* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Effects of Hypo- and Hyperthyroidism on Noradrenergic Activity and
Survey
Document related concepts
Transcript
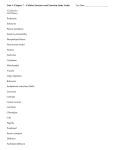
0021-972X/03/$15.00/0 Printed in U.S.A. The Journal of Clinical Endocrinology & Metabolism 88(12):5605–5608 Copyright © 2003 by The Endocrine Society doi: 10.1210/jc.2003-030576 Effects of Hypo- and Hyperthyroidism on Noradrenergic Activity and Glycerol Concentrations in Human Subcutaneous Abdominal Adipose Tissue Assessed with Microdialysis MARTIN HALUZIK, JARA NEDVIDKOVA, VLADIMIR BARTAK, IVANA DOSTALOVA, PETR VLCEK, PAVEL RACEK, MICHAL TAUS, STEPAN SVACINA, SALVATORE ALESCI, AND KAREL PACAK Third Department of Medicine (M.H., S.S.), First Faculty of Medicine; Nuclear Medicine Department (P.R., P.V.), Second Faculty of Medicine; and Outpatient Endocrine Clinic (M.T.), Prague, Czech Republic; Institute of Endocrinology (J.N., V.B., I.D.), Prague, Czech Republic 11694; Pediatric and Reproductive Endocrinology Branch (S.A., K.P.), National Institute of Child Health and Human Development, National Institutes of Health, Bethesda, Maryland 20892 20892-1583; and Clinical Neuroendocrinology Branch (S.A.), National Institute of Mental Health, National Institutes of Health, Bethesda, Maryland 20892 Thyroid hormones play a major role in lipid metabolism. However, whether they directly affect lipolysis locally in the adipose tissue remains unknown. Therefore, we measured abdominal sc adipose tissue norepinephrine (NE), basal, and isoprenaline-stimulated lipolysis in 12 hypothyroid patients (HYPO), six hyperthyroid patients (HYPER), and 12 healthy controls by in vivo microdialysis. Adipose tissue NE was decreased in HYPO and increased in HYPER compared with controls (90.4 ⴞ 2.9 and 458.0 ⴞ 69.1 vs. 294.9 ⴞ 19.5 pmol/liter, P < 0.01). Similarly, basal lipolysis, assessed by glycerol assay, was lower in HYPO and higher in HYPER than in controls (88.2 ⴞ 9.9 and 566.0 ⴞ 42.0 vs. 214.3 ⴞ T HYROID HORMONES (THs) exert several important metabolic actions, including lipolysis enhancement (1). Hyperthyroid (HYPER) states result in increased oxygen consumption, thermogenesis, and lipid mobilization, whereas hypothyroid (HYPO) states are accompanied by decreased oxygen consumption and energy expenditure (2). Metabolic changes induced by THs are accomplished in part directly, through specific nuclear receptors expressed in target tissues, and indirectly, by modulation of other hormones’ action (3). Some of the symptoms most typically associated with HYPER/HYPO states, such as tachy/bradycardia and increased/decreased perspiration, may reflect increased/ decreased sympathetic activity. Although it has been previously reported that THs can amplify catecholamine actions in different tissues, the exact mechanism of this effect is not entirely understood (1, 4). Catecholamines are released from neural endings in the sc adipose tissue, where glycerol is released after lipolysis of triacylglycerols (5, 6). There is evidence that the lipolytic effect of THs may be, at least in part, mediated by catecholamines. Animal studies have shown that THs can influence the adrenergic activities of brown and white adipose Abbreviations: BMI, Body mass index; fT3 and fT4, serum free T3 and T4; HYPER, hyperthyroid; HYPO, hypothyroid; NE, norepinephrine; TT3 and TT4, total T3 and T4; TH, thyroid hormone. 5.1 mol/liter P < 0.01). The relative magnitude of isoprenaline-induced glycerol increase was smaller in HYPO (39 ⴞ 19.4%, P < 0.05 vs. basal) and higher in HYPER (277 ⴞ 30.4%, P < 0.01) than in controls (117 ⴞ 5.6%, P < 0.01). The corresponding changes in NE after isoprenaline stimulation were as follows: 120 ⴞ 9.2% (P < 0.05), 503 ⴞ 113% (P < 0.01), and 267 ⴞ 17.2 (P < 0.01). In summary, by affecting local NE levels and adrenergic postreceptor signaling, thyroid hormones may influence the lipolysis rate in the abdominal sc adipose tissue. (J Clin Endocrinol Metab 88: 5605–5608, 2003) tissue through modulation of postreceptor signaling events, including adenylate cyclase activity (4, 7, 8). Moreover, increased/decreased