,65,66
Thus, low operative mortality and an infrequent
incidence of significant complications at midterm
follow-up lead us to recommend the ASO for children with TGA with VSD. We recognize that a
longer duration of follow-up will be necessary before
final comparisons of the two alternative surgical
approaches may be made.
Acknowledgments
The authors greatly acknowledge the support and
cooperation of all of the referring cardiologists,
especially those in the New England Regional Infant
Cardiac Program. We also thank Dr. Thomas J.
Hougen for helping to establish the follow-up protocol. We are indebted to Ms. Emily Flynn McIntosh for her assistance with the artwork and figures.
References
1. Liebman J, Cullum L, Belloc NB: Natural history of transposition of the great arteries-Anatomy and birth and death
characteristics. Circulation 1969;40:237-262
2. Rashkind WJ, Miller WW: Transposition of the great arteries: Results of palliation by balloon atrioseptostomy in
thirty-one infants. Circulation 1968;38:453-462
3. Senning A: Surgical correction of transposition of the great
vessels. Surgery 1959;45:966-980
4. Mustard WT: Successful two-stage correction of transposition of the great vessels. Surgery 1964;55:469-472
5. Turina M, Siebenmann R, Nussbaumer P, Senning A: Longterm outlook after atrial correction of transposition of the
great arteries. J Thorac Cardiovasc Surg 1988;95:828-835
1703
6. Ferencz C: Transposition of the great vessels: Pathophysiologic considerations based upon a study of the lungs. Circulation 1966;33:232-241
7. Edwards WD, Edwards JE: Hypertensive pulmonary vascular disease in d-transposition of the great arteries. Am J
Cardiol 1978;41:921-924
8. Newburger JW, Silbert AR, Buckley LP, Fyler DC: Cognitive function and age at repair of transposition of the great
arteries in children. N Engl J Med 1984;310:1495 -1499
9. Turley K, Hanley FL, Verrier ED, Merrick SH, Evert PA:
The Mustard procedure in infants (less than 100 days of age).
J Thorac Cardiovasc Surg 1988;96:849-853
10. Hayes CJ, Gersony WM: Arrhythmias after the Mustard
operation for transposition of the great arteries: A long-term
study. JAm Coll Cardiol 1986;7:133-137
11. Flinn CJ, Wolff GS, Dick M, Campbell RM, Borkat G, Casta
A, Hordof A, Hougen TJ, Kavey RW, Kugler J, Liebman J,
Greenhouse J, Hees P: Cardiac rhythm after the Mustard
operation for complete transposition of the great arteries. N
Engl J Med 1984;310:1635-1638
12. Byrum CJ, Bove EL, Sondheimer HM, Kavey RW, Blackman MS: Hemodynamic and electrophysiologic results of
the Senning procedure for transposition of the great arteries.
Am J Cardiol 1986;58:138-142
13. Turley K, Ebert PA: Total correction of transposition of the
great arteries: Conduction disturbances in infants younger
than three months of age. J Thorac Cardiovasc Surg
1978;76:312-320
14. Warnes CA, Somerville J: Transposition of the great arteries: Late results in adolescents and adults after the Mustard
procedure. Br Heart J 1987;58:148-155
15. Vetter VL, Tanner CS, Horowitz LN: Electrophysiologic
consequences of the Mustard repair of d-transposition of the
great arteries. JAm Coll Cardiol 1987;10:1265-1273
16. Tynan M, Aberdeen E, Stark J: Tricuspid incompetence
after the Mustard operation for transposition of the great
arteries. Circulation 1972;46 (suppl I):I-111-1-115
17. Chin AJ, Sanders SP, Williams RG, Lang P, Norwood WI,
Castaneda AR: Two-dimensional echocardiographic assessment of caval and pulmonary venous pathways after the
Senning operation. Am J Cardiol 1983;52:118-126
18. Hagler DJ, Ritter DG, Mair DD, Davis GD, McGoon DC:
Clinical, angiographic, and hemodynamic assessment of late
results after Mustard operation. Circulation 1978;57:12141220
19. Graham TP Jr, Atwood GF, Boucek RJ Jr, Boerth RC,
Bender HW Jr: Abnormalities of right ventricular function
following Mustard's operation for transposition of the great
