* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download The Urinary Physiology Chapter 17
Epoxyeicosatrienoic acid wikipedia , lookup
Intracranial pressure wikipedia , lookup
Cardiac output wikipedia , lookup
Circulatory system wikipedia , lookup
Haemodynamic response wikipedia , lookup
Vasopressin wikipedia , lookup
Hemodynamics wikipedia , lookup
Biofluid dynamics wikipedia , lookup
Countercurrent exchange wikipedia , lookup
Renal function wikipedia , lookup
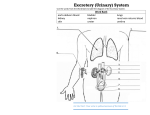
The Urinary Physiology Chapter 17 • Chapter Outline • Structure of Nephron and Renal Corpuscle • Structure of Kidney • 3 Basic Renal Processes: Glomerular Filtration, Tubular Reabsorption, Tubular Secretion. • Glomerular Filtration Rate (GFR) and its Regulation • Regulation of Ion / Water Balance – Role of ADH, Role of Renin – Angiotensin-2 • Regulation of H+ Ion Balance – Acidosis / Alkalosis • Diuretics – drugs that decrease Na+ absorption or increase urine output • Kidney Disease – Uremia, Chronic Kidney Failure • Hemodialysis – artificial removal of waste products and maintenance of electrolyte / acid balance. • Functions of kidney • Regulation of water, electrolyte and pH balance • Removal of waste materials from blood into urine; this includes Nitrogenous wastes Urea, NH3, Uric acid • Removal of foreign chemicals, including drugs • Gluconeogenesis: production of glucose from glycerol and amino acids • Secretion of Hormones: • Erythropoietin - ↑erythrocytes # • Renin – promotes formation of Angiotensin • 1,25-Dihydroxyvitamin D - ↑ calcium absorption • Nephrons • Nephron has renal corpuscle formed of Glomerulus (bunch of capillaries) and Bowman’s capsule • Visceral layer of Capsule has Podocytes having filtration slits between their foot processes • Bowman’s space is present between visceral and parietal layers. • Bowman’s space Proximal convoluted tubule descending limb thin part of Ascending limb thick part of Ascending limb distal convoluted tubule cortical collecting duct medullary collecting duct pelvis ureter • Nephrons Nephrons are units of kidney function Cortical nephrons Medullary Nephrons 1. Present in cortex 1. Present in cortex 2. No loop of Henle or very small one 2. No loop of Henle or very small one 3. Efferent arterioles form peritubular capillaries 3. Efferent arterioles form peritubular capillaries • • • Filtration • Takes place in renal corpuscles Afferent Arteriole glomerular capillaries fenestrae (holes in wall) basement membrane Filtration Slits (between foot processes of Podocytes) Bowman space proximal tubule Water and solutes move out due to blood pressure in capillaries • • • Kidney Each kidney has 1 million Nephrons = functional units of kidney Cortex is outer part having renal corpuscles • • • • • • • • • • • • Medulla is inner part having loop of Henle’s and collecting ducts Medullary collecting ducts medullary pyramid minor calyx major calyx pelvis ureter • Juxtaglomerular Apparatus Macula Densa are a patch of cells in thick ascending loop of Henle passing between afferent and efferent arterioles. At the same point, secretory Juxtaglomerular cells, lie in afferent arteriole Macula Densa + Juxtaglomerular cells = Juxtaglomerular Apparatus = JGA. JGA secretes Renin an enzyme. • Glomerular Filtration Rate Glomerular Filtration Rate = GFR Glomerular capillary blood pressure = PGC = 60mm/Hg Fluid pressure in Bowman’s space = PBS = 15mm/Hg Osmotic pressure due to plasma protein = πGC= 29mm/Hg GFR = PGC – PBS – πGC GFR = 60 – (15 + 29) = 16mm/Hg • Glomerular filtration refers to the movement of fluid and solutes from the glomerular capillaries into Bowman’s space. • Tubular secretion refers to the secretion of solutes from the peritubular capillaries into the tubules. • Tubular reabsorption refers to the movement of materials from the filtrate in the tubules into the peritubular capillaries. • Regulation