* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Elinogrel, an orally and intravenously available ADP
Clinical trial wikipedia , lookup
Psychedelic therapy wikipedia , lookup
Discovery and development of direct thrombin inhibitors wikipedia , lookup
Adherence (medicine) wikipedia , lookup
Intravenous therapy wikipedia , lookup
Drug-eluting stent wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Theralizumab wikipedia , lookup
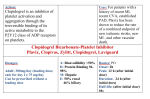
Review © Schattauer 2012 Elinogrel, an orally and intravenously available ADP-receptor antagonist How does elinogrel affect a personalized antiplatelet therapy? K. A. L. Müller; T. Geisler; M. Gawaz Medizinische Klinik III, Kardiologie und Kreislauferkrankungen, Universitätsklinikum Tübingen Keywords Schlüsselwörter Elinogrel, reversible P2Y12 ADP receptor antagonist, antiplatelet therapy Elinogrel, reversibler P2Y12-ADP-Rezeptorantagonist, antithrombozytäre Therapie Summary Zusammenfassung The antiplatelet therapy with aspirin and the ADP-receptor blocker clopidogrel is currently the standard medication after coronary intervention or after acute coronary syndrome to prevent recurrent ischemic events and reduce mortality. However, high interindividual response variability to antiplatelet treatment is described in up to 44% of treated patients. A poor response to clopidogrel is caused by multifactorial mechanisms. Individual risk assessment including platelet function testing (PFT) can help to identify high risk patients, although recent randomized trials to investigate effects of PFT-guided therapy have failed to detect an impact on prognostic outcome. Poor response to standard antiplatelet agents can be overcome by switching to alternate substances. Elinogrel is a novel competitive, reversible ADP-receptor antagonist available in oral and intravenous formulation. Additional treatment with elinogrel showed advantages over clopidogrel, including more rapid, less variable, and more complete inhibition of platelet function without significantly increased bleeding complications. This review gives an overview over the investigational drug elinogrel for use in a personalized antiplatelet approach. Die duale antithrombozytäre Therapie mit Aspirin und dem ADP-Rezeptor-Inhibitor Clopidogrel gehört zur Standardmedikation nach Koronarintervention oder akutem Koronarsyndrom, um das Auftreten kardiovaskulärer Ereignisse zu verringern. Jedoch ist eine hohe Variabilität in der Ansprechrate bei bis zu 44% aller behandelten Patienten beschrieben. Ein geringes Ansprechen auf Clopidogrel ist durch verschiedene Faktoren bedingt, weshalb eine individuelle Risikostratifizierung erfolgen sollte. Einer hohen residuellen Plättchenaktivität kann durch Anpassen der antiaggregatorischen Therapie begegnet werden. Elinogrel, ein kompetitiver, reversibler ADPRezeptor-Antagonist wurde als begleitende Medikation zu einer plättchenhemmenden Therapie mit Clopidogrel eingesetzt und untersucht. Elinogrel ist sowohl zur intravenösen als auch zur oralen Gabe verfügbar. Der zusätzliche Einsatz von Elinogrel führte zu einer schnelleren maximalen und weniger variablen Plättchenhemmung als eine ClopidogrelMonotherapie ohne signifikante Erhöhung von Blutungskomplikationen. Dieser Übersichtsartikel befasst sich mit dem Einsatz von Elinogrel in einer individuell angepassten antithrombozytären Therapie. Correspondence to: Prof. Dr. med. Meinrad Gawaz Medizinische Klinik III, Abteilung für Herz- und Kreislauferkrankungen, Eberhard-Karls-Universität Otfried-Müller-Straße 10, 72076 Tübingen E-Mail: [email protected] Elinogrel, ein oral und intravenös verfügbarer ADP-Rezeptorantagonist – In welcher Weise beeinflusst Elinogrel die personalisierte Antithrombozytentherapie? Hämostaseologie 2012; 32: 191–194 doi:10.5482/ha-1192 received: June 1, 2012; accepted: June 4, 2012; prepublished online: July 5, 2012; Personalized antiplatelet therapy after individual risk assessment Dual antiplatelet therapy with aspirin and the irreversible ADP-receptor blocker clopidogrel is currently the standard medication after coronary intervention (PCI) or acute coronary syndrome (ACS). Dual antiplatelet medication at optimal dosing and timing has lowered the risk of recurrent ischaemic events and reduced mortality significantly in randomized clinical trials (1). Hence, a high interindividual response variability to clopidogrel is described which is associated with insufficient inhibition of platelet aggregation and worse clinical outcome in patients with coronary artery disease (CAD). Mechanisms leading to poor response are multifactorial including ● drug interactions, ● polymorphisms of cytochrome P450 isoform CYP 2C19 and ● clinical factors like diabetes mellitus, renal insufficiency, age>65 years, reduced left ventricular function, and ACS (PREDICT-Score) (2). Therefore, an individual risk assessment is needed before choosing the appropriate antiplatelet therapy for each patient considering cardiovascular risk factors, bleeding risks and interventional issues. Platelet function testing can be helpful to further identify high risk patients with high ontreatment platelet reactivity. The release of new antiplatelet agents like ticagrelor and prasugrel and their recommendation over clopidogrel in the treatment of ACS in the updated guidelines by the AHA and ESC guidelines has imHämostaseologie 3/2012 Downloaded from www.haemostaseologie-online.com on 2017-06-19 | IP: 88.99.165.207 For personal or educational use only. No other uses without permission. All rights reserved. 