arteries. Circulation 1975;52:678-684
20. Hagler DJ, Ritter DG, Mair DD, Tajik AJ, Seward JB,
Fulton RE, Ritman EL: Right and left ventricular function
after the Mustard procedure in transposition of the great
arteries. Am J Cardiol 1979;44:276-283
21. Borow KM, Keane JF, Castaneda AR, Freed MD: Systemic
ventricular function in patients with tetralogy of Fallot,
ventricular septal defect and transposition of the great arteries repaired during infancy. Circulation 1981;64:878-885
22. Trowitzsch E, Colan SD, Sanders SP: Two-dimensional
echocardiographic estimation of right ventricular area change
and ejection fraction in infants with systemic right ventricle
(transposition of the great arteries or hypoplastic left heart
syndrome). Am J Cardiol 1985;55:1153-1157
23. Kato H, Nakano S, Matsuda H, Hirose H, Shimazaki Y,
Kawashima Y: Right ventricular myocardial function after
the atrial switch operation for transposition of the great
arteries. Am J Cardiol 1989;63:226-230
24. Musewe NN, Reisman J, Benson LN, Wilkes D, Levison H,
Freedom RM, Trusler GA, Canny GJ: Cardiopulmonary
adaptation at rest and during exercise 10 years after Mustard
atrial repair for transposition of the great arteries. Circulation 1988;77:1055-1061
25. Egloff LP, Freed MD, Dick M, Norwood WI, Castaneda
AR: Early and late results with the Mustard operation in
infancy. Ann Thorac Surg 1978;26:474 484
1704
Circulation Vol 80, No 6, December 1989
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
26. Stark J, Weller P, Leanage R, Cunningham K, De Leval M,
Macartney F, Taylor JFN: Late results of surgical treatment of transposition of the great arteries. Adv Cardiol
1980;27:254-265
27. Arciniegas E, Zia QF, Hakimi M, Perry BL, Green EW:
Results of the Mustard operation for dextro-transposition of
the great arteries. J Thorac Cardiovasc Surg 1981;81:580-587
28. Penkoske PA, Westerman GR, Marx GR, Rabinovitch M,
Freed MD, Norwood WI, Castaneda AR: Transposition of
the great arteries and ventricular septal defect: Results of the
Senning operation and closure of the ventricular septal
defect in infants. Ann Thorac Surg 1983;36:281-288
29. George BL, Laks H, Klitzner TS, Friedman WF, Williams
RG: Results of the Senning procedure in infants with simple
and complex transposition of the great arteries. Am J Cardiol 1987;59:426-430
30. Trusler GA, Castaneda AR, Rosenthal A, Blackstone EH,
Kirklin JW, and the Congenital Heart Surgeons Society: Current results of management in transposition of the great arteries, with special emphasis on patients with associated ventricular septal defect. JAm Coll Cardiol 1987;10:1061-1071
31. Mair DD, Ritter DG, Ongley PA, Helmholz HF: Hemodynamics and evaluation for surgery of patients with complete
transposition of the great arteries and ventricular septal
defect. Am J Cardiol 1971;28:632-640
32. Huhta JC, Edwards WD, Danielson GK, Feldt RH: Abnormalities of the tricuspid valve in complete transposition of
the great arteries with ventricular septal defect. J Thorac
Cardiovasc Surg 1982;83:569-576
33. Deal BJ, Chin AJ, Sanders SP, Norwood WI, Castaneda
AR: Subxiphoid two-dimensional echocardiographic identification of tricuspid valve abnormalities in transposition of
the great arteries with ventricular septal defect. Am J
Cardiol 1985;55:1146-1151
34. Jatene AD, Fontes VF, Souza LCB, Paulista PP, Abdulmassih Neto C, Sousa JEMR, Zerbini EJ: Anatomic correction
of transposition of the great arteries. J Thorac Cardiovasc
Surg 1982;83:20-26
35. Stark J: Transposition of the great arteries: Which operation? Ann Thorac Surg 1984;38:429-431
36. Quaegebeur JM, Rohmer J, Ottenkamp J, Buis T, Kirklin
JW, Blackstone EH, Brom AG: The arterial switch operation: An eight-year experience. J Thorac Cardiovasc Surg
1986;92:361-384
37. Idriss FS, Ilbawi MN, DeLeon SY, Duffy CE, Muster AJ,
Berry TE, Paul MH: Arterial switch in simple and complex