of Water Balance • Water absorption is coupled to Na+ absorption. • More Na+ absorption means more water absorption. • More water in blood means ↑ blood pressure; loss of water in large quantity means ↓ blood pressure. • Role of ADH = Vasopressin • Vasopressin is a peptide hormone with rapid action • It makes cells of collecting duct embed Aquaporin proteins in their luminal side. Collecting ducts reabsorb a lot of water from urine to release small amount of hyperosmotic urine. • In absence of vasopressin no aquaporins embedded and kidneys excrete large amount of hypoosmotic urine = diuresis, a condition called Diabetes insipidus • • • • • • • The Countercurrent Multiplier System Loop of Henle’s and Collecting ducts of juxtamedullary nephrons form the countercurrent multiplier system Vasa recta the long loops of capillaries around them form the 2nd component of this system. Isoosmotic = 300mOsm; Countercurrent = fluid flows in opposite direction in ascending and descending limbs of loop of Henle and Vasa recta; Concentration Multiplier = from cortex to deep inside medulla the osmolarity of interstial fluid increases gradually from 100 300 600 900 1200mOsm (4 X isoosmotic) Vasa recta removes the water and ions absorbed from filtrate/urine and help to maintain multiplier system The system helps the kidneys to excrete Hypoerosmotic urine • Renin-Angiotensin System Liver angiotensinogen in plasma • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • JGA renin (limiting factor) Renin converts angiotensinogen angiotensin 1 ACE = Angiotensin Converting Enzyme lines endothelium of capillaries and converts angiotensin 1 angiotensin 2 (active hormone) Angiotensin 2 stimulates adrenal cortex to secrete aldosterone; it also causes vasoconstriction; both effects lead to ↑ blood pressure. Salt depletion ↑renin secretion ↑ plasma renin ↑ plasma Angiotensin 1 ↑ plasma Angiotensin 2 ↑ Aldosterone secretion ↑ plasma aldosterone modifies gene expression to increase Na+-K+ pumps, channels for Na+ and K+ ions ↑ Na+ absorption and ↑ water absorption ↑ blood pressure • Atrial Natriuretic Peptide Natrium = Na = Sodium Natriuretic = greater excretion of Na in urine ↑ blood volume expands atria and stimulate them to secrete ANP in blood ANP ↑ Na excretion by inhibiting reabsorption of Na ↑ GFR that leads to greater excretion of Na Inhibits aldosterone secretion • Acid-Base Balance Kidneys secrete H+ in filtrate to reabsorb HCO3CO2 + H2O H2CO3 H+ + HCO3Kidneys generate bicarbonate ions by different means to regulate acid base balance Kidneys and lungs help to maintain pH of interstial fluid and blood is around 7.4 H3PO4 H2PO4- HPO4- 2 PO4-3 is the most important buffer to resist changes in pH. H2CO3 H+ + HCO3- CO3-2 • Acidosis / Alkalosis + Acidosis is the increase of H concentration of arterial plasma. Alkalosis is the decrease of H+ concentration of arterial plasma. Respiratory Acidosis/ alkalosis is due to change in alveolar ventilation – change to eliminate CO2 Metabolic acidosis/alkalosis includes all other situations than respiratory reasons. • Diuretics Diruretics are drugs that decrease Na+ reabsorption; increase the volume of urine passed out; decrease blood volume; decrease blood pressure. Homeostasis attains stability of total-body sodium mass and extra cellular volume. Diuretics are used to treat retention of salt/water by kidney, for example in congestive heart failure. Diuretic drugs are also used in hypertension. • Kidney Diseases Kidney Stones are accumulation of mineral deposits Chronic Kidney Failure develops over the years and is asymptomatic. Untreated hypertension and diabetes can cause it. Kidney failure leads to Uremia. Hemodialysis – patients are put on hemodialysis to remove excess metabolic wastes like urea and restore electrolyte / acid balance. 13% Americans are suffering from it. Accounts for 25% of total Medicare Expenditure.