191 192 K. A. L. Müller; T. Geisler; M. Gawaz: Elinogrel Tab. Elinogrel: clinical trials trial patients study design centers patient number treatment groups ERASE-MI STEMI randomized, double-blind, placebocontrolled pilot trial 70 ● n = 34 elinogrel ● n = 36 placebo elinogrel with escalating doses (10, 20, 40, 60 mg) as a single intravenous bolus before the diagnostic angiogram preceding primary PC and 600-mg clopidogrel loading dose, followed by a second 300-mg clopidogrel loading dose four hours after PCI versus placebo INNOVATE-PCI stable CAD undergoing non-urgent PCI randomized, double-blind, triple-dummy 652 centers in five countries 616 ● n = 408 elinogrel ● n = 208 clopidogrel elinogrel loading dose 80 or 120 mg intravenously followed by 50, 100 or 150 mg orally or clopidogrel loading dose with 300 to 600 mg and maintenance dose 75 mg/day proved patient treatment as the response variability is not as high as under clopidogrel due to different metabolic mechanisms and the effect on the ADP-receptor. Low response can also be overcome by other adjustments of the antiplatelet therapy, for example, with an additional treatment of novel substances like elinogrel, a competitive and reversible ADP-receptor antagonist that is available in an oral and intravenous formulation. Novel P2Y12 antagonists like elinogrel show advantages over a single treatment with clopidogrel, comprising more rapid, less variable, and more complete inhibition of platelet function without a significant increase of haemorrhagic complications. This review gives an overview of the investigational drug elinogrel and the options of an additional treatment with elinogrel for personalized antiplatelet therapy. Impact of switching to alternate P2Y12 receptor inhibitors in poor responders to standard antiplatelet therapy? Inadequate response to clopidogrel can be overcome by dose increase or adminis- tration of more potent P2Y12 inhibitors. The clinical impact of a platelet function guided antiplatelet approach remains unclear though. The GRAVITAS study (5429 patients, 2214 with high platelet reactivity after 600 mg clopidogrel loading dose, LD, VerifyNow to measure ADP-induced platelet aggregation) randomized patients either to a ● high-dose clopidogrel arm (600 mg LD followed by 150 mg daily maintenance dose, MD) or to a ● standard dose arm (no additional LD followed by 75 mg daily MD) for six months. Primary endpoint (cardiovascular death, non fatal myocardial infarction, or stent thrombosis) were not different among the cohorts after 30 days and six months. Despite GRAVITAS being the largest randomized trial to date of individualized antiplatelet dosing, it did not discern a significant effect of clopidogrel dose intensification. The occurrence of primary endpoints was not reduced whereas better inhibition of platelet aggregation was achieved in the high dose group (3). Another option to overcome poor response to antiplatelet therapy with clopidogrel is an additional medication with novel drugs like the third generation P2Y12 receptor antagonist elinogrel. Elinogrel, mode of action Elinogrel, a quinazoline-2,4-dione, is a potent, reversible, ADP receptor antagonist that is available in an oral and intravenous formulation (4). Elinogrel has a plasma half-life of approximately 12 hours. Its direct mode of action does not require metabolic activation or conversion into an active drug leading to reduced variability in drug response compared to clopidogrel. Polymorphisms of genes codifying hepatic cytochrome P450 isoenzymes do not seem to play a role in the elinogrel response rate (5–8). The compound is cleared to a similar extent through the kidney and the liver. Elinogrel is a reversible and competitive inhibitor of the P2Y12 receptor. This results in a direct dose-action relationship with fast on- and offset of action, thus being advantageous in bleeding situations when fast recovery of platelet function is desirable (9). Maximum platelet inhibition is achieved within 15 minutes of intravenous administration resulting in more rapid platelet inhibition effects than any other oral antiplatelet drugs. This approach is of potential