* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Basic ECG Interpretation
Management of acute coronary syndrome wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Myocardial infarction wikipedia , lookup
Jatene procedure wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Atrial fibrillation wikipedia , lookup
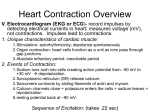
Basic ECG Interpretation Wendy Callaway, RN, BSN Cardiopulmonary Rehab Cardiac Anatomy Four chambers Atria (thin walls, low pressure) Ventricles (thick walls, high pressure) Four Valves Atrioventricular -Tricuspid & mitral Semilunar - Aortic & pulmonic Cardiac Physiology Systole Ventricles in action Aortic and pulmonic valves open Diastole Ventricles at rest Tricuspid and mitral valves open Conduction Pathway SA – right atrium (60-100) AV- non pacer cells that delay impulses Bundle of His- Left & Right bundle branches Purkinje Fibers – located deeper in the muscle tissue ECG Recordings The heart’s electrical currents are transformed into waveforms that represent the heart’s depolarizationrepolarization cycle ECG tracings represent the conduction of electrical impulses from the atria to the ventricles ECG do not represent mechanical activity or contraction Leads Electrode placement is different for each lead Different leads provide different views of the heart Current flows from negative to positive Color codes are often used for lead placement ECG Paper Horizontal axis represents time One small box = 0.04secs 6 sec strip is the standard for Single ECG Vertical axis represents energy One small box = 0.1mV P Wave Represent atrial depolarization; conduction of impulse through atria Location – precedes the QRS Amplitude – 2-3 mm high Duration – 0.06-0.12 sec Configuration – usually round and upright Normal P waves originate from the SA node Abnormal P Waves Peaked, notched or enlarged Stretched atrial tissue Inverted Reverse or retrograde conduction Varying Originate from different sites Absent Blockage PR Interval Tracks the atrial impulse form the atria , AV, Bundle of His, and Branches Location- from P to QRS Duration – 0.12-0.20 sec Abnormal Shortened – impulse did not originate in SA Prolonged –represents conduction delay QRS Complex Represents depolarization of the ventricles Location – follows the PR interval Amplitude 5-30 mm high, depends on lead Duration 0.06-0.10 sec; measured from start of Q wave to end of S wave Configuration – consist of Q wave first negative deflection, R wave positive deflection, S wave negative deflection QRS Complex abnormalities Deep and wide QRS MI Bundle branch block Notched QRS Absent QRS AV Blockage or standstill ST Segment Represents the end of ventricular conduction or depolarization J point – the point that marks the end of the QRS and the start of the ST segment Location – extends from the S wave to the start of T wave Abnormal ST Segment: Elevation – injury Depression - ischemia T Wave Represents ventricular recovery or repolarization Location – follows S wave Configuration- smooth and round Deflection- usually upright in I, II,V3-V6 Abnormal Notched – hidden p wave (indicates atrial depolarization) Tall, peaked, tented – injury or hyperkalemia Inverted (I, II, V3-V6) - ischemia QT Interval Measures ventricular depolarization and repolarization Location – extends from the start of Q wave to the end of the T wave Duration – varies 0.36-0.44 Shows time needed for ventricular cycle U Wave Represents the recovery peroid of the Purkinje conduction fibers Usually not present Location – follows the T wave Configuration – usually round and upright Deflection – upright Prominent U wave – due to hypercalcemia, hypokalemia or digitalis toxicity Steps in Strip Interpretation Check rhythm Calculate rate Evaluate P wave Check PR Interval Check QRS Examine T wave Check QT interval Check for abnormalities/ectopy Naming the Strip Origin of the rhythm Pacemaker Sinus, atria, ventricular Rate characteristics Bradycardia or tachycardia Rhythm abnormalities Flutter, fibrillation, heart block Normal Sinus Rhythm Rhythm: Atrial &ventricular rhythms regular Rate: Atrial & ventricular rate: 60-100 P waves – round, smooth, upright in lead II PR interval – 0.12-0.20sec QRS – less than 0.12sec T wave – upright in lead II QT interval – 0.36-0.44 sec No ectopic or aberrant beats Sinus Bradycardia Rate less than 60 beats per minute Normal during sleep, athletes Normal response to reduced demand for blood (45-59 tolerated by most) Abnormal – MI, drugs, vagal stimulation etc… Symptomatic Response (decreased CO) S/S – hypotension, dizziness, altered mentation, cool, clammy skin, blurred vision, chest pain, syncope, crackles, dyspnea, S3 Sinus Tachycardia Rate greater than 100 bpm Rarely exceeds 180 except with strenuous exercise Increase myocardial oxygen demand Causes Exercise, fever, fear, pain, hemorrhage, hypovolemia, MI, CHF… Symptomatic - S/S decrease CO/reduced ventricular filling time; increase O2 demand Treatment – treat cause Premature Atrial Contractions Originate from an irritable spot or focus in the atria that takes over as the pacemaker PACs may or may not be conducted through the AV node Blocked – p wave only (unlike normal p wave) Usually followed by a pause Pwave may be buried in preceding Twave May cause the P to P intervals of the next two occuring normal beats to be shorter (noncompensatory) Atrial Fibrillation Chaotic, asynchronous electrical activity in atrial tissue Atrial Rate 400-600bpm (quivering) Loss of atrial kick, decreased CO, myocardial perfusion, CHF No P waves – fibrillatory wave or f waves Irregular conduction & Irregular rhythm Atrial Flutter SVT Atrial Rate 250-400bpm (usually 300bpm) Pwaves – saw-tooth appearance (flutter waves) Conduction Rate – 2:1, 3:1, 4:1 (atrial:ventricular response) Rapid ventricular response reduce CO and myocardial perfusion time Premature Ventricular Contractions A premature beat originating in the ventricles P wave is normal, but often buried when PVC occurs Wide QRS complex, > 0.12, may be strangely shaped with an upside- down T wave Rhythm will be regular except for the single beat interrupting the underlying rhythm Bundle Branch Block Conduction failure of the bundle branch Causes prolonged ventricular depolarization on the affected side QRS greater than 0.12sec Ventricular Tachycardia Three or more consecutive PVC’s at >100 bpm P wave is present or absent, QRS complexes are not preceded by associated P waves QRS is wide, >0.12, and bizarre Atria rate is immeasurable, Ventricular rate is 150-200 bpm Ventricular rhythm is usually regular Ventricular Fibrillation Quivering ventricular movements No Pulse PQRST non-identifiable Chaotic Asystole Cardiac standstill Absence of all ventricular activity Treat with pacemaker, CPR, and related drug intervention Paced Rhythm/ Pacer Spike Appears as a vertical line or spike on the ECG strip Atrial – followed by P wave…. Ventricular – followed by QRS A/V – as above The type of pacemaker used and the patient’s condition may affect whether every beat is paced 12 Lead EKG Diagnostic test used to identify pathologic conditions Provide a more complete view of cardiac electrical activity than rhythm strip Must be viewed with other clinical evidence i.e. history, physical, laboratory results and medication ST segment elevation and depression Depression indicates myocardial ischemia, lack of O2 to heart muscle Elevation indicates heart muscle injury or infarct 12 lead EKG can identify the area, but not the extent of an infarct Final Thought! Even with your current knowledge of rhythm strips, always remember to treat the patient, and not the monitor!!