* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Atrial fibrillation
Saturated fat and cardiovascular disease wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Rheumatic fever wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Heart failure wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Coronary artery disease wikipedia , lookup
Cardiac surgery wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
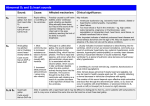
Jatene procedure wikipedia , lookup
Myocardial infarction wikipedia , lookup
Electrocardiography wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Welcome to the Medical Risk Webinar: Cardiology 4 October 2013 1 The heart (beat) The primary function of the heart is to supply blood and nutrients to the body This is accomplished by regular beating [contraction] of the heart Each heart beat is controlled by electrical impulses travelling through the heart at regular intervals 2 Interior of heart • • • • • The heart consists of 4 cavities filled with blood Right & left atria (RA/LA) Right & left ventricles (RV/LV) Atria form curved top - apex Ventricles meet at bottom to form pointed base • Atria & ventricles separated by valves • Left ventricle largest Systemic & pulmonary circulation The human heart is placed in the middle of a circle shaped like the figure ‘8’ It is structurally and functionally compartmentalised to create a double pump The left half pumps oxygenated blood to the general circulation -the systemic circulation The right half pumps deoxygenated blood to the lungs - the pulmonary circulation Conducting system Conduction pathways & the heartbeat • The rhythmic contraction of the heart is called the heart beat • The impulse to contract is generated intrinsically in specialised tissue in the wall of the right atrium (SA node) and modified when necessary extrinsically by the autonomic nervous system (particularly the vagus nerve) Anatomy – conducting system Electrical impulses from the conducting system cause the heart to beat - contract The electrical signal begins at sinoatrial [SA] node and causes the atria to contract SA node = ‘pacemaker’ The signal then passes through Atrio-ventricular [AV] node which checks the signal and sends it through the muscle fibres of the ventricles, causing them to contract Arrhythmias A heart beating regularly, albeit varying with breathing, at 60-100 (120 USA) bmp is said arbitrarily to be in normal sinus rhythm - any variation from this is, by definition, is an arrhythmia determining an arrhythmia usually requires an electrocardiogram 7 Arrhythmias • The most common arrhythmia is an extrasystole • A few people will suffer from recurrent arrhythmias but it is difficult to obtain any precise figures about prevalence as many arrhythmias are asymptomatic and go unreported • The range of arrhythmias varies from innocent extrasystoles to immediate life-threatening conditions such as asystole or ventricular fibrillation • Arrhythmias may be present in the absence of cardiac disease, but are more commonly associated with structural heart disease or external provoking factors • Transient arrhythmias, such as extrasystoles, are very common and do not usually indicate heart disease 8 The heartbeat A heartbeat is a two-part pumping action that takes about a second. Part 1 As blood collects in the right and left atria, the SA node sends out an electrical signal that causes the atria to contract. This contraction pushes blood through the tricuspid and mitral valves into the resting right and left ventricles. This is the longer part of the two-part pumping phase and is called diastole 9 The heartbeat Part 2 of the pumping phase begins when the ventricles are full of blood. The electrical signals from the SA node travel through the AV node along a pathway of cells to the ventricles causing them to contract. This is called systole. The pulmonary and aortic valves are pushed open. Blood is squeezed from the ventricles to the lungs, via the pulmonary artery and to the coronary arteries and other parts of the body through the aorta. 10 Diagramtic representation Atrial depolarisation Atria SA node AV node Ventricles Ventricular depolarisation His-Purkinge system 11 The Sinus (SA) Node The onset of depolarisation in the healthy heart begins within a focus of pacemaker cells found at the upper right border of the heart. These cells which give the initial activation are collectively known as the sinus (or sinoatrial) node Healthy rhythms are classified by heart rate as follows: Sinus rhythm — a heart rate between 50 and 100 (120) bpm. Sinus tachycardia — a heart rate over 120 bpm. Sinus bradycardia — a heart rate below 50 bpm. 12 Sinus Rhythm Sinus rhythm occurs when the sinus node depolarises spontaneously, and the consequent wave of depolarisation follows the natural pathways through the heart. When this electrical impulse is released from the SA node it causes the atria to contract The following ECG trace shows sinus rhythm at a rate of 77 bpm. Each QRS complex (shaded) is preceded by a P wave (arrowed) of regular shape 13 Reminder of ECG nomenclature P wave = activation (depolarization) of atria. QRS complex = depolarization of