clinical benefit in the setting of primary/urgent PCI or in ACS. For maintainance therapy the oral formulation was developed allowing for witching to oral medication after PCI using the same compound an thus avoiding drug-drug interactions and rebound phenomenon (10). Elinogrel has been evaluated for its effects as adjunc- Hämostaseologie 3/2012 © Schattauer 2012 Downloaded from www.haemostaseologie-online.com on 2017-06-19 | IP: 88.99.165.207 For personal or educational use only. No other uses without permission. All rights reserved. K. A. L. Müller; T. Geisler; M. Gawaz: Elinogrel outcome measures results primary percentage ST-segment resolution before first device activation during primary PCI corrected TIMI frame count before PCI percentage ST-segment resolution 30 minutes after completion of the PCI procedure primary no differences in serious adverse events TIMI and GUSTO major and minor bleeding intracranial haemorrhage through 30 days safety incidence of bleeding events infrequent and similar in elinogrel arm vs placebo troponin elevation, death, MI, stroke, GP IIb/IIIa bailout, stent thrombosis primary no significant differences for the primary end points, no deaths, strokes, or stent thromboses at 24 h/discharge TIMI major or minor bleeding clinically relevant bleeding safety no significant differences with respect to TIMI major or minor bleeding ● ● ● safety ● ● primary ● ● ● ● safety ● ● tive therapy in phase-2 clinical trials including moderate to high risk patients for whom a short onset of platelet inhibition was required. Clinical trials Elinogrel has been tested in two phase 2 studies (씰Tab.) in patients with STelevation myocardial infarction (STEMI) and in patients with stable CAD undergoing PCI. The ERASE MI study was designed as randomized, double blind, placebo controlled, dose escalating safety trial that assessed the effects of additional intravenous elinogrel bolus administration in a total of 70 patients with STEMI. Patients with STEMI were randomized to several doses of either elinogrel (n = 34) or placebo (n = 36). Elinogrel was given with escalating doses (10, 20, 40, and 60 mg) as a single intravenous bolus before the diagnostic angiography before PCI in subjects who received concomitant therapy with 600 mg clopidogrel LD, followed by a second 300 mg clopidogrel LD four hours after PCI. The primary safety endpoints of the study were TIMI major and minor in hospital bleedings, Global Strategies to Open Occluded Coronary Arteries (GUSTO) severe and moderate in-hospital bleedings and intracerebral haemorrhage within 30 days. The safety endpoints occurred in similar frequency between the placebo arm and across the different elinogrel dosing arms. No major bleeding events and five minor bleeding events were documented within the elinogrel group. The incidence of bleeding events was similar between all tested doses of elinogrel and the placebo group. No differences in serious adverse events, laboratory values, or ST resolution were demonstrated between the elinogrel and placebo arm. All doses were well-tolerated. Limitations were the small patient number of this pilot study. The trial was prematurely terminated for administrative reasons (6). The INNOVATE-PCI study was a multicenter, randomized, double-blind, tripledummy, active-controlled phase 2b study of intravenously administered elinogrel followed by an oral treatment with elinogrel in patients with CAD undergoing elective non-urgent PCI. 616 patients were assigned to receive either clopidogrel 300 or 600 mg followed by 75mg daily or elinogrel 80 or 120 mg intravenous followed by 50 mg, 100 mg or 150 mg of oral elinogrel twice daily. Compared to clopidogrel, patients in the elinogrel arm achieved a more rapid and potent platelet inhibition ex vivo with a similar bleeding rate. But there were no significant differences in the occurrence of ischemic events between the clopidogrel and elinogrel arms at 24 hours and 120 days and no significant differences in troponin elevation either. Although not significant, treatment with elinogrel was associated with higher rates of bleeding at the vascular access site requiring medical intervention as well as higher rates of serious adverse events and severe dyspnea. Elevated liver enzymes (greater than three times the upper limit of normal) occurred in 1% of the clopidogrel group and in 4.0% and 4.8% of the elinogrel 100 mg and 150 mg twice daily arms, respectively. Most cases occurred within the first 60 days, none involved serious hepatotoxicity, and all resolved even though treatment was continued (7, 8). The data show that elinogrel might provide additional platelet inhibition on top of standard dual antiplatelet therapy independent from CYP2C19 polymorphism (5). However, larger studies are needed to prove the superiority of this substance in patients with loss-of-function genotypes and to further prove the advantages of the two formulations (intravenous and oral) available for transition from acute to subacute and long-term therapy. Thus, elinogrel might represent a valuable alternative in patients in whom sufficient oral drug absorption cannot be safeguarded. However, issues concerning pharmacodynamic and -kinetic response, mode of action during transition phase from intravenous to oral solutions, drug monitoring and dosing have to © Schattauer 2012 Hämostaseologie 3/2012 Downloaded from www.haemostaseologie-online.com on 2017-06-19 | IP: 88.99.165.207 For personal or educational use only. No other uses without permission. All rights reserved. 