transposition of the great arteries. J Thorac Cardiovasc Surg
1988;95:29-36
38. Bove EL, Beekman RH, Snider AR, Rocchini A, Dick M,
Crowley DC, Serwer GA, Rosenthal A: Arterial repair for
transposition of the great arteries and large ventricular septal
defect in early infancy. Circulation 1988;78(suppl III):III26-111-31
39. Pacifico AD, Stewart RW, Bargeron LM Jr: Repair of
transposition of the great arteries with ventricular septal
defect by an arterial switch operation. Circulation
1983;68(suppl lI):II-49-II-55
40. Norwood WI, Dobell AR, Freed MD, Kirklin JW, Blackstone
EH, and the Congenital Heart Surgeons Society: Intermediate
results of the arterial switch repair. A 20-institution study. J
Thorac Cardiovasc Surg 1988;96:854-863
41. Kirklin JW, Barratt-Boyes BG: Complete transposition of
the great arteries, in Cardiac Surgery. New York, John
Wiley & Sons, 1986, pp 1129-1218
42. Shaher RM, Puddu GC: Coronary arterial anatomy in complete transposition of the great vessels. Am J Cardiol
1966;17:355-361
43. Gittenberger-de Groot AC, Sauer U, Oppenheimer-Dekker
A, Quaegebeur JM: Coronary arterial anatomy in transposition of the great arteries: A morphologic study. Pediatr
Cardiol 1983;4(suppl I):I-15-1-24
44. Castaneda AR, Norwood WI, Jonas RA, Colan SD, Sanders
SP, Lang P: Transposition of the great arteries and intact
45.
46.
47.
48.
49.
50.
51.
52.
53.
54.
55.
56.
57.
58.
59.
60.
61.
62.
ventricular septum: Anatomical repair in the neonate. Ann
Thorac Surg 1984;38:438-443
Mayer JE Jr, Jonas RA, Castaneda AR: Arterial switch
operation for transposition of the great arteries with intact
ventricular septum. J Cardiac Surg 1986;1:97-104
Yeager SB, Freed MD, Keane JF, Norwood WI, Castaneda
AR: Primary surgical closure of ventricular septal defect in
the first year of life: Results in 128 infants. JAm Coll Cardiol
1984;3:1269-1276
Lecompte Y, Zannini L, Hazan E, Jarreau MM, Bex JP, Tu
TV, Neveux JY: Anatomic correction of transposition of the
great arteries: New technique without use of a prosthetic
conduit. J Thorac Cardiovasc Surg 1981;82:629-631
Colan SD, Borow KM, Neumann A: Left ventricular endsystolic wall stress-velocity of fiber shortening relation: A
load-independent index of myocardial contractility. J Am
Coll Cardiol 1984;4:715-724
Colan SD, Trowitzsch E, Wernovsky G, Sholler GF, Sanders SP, Castaneda AR: Myocardial performance after arterial switch operation for transposition of the great arteries
with intact ventricular septum. Circulation 1988;78:132-141
Wernovsky G, Hougen TJ, Walsh EP, Sholler GF, Colan
SD, Sanders SP, Parness IA, Keane JF, Mayer JE Jr, Jonas
RA, Castaneda AR, Lang P: Midterm results after the
arterial switch operation for transposition of the great arteries with intact ventricular septum: Clinical, hemodynamic,
echocardiographic and electrophysiologic data. Circulation
1988;77:1333-1344
Lipshultz SE, Sanders SP, Mayer JE Jr, Colan SD, Lock JE:
Are routine preoperative cardiac catheterization and angiography necessary before repair of ostium primum atrial septal
defect. JAm Coll Cardiol 1988;11:373-378
Sholler GF, Colan SD, Sanders SP: Effect of isolated right
ventricular outflow obstruction on left ventricular function in
infants. Am J Cardiol 1988;62:778-784
Borow KM, Colan SD, Neumann A: Altered left ventricular
mechanics in patients with valvular aortic stenosis and
coarctation of the aorta: Effects on systolic performance and
late outcome. Circulation 1985;72:515-522
Colan SD, Sanders SP, Ingelfinger JR, Harmon W: Left
ventricular mechanics and contractile state in children and
young adults with end-stage renal disease: Effect of dialysis and renal transplantation. J Am Coll Cardiol
1987;10: 1085-1094
Brawn WJ, Mee RBB: Early results for anatomic correction
of transposition of the great arteries and for double-outlet
right ventricle with subpulmonary ventricular septal defect.