ventricles, T wave = ventricular repolarisation PR interval = time interval between onset of atrial depolarization and onset of ventricular depolarization QT interval = time interval between onset of ventricular depolarization and end of ventricular repolarisation R-R interval = time interval between 2 QRS complexes 14 The Atrioventricular (AV) Node The atrioventricular node introduces a delay in conduction which allows atrial contraction to fill the relaxed ventricles before ventricular contraction pushes blood around the body It also acts as a gate to prevent the ventricles from contracting too rapidly in response to atrial arrhythmias 15 Abnormal rhythms • Abnormal heart rhythms (arrhythmias) result from disorders of the normal conducting system They fall into two general types: • excessively slow heart rates, known as bradyarrhythmias or bradycardias, and • excessively fast [rapid] heart rates, known as tachyarrhythmias or tachycardias 16 Arrhythmias Fast – tachycardias Slow - bradycardiaas Classified where they begin • • Supraventricular [atria] • • • SVT AF etc Ventricular [ventricles] • • • Ventricular ectopics Ventricular tachycardias VF 17 Atrioventricular node & heart block Atrioventricular block describes a partial or total interruption of the conduction of electrical impulses from the atria to the ventricles 18 Atrioventricular block AV block is classified as follows: First degree — all heart beats are conducted from the atria to the ventricles. The conduction, however, is delayed Second degree — some, but not all, heart beats are conducted from the atria to the ventricles Third degree — no heart beats are conducted from the atria to the ventricles 19 Supraventricular tachycardia [SVT] • The atrial arrhythmias vary considerably in their rate and regularity, their clinical manifestations and the setting in which they occur. • SVT is a common clinical condition • The pulse has a regular, rapid rhythm and occurs in people of all age groups • SVT is a general term that describes tachycardias arising from within the atria or the atrioventricular node • It is the preferred term as the exact cause of the tachycardia is not always obvious from reviewing the ECG 20 Atrial fibrillation • Atrial fibrillation (AF) is a common arrhythmia • It is a significant public health problem affecting almost 5% of the population in people over 70 years of age • The prevalence of AF increases with advancing age • Data from the Framingham heart study show that AF is associated with a 1.5- to 2.0 - fold higher risk of death, because of a 5 fold increase in thrombo-embolic stroke • About 1/3 of people with AF have no symptoms • However, many experience a wide variety of symptoms, including palpitations, dyspnoea, fatigue, dizziness and angina 21 Types of Atrial Fibrillation Paroxysmal AF recurrent fibrillation that terminates spontaneously within 7 days Persistent AF lasts longer than 7 days or doesn’t stop without treatment Permanent (longstanding) AF persisting for more than a year, and possibly Acute-onset AF sudden onset (NICE 2006) 22 Aetiology of AF Known risk factors include: • male sex, • valvular heart disease (rheumatic valvular disease), • congestive heart failure, • hypertension, and • diabetes • hyperthyroidism Additional risk factors, such as – advanced age – prior history of stroke – diabetes, and – hypertension, place patients with pre-existing AF at even higher risk for further co-morbidities such as stroke 23 Atrial fibrillation Atrial fibrillation is usually due to constant conduction within the atria caused by multiple circuits. Certain parts of the atria are depolarising whilst other parts are repolarising. This causes a loss of atrial contraction due to the ineffective quiver of the muscle P waves are absent from the ECG and the baseline consists of irregular waveforms that continuously change in shape, duration, amplitude, and direction. The resulting ventricular response (seen as QRS complexes) is completely irregular 24 Atrial fibrillation In this ECG tracing the QRS complexes (arrowed) form an irregular rhythm with an average rate of 78 bpm. The ECG baseline (shaded) shows Irregular waveforms Patients are categorised clinically based on whether their atrial fibrillation is paroxysmal (self-terminating), persistent (can be converted to sinus rhythm), or permanent (unable to convert or maintain sinus rhythm) 25 Atrial fibrillation Investigations • A thorough history, physical examination, and an ECG are key to making an accurate diagnosis Blood tests include: • A thyroid function study to exclude hyperthyroidism. • Blood count. • Kidney and liver function • Digoxin level if taken Other tests include a chest X-ray, echocardiogram and 24 rhythm tape and where chest pain is a symptom catheter studies [coronary angiogram] 26 Atrial fibrillation Treatment • Generally the initial aim of treatment is to control the rhythm, however • In some patients with longstanding disease the focus is on rate control – these are usually patients with permanent AF (BMJ Sept 2013) • Two randomised controlled trials have demonstrated that a strategy aimed at restoring (and maintaining) sinus rhythm (rather than rate) neither