193 194 K. A. L. Müller; T. Geisler; M. Gawaz: Elinogrel be further resolved and need to be investigated in clinical trials. The large double-blind placebocontrolled phase III trial in patients with prior history of myocardial infarction and chronic CAD was planned due to elinogrel's encouraging results in the phase II trials. However, this study was currently suspended as the production of elinogrel was preliminary terminated by the manufacturer in January 2012. Conclusion The major advantage for elinogrel is its availability as two formulations (intravenous and oral form), its fast onset and higher maximum platelet inhibition within 15 minutes of the intravenous administration. Clopidogrel exhibits a highly variable response profile and is ineffective in a relevant number of patients. In contrast, elinogrel has a lower variability and a favourable pharmacodynamic and -kinetic profile. Both, intravenous and oral elinogrel resulted in faster and more complete platelet inhibition than clopidogrel during acute and long-term therapy. Optimal timing and dosing of this novel compound warrants further clinical investigations. Recently, the manufacturer terminated the production of elinogrel in January 2012. 6. Conflict of interest The authors declare, that there are no conflicts of interest. References 1. King SB 3rd, Smith SC Jr, Hirshfeld JW Jr et al. 2007 focused update of the ACC/ AHA/SCAI 2005 guideline update for percutaneous coronary intervention: a report if the American College of Cardiology/American Heart Association Task Force on Practice guidelines. J Am Coll Cardiol 2008; 51: 172–209. 2. Geisler T, Grass D, Bigalke B et al. The Residual Platelet Aggregation after Deployment of Intracoronary Stent (PREDICT) score. J Thromb Haemost 2008; 6: 54–61. 3. Price MJ, Berger PB, Teirstein PS et al. GRAVITAS Investigators. Standard- vs high-dose clopidogrel based on platelet function testing after percutaneous coronary intervention: the GRAVITAS randomized trial. JAMA 2011; 305: 1097–1105. 4. Gretler DD, Conley PB, Andre P et al. “First in human” experience with PRT060128, a new directacting, reversible, P2Y12 inhibitor for IV and oral use. J Am Coll Cardiol 2007; 9(Suppl 2): 326A. 5. Gurbel PA, Bliden KP, Antonino MJ et al. The effect of elinogrel on high platelet reactivity during dual antiplatelet therapy and the relation to CYP2C19*2 7. 8. 9. 10. genotype: first experience in patients. J Thromb Haemost 2010; 8: 43–53. Berger JS, Roe MT, Gibson CM et al. Safety and feasibility of adjunctive antiplatelet therapy with intravenous elinogrel, a directacting and reversible P2Y12 ADP-receptor antagonist, before primary percutaneous intervention in patients with ST-elevation myocardial infarction: the Early Rapid ReversAl of platelet thromboSis with intravenous Elinogrel before PCI to optimize reperfusion in acute Myocardial Infarction (ERASE MI) pilot trial. Am Heart J 2009; 158: 998–1004.e1. Leonardi S, Rao SV, Harrington RA et al. Rationale and design of the randomized, double-blind trial testing INtraveNous and Oral administration of elinogrel, a selective and reversible P2Y(12)-receptor inhibitor, versus clopidogrel to eVAluate Tolerability and Efficacy in nonurgent Percutaneous Coronary Interventions patients (INNOVATE-PCI). Am Heart J 2010; 160: 65–72. Rao S. A randomized, double-blind, active controlled trial to evaluate intravenous and oral PRT060128 (elinogrel), a selective and reversible P2Y12 receptor inhibitor, vs. clopidogrel, as a novel antiplatelet therapy in patients undergoing non-urgent percutaneous coronary interventions (INNOVATE-PCI). ESC Congress, August 28 – September 1, 2010 in Stockholm, Sweden. Sabatine MS. Novel antiplatelet strategies in acute coronary syndromes. Cleve Clin J Med 2009; 76 (suppl 1): S8–S15. Steinhubl SR, Oh JJ, Oestreich JH, et al. Transitioning patients from cangrelor to clopidogrel: pharmacodynamic evidence of a competitive effect. Thromb Res 2008; 121: 527–534. Hämostaseologie 3/2012 © Schattauer 2012 Downloaded from www.haemostaseologie-online.com on 2017-06-19 | IP: 88.99.165.207 For personal or educational use only. No other uses without permission. All rights reserved.