* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Case_Report_28_years_old_man_with_cardiac_arrest
Cardiovascular disease wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Coronary artery disease wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Electrocardiography wikipedia , lookup
Myocardial infarction wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
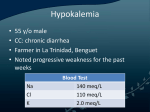
Cardiac Arrest due to severe Hypokalemia – Case Report *Rony Falty S MD, **Retna MD *General Practitioner Premier Jatinegara Hospital ** Department of Cardiology and Vascular Medicine Premier Jatinegara Hospital Abstract We report a case in Premier Jatinegara Hospital, Sudden Cardiac Death due to Severe Hypokalemia . A 28 year old man came to Emergency Department with Cardiac Arrest and No breathing . ECG in Emergency Room Showed reapeated VT Polimorfik (Torsade de pointes ) and Laboratory result revealed severe hypokalemia. Electrolyte imbalances are a common risk factor for Torsade de pointes (TdP), most importantly hypokalemia. Hypokalemia was associated with an increased risk of ventricular tachycardia and ventricular fibrillation Keywords: Torsade de pointes, Hypokalemia Introduction Worldwide, three million people suffer sudden cardiac death annually. Of these, approximately 0.5 million people are younger than 50 years of age. 2 These deaths often emerge from a complex interplay of substrates and triggers. Structural abnormalities are substrates, and perturbations of the environment at the level of heart myocyte and Purkinje fibre membranes (eg, ischemia, electrolyte disturbances, autonomic changes and exercise) are trigger promoting arrhythmia, which may culminate in death. 2 Hypokalemia refers to a below normal serum potassium concentration. It usually indicates a real deficit in total potassium stores. Hypokalemia is present in 7% to 17% of patients with cardiovascular disease. Inadequate management of hypokalemia was found in 24% of hospitalized patients. Hypokalemia is associated with increased risk of arrhythmia in patients with cardiovascular disease, as well as increased all-cause mortality, cardiovascular mortality and heart failure mortality. 2 Torsade de pointes (TdP) is a stereotyped polymorphic ventricular tachycardia characterized by a cyclic shifting of the QRS axis (twisting around the points of the isoelectric line) preceded by a prolonged QT interval. The incidence of TdP is difficult to estimate because it can manifest as syncope or SCD without ECG documentation of the rhythm. . Epidemiological risk factors of TdP such as sex, electrolyte imbalance, ischemia, and QT-prolonging drugs are well established. Electrolyte imbalances are a common risk factor for TdP, most importantly hypokalemia. 3 Case Report A 28 year old man came to Emergency Department with Cardiac Arrest and No breathing , he is discovered by his wife with no breathing and she couldn’t awaken him . From Heteroanamnesis symptoms like chest pain, hard to breath , asthenia, fever, headache, nausea and vomit, and diarrhea were denied. His medical history is hypertension and under control with amlodipine 5 mg once a day. We did continuous CPR & Defibrillation and also gave him medication like adrenalin. ECG in Emergency Room Showed repeated VT Polimorphic ( Torsade de Pointes ), with heart rate 73 and SpO2 94%.We also gave him amiodaron, and MgSO4 while doing Resucitation . Figure 1 : ECG Torsade de Pointes After 120 minutes resuscitation patient was stable ( ROSC ). The physical examination after resuscitation revealed Airway was patent with Endotracheal tube, carotid pulse was palpabled. Respiration on intubation with bagging , temperature afebris and cold extremities. Physical examination were normal. His laboratory result showed hemoglobin 15 L 26900 Thrombosit 254000 Na 144 Kalium 1.36 Cl 102 Calcium 8.6 Magnesium 4.74 Creatinine Kinase 1947 CKMB 177 Troponin T 5.2757 Urea 56 Creatinine 1.57 . Urinalysis : Kalium Urine 169 SGOT/SGPT 361/141 Blood Gluocose 326 Cortisol 22.10. Blood Gas : Lactat 1.92 pH 7.54 pCO2 38.4 pO2 133 HCO3 32.9 Sat O2 99 BE 9.10 Patient tranfered to ICU after his condition stable with Blood pressure 116/70 ( on dobutamin ), heart rate 125 times/minute and ECG VES Bigemini. He also got Kalium correction 50 meq/4 hours and be monitored every 1 hour after correction. His Echocardiography result showed Global normokinetik with Ejection fraction 70% Note : his family refused to check renin and aldosterone. Discussion Hypokalemia is generally defined as a serum potassium concentration that is lower than 3.5 mmol/L. Hypokalemia was associated with an increased risk of ventricular tachycardia and ventricular fibrillation. Thus, the incidence of ventricular fibrillation has been found to be fivefold higher in patients with a low serum potassium concentration than in patients with a high serum potassium concentration. 2 Figure 2. Diagnositic Evaluation of Hypokalemia.1 Table 1. Causes of Potassium Loss . 