improves the survival rate nor reduces the risk of stroke 27 Treatment of AF • Rhythm control – Flecanide and Amiodarone are used but in many patients (43-67% meta-analysis) they are not effective and, have significant side effects • Rate control – Beta-blockers and calcium channel blockers are the drugs of choice for rate control. They are effective at rest and with exertion – Digoxin can be used in the acute setting but does little to control the ventricular rate in active patients • Anticoagulation – AF is recognized as a powerful risk factor for stroke – One of the most important concerns in treating patients is the need for anticoagulation – Effective anticoagulation in patients with AF reduces the risk of stroke 3-fold 28 Treatment of AF Cardioversion • Pharmacological – in the absence of structural heart disease, a drug such as flecainide or propafenone is the drug of choice – in the presence of structural heart disease, amiodarone should be the drug of choice • Electrical – External and internal Catheter ablation – Suitable for patients with no underlying structural or valvular disease (about 2% patients with AF under 60 years) and paroxysmal disease (BMJ Sept 2013) 29 Atrial fibrillation Elective conversion to sinus rhythm • The longer patients are in AF, the more likely they are to develop atrial thrombus • In general, if the arrhythmia is present for less than 48 hours, cardioversion can be accomplished safely without further need for anticoagulation • In patients with AF longer than 48 hours in duration or of unknown duration, cardioversion is not recommended until sufficient anticoagulation is achieved • Because embolic events can occur following cardioversion as atrial mechanical function returns, continued anticoagulation for an additional 4-6 weeks is usually required • Pacing devices are available to prevent AF from recurring in susceptible individuals 30 AF Atrial fibrillation carries a particularly poor prognosis if associated with: • Mitral valve disease • Enlargement of the left atrium • Hypertension • Old age • Diabetes • History of embolism 31 Ventricular arrhythmias The term ventricular arrhythmia refers to any cardiac rhythm in which both the pacemaker site and conduction path are confined to the ventricles Arrhythmias arising from the ventricles are less common than SVTs and are more likely to be found in people with heart disease Conduction irregularities that bypass the atrioventricular node will cause the ventricles to be stimulated early and not through the standard pathways This is referred to as ventricular pre-excitation 32 Ventricular arrhythmias Ventricular ectopic beats • The most common type of ventricular ectopic beat is premature, causing ventricular contraction before the underlying rhythm would normally depolarise the ventricles • The resultant heartbeat morphology on the ECG often appears wider and taller than that seen with the underlying rhythm • Ventricular ectopic beats may indicate heart disease, be induced by stimulation (e.g., stress, alcohol, caffeine, medication, cocaine, or amphetamines) or occur naturally - innocently 33 Ventricular ectopic beats Ventricular ectopic beats may occur in patterns, such as: •bigeminy (every other beat), •trigeminy (every third beat), or •quadrigeminy (every forurth beat). They may also occur in sequences, such as couplets, triplets, salvos (four to seven), or episodes (eight or more) This ECG tracing shows ventricular bigeminy, in which every other beat is a ventricular ectopic beat. These beats are premature, wider, and larger than the sinus beats 34 Ventricular tachycardias Ventricular tachycardia occurs when a rapid and repetitive conduction path exists entirely within the ventricles Usually a re-entrant arrhythmia, it is often caused as a result of scarred heart tissue. Once the conduction circuit is initiated, the rhythm may stabilise, extinguish and revert to sinus rhythm, or degenerate into ventricular fibrillation. 35 Ventricular fibrillation [VF] • VF arises when there is uncoordinated contraction of the cardiac muscle of the ventricles in the heart. • As a result the heart fails to adequately pump blood and hypoxia (shortage of oxygen) will occur followed by unconsciousness within 20 - 30 seconds. • Ventricular fibrillation is a medical emergency 36 Ventricular fibrillation [VF] Ventricular fibrillation is a cause of cardiac arrest and sudden cardiac death The ventricular muscle twitches randomly, rather than contracting in unison, and so the ventricles fail to pump blood into the arteries and into systemic/pulmonary circulation Ventricular fibrillation is a sudden lethal arrhythmia responsible for many deaths in the Western world, mostly brought on by ischaemic heart disease 37 Arrhythmias Prognosis • Prognosis depends on the type of arrhythmia. There may be no excess mortality (e.g. with extra systoles), or a very high mortality (e.g. ventricular fibrillation). • A worsening prognosis occurs if the arrhythmia is associated with other aggravating factors such as cardiac ischaemia 38 Assessing and Managing Medical Risk for Insurers www.cardiff.ac.uk/train/medicalrisk Follow us on Twitter @CardiffUniCPD #Medriskwebinar