J Thorac Cardiovasc Surg 1988;95:230-238
Planche C, Bruniaux J, Lacour-Gayet F, Kachaner J, Binet
J-P, Sidi D, Villain E: Switch operation for transposition of
the great arteries in neonates: A study of 120 patients. J
Thorac Cardiovasc Surg 1988;96:354-363
Blake RS, Chung EE, Wesley H, Hallidie-Smith KA: Conduction defects, ventricular arrhythmias, and late death after
surgical closure of ventricular septal defect. Br Heart J
1982;47:305-315
Hobbins SM, Izukawa T, Radford DJ, Williams WG, Trusler
GA: Conduction disturbances after surgical correction of
ventricular septal defect by the atrial approach. Br Heart J
1979;41:289-293
Bharati A, Lev M: The conduction system in simple, regular
(d-), complete transposition with ventricular septal defect. J
Thorac Cardiovasc Surg 1976;72:194-201
Downing JW Jr, Kaplan S, Bove KE: Postsurgical left
anterior hemiblock and right bundle-branch block. Br Heart
J 1972;34:263-270
Martin RP, Ettedgui JA, Qureshi SA, Gibbs JL, Baker EJ,
Radley-Smith R, Maisey MN, Tynan M, Yacoub MH: A
quantitative evaluation of aortic regurgitation after anatomic
correction of transposition of the great arteries. JAm Coll
Cardiol 1988;12:1281-1284
Gibbs JL, Qureshi SA, Wilson N, Radley-Smith R, Yacoub
MH: Doppler echocardiographic comparison of haemody-
Di Donato et al Arterial Switch Operation for TGA With VSD
namic results of one- and two-stage anatomic correction of
complete transposition. Int J Cardiol 1987;18:85-92
63. Gibbs JL, Qureshi SA, Martin RP, Wilson N, Yacoub MH,
Radley-Smith R: Neonatal anatomical correction of transposition of the great arteries: Non-invasive assessment of
haemodynamic function up to four years after operation. Br
Heart J 1988;60:66-68
64. Qureshi SA, Ettedgui JA, Jones ODH: Pulmonary regurgitation in transposition of the great arteries. Br Heart J
1987;57:199-201
1705
65. Vetter VL, Tanner CS: Electrophysiologic consequences of
the arterial switch repair of d-transposition of the great
arteries. JAm Coll Cardiol 1988;12:229-237
66. Martin RP, Radley-Smith R, Yacoub MH: Arrhythmias
before and after anatomic correction of transposition of the
great arteries. JAm Coll Cardiol 1987;10:200-204
KEY WORDS * transposition of the great arteries * arterial
switch operation * ventricular septal defect * pulmonary
vascular obstructive disease
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
Results of the arterial switch operation for transposition of the great arteries with
ventricular septal defect. Surgical considerations and midterm follow-up data.
R M Di Donato, G Wernovsky, E P Walsh, S D Colan, P Lang, D L Wessel, R A Jonas, J E
Mayer, Jr and A R Castañeda
Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017
Circulation. 1989;80:1689-1705
doi: 10.1161/01.CIR.80.6.1689
Circulation is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 1989 American Heart Association, Inc. All rights reserved.
Print ISSN: 0009-7322. Online ISSN: 1524-4539
The online version of this article, along with updated information and services, is located on
the World Wide Web at:
http://circ.ahajournals.org/content/80/6/1689
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally
published in Circulation can be obtained via RightsLink, a service of the Copyright Clearance Center, not the
Editorial Office. Once the online version of the published article for which permission is being requested is
located, click Request Permissions in the middle column of the Web page under Services. Further
information about this process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Circulation is online at:
http://circ.ahajournals.org//subscriptions/