1 Two major side-effects of hypokalemia affect the cardiovascular system are hypokalemia-related hypertension and hypokalemia-induced ventricular arrhythmia. The mechanism of hypokalemia-induced hypertension is not completely clear. One component of this type of hypertension appears to be salt retention. Hypokalemia leads to intravascular volume expansion as a result of renal NaCl retention. Hypokalemia may also potentiate the hypertensive effects of various neurohumoral agents. Ventricular arrhythmias are a second cardiovascular side-effect of hypokalemia. Several prospective studies show that hypokalemia predisposes patients to the development of a variety of ventricular arrhythmias, including ventricular fibrillation. 1 Table 2. Clinical Presentations of Patients with Ventricular Arrhytmias and Sudden Cardiac Death. 4 A relatively recent meta-analysis of six singledose, placebo- controlled studies of 168 patients receiving beta-adrenoceptor agonists for asthma showed reductions in potassium levels by 0.23 mmol/L to 0.58 mmol/L (mean 0.36 mmol/L; 95% CI 0.18 mmol/L to 0.54 mmol/L). In one study (39), the reduction in potassium level by 0.58 mmol/L was associated with a prolongation in the electrocardiogram of the corrected QT (QTc) interval by 78 ms and an increase in heart rate by 61 beats/min. Because prolonged QTc interval reflects abnormal cardiac repolarization, it is a predictor of dangerous arrhythmia, and there is speculation that severe hypokalemia is involved in some cases of sudden death among asthmatic patients.2 Torsade de pointes (TdP) is a stereotyped polymorphic ventricular tachycardia characterized by a cyclic shifting of the QRS axis (twisting around the points of the isoelectric line) preceded by a prolonged QT( Which Indicates a lengthened action potensial duration). it can produced by early afterdepolrization, particulary in patients who have a prolong QT. interval Epidemiological risk factors of TdP such as sex, electrolyte imbalance, ischemia, and QT-prolonging drugs are well established. Electrolyte imbalances are a common risk factor for TdP, most importantly hypokalemia. 3 Yan et al have described an experimental model involving canine left ventricular wedge preparations to better understand the action potential in an electrically coupled environment while removing the potentially confounding variable of anesthesia. Microelectrodes can then be used to record action potentials in epicardium, midmyocardium, and endocardium, as well as subendocardial Purkinje fibers. This model has established that M cells, which make up the midmyocardium, have disproportionate prolongation of APD ( Action Potensial Duration) in response to hypokalemia or class III antiarrhythmics compared with other layers of cells within the left ventricular myocardium. IKr blocking agents such as d-sotalol were also found to preferentially prolong the APD of the M cell. Figure 3. Transmural dispersion of repolarization Shown here are the sotalol-induced changes (B) compared to control (A) in action potential duration of each layer of the canine left ventricular arterially perfused wedge. Note the disproportionately prolonged M-cell action potential and its corresponding contribution to the prolongation of the time from the peak to the end of the T wave Withdrawal of any offending drugs and correction of electrolyte abnormalities are recommended in patients presenting with torsades de pointes (Level of Evidence: A) Class 1 Potassium repletion to 4.5 to 5 mM/L may be considered for patients who present with torsades de pointes. (Level of Evidence: B) Class IIb.4 Management with intravenous magnesium sulfate is reasonable for patients who present with LQTS and few episodes of torsades de pointes. Magnesium is not likely to be effective in patients with a normal QT interval. (Level of Evidence: B) Class IIa.4 Intravenous lidocaine or oral mexiletine may be considered in patients who present LQT3 and torsades de pointes. (Level of Evidence: C) Class IIb.4 TdP is difficult to estimate because it can manifest as syncope or SCD. That is why ECG and some laboratory test ( e.g Electrolite, Cardiac enzim etc ) are very important because it will help us to treat the patient with the correct way.3 Conclusion The etiology of Hypokalemia in this patient is still questionable because he refused to do further laboratory test. Hypokalemia was associated with an increased risk of ventricular tachycardia and ventricular fibrillation. The incidence of TdP is difficult to estimate because it can manifest as syncope or SCD without ECG documentation of the rhythm. Correction of electrolyte abnormalities are recommended in patients presenting with torsades de pointes. Management with intravenous magnesium sulfate is reasonable for patients who present with LQTS and few episodes of torsades de pointes. References 1. David Weiner, Charles S. Wingo. Hypokalemia-Consequences , Causes , and Correction, Division of Nephrology, Hypertension and Transplantation, University of Florida College of Medicine, and Gainesville Veterans Administration Medical Center, Gainesville, Florida.1997 2. k kjeldsen. Hypokalemia and sudden cardiac death. exp Clin Cardiol 2010;15(4):e96-e99. 3. Andrew J. Sauer, Christopher Newton-Cheh .Clinical and Genetic Determinants of Torsade de Pointes Risk. Circulation. 2012;125:1684-1694 4. ACC/AHA/ESC 2006 Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death—Executive Summary