lipolytic response to norepinephrine (NE) was detected in cultured adipocytes derived from HYPER/HYPO patients. The increased lipolytic response was accompanied by a 2-fold increase in the number of adipocyte -adrenergic binding sites (9). More recently, increased abdominal and femoral adipose tissue lipolysis was demonstrated in HYPER patients in vivo (10). Despite this evidence, it remains unknown if altered thyroid function is associated with local changes in abdominal sc fat catecholamine levels or not. A relatively new approach used in an effort to gain a better understanding of tissue metabolism is the measurement and quantification of compounds in the interstitial space. This is accomplished by using the microdialysis technique that is based on the principle of diffusion through a semipermeable membrane (11). True equilibrium can be accomplished across the membrane when low flow rates are used (12). Microdialysis can be used to monitor for changes in the flux of different molecules from the interstitial fluid to the dialysate and has been applied to a large number of human tissues since it was first introduced (13–17). In the present study, we used in vivo microdialysis to investigate possible changes in NE concentration and NEstimulated lipolysis measured as changes of local glycerol 5605 5606 J Clin Endocrinol Metab, December 2003, 88(12):5605–5608 concentrations in the abdominal sc adipose tissue of HYPER and HYPO patients and healthy individuals. Subjects and Methods Study subjects Twelve HYPO women [age, 41.4 ⫾ 14 yr; body mass index (BMI), 28.6 ⫾ 2.1 kg/m2; mean ⫾ sem], six HYPER women (age, 36.8 ⫾ 12.6 yr; BMI, 20.6 ⫾ 1.9 kg/m2) and 12 healthy women (age: 32.0 ⫾ 10 yr; BMI: 23 ⫾ 1.9 kg/m2), were included in this study. Only untreated patients newly diagnosed as HYPO and HYPER were included into the present study. All patients were studied a few days after the diagnosis of thyroid dysfunction. After the study was carried out, all patients were given appropriate medication. All participants were nonsmokers, had no history of allergies, and had been free of medication for at least 2 wk before the study. Healthy volunteers had no history of obesity, thyreopathies, gastrointestinal disease, eating disorders, or other psychiatric disorders, and normal physical exam and electrocardiogram. Blood tests confirmed normal blood count, liver, and renal functions. Except for thyroid disorders, all patients were clinically stable, not suffering from any major health problems that could affect their nutritional status such as gastrointestinal disease, eating disorders, or other psychiatric disorder. Upon enrollment, all subjects were placed on a low monoamine diet. Written informed consent was provided by all participants before being enrolled in the study, which was approved by the Human Ethical Review Committee, Institute of Endocrinology, Prague, Czech Republic. Blood and microdialysate sampling All subjects were studied while resting supine on a comfortable bed in a room kept at 23–25 C. At 0800 h, after overnight fasting, a venous catheter was placed in the antecubital vein and a CMA-60 catheter with cut-off of 20 kDa (CMA Microdialysis, Stockholm, Sweden) was inserted sc under sterile conditions (8 –10 cm left to the umbilicus, at least 45 min before blood and microdialysate sampling). Sterile Ringer buffer was used as perfusate. After insertion of the CMA-60 catheter, perfusion with Ringer solution supplemented with 50 mmol/liter of ethanol was started at a flow rate of 2 l/min using CMA 107 microdialysis pumps (CMA Microdialysis). Microdialysate samples were collected every 30 min over a 2-h period, 1 h before (basal condition) and 1 h after (stimulated condition) local administration of the 1,2-adrenergic agonist isoprenaline (Saventrine, 0.1 mmol/liter, Pharmax, Bexley, Kent, UK). Microdialysate samples for catecholamine determination were collected into microvials containing preserving agents (0.2 n of acetic acid and 0.04 mol/liter of H3PO4). Both blood and microdialysate samples were placed on ice immediately after collection and stored at ⫺80 C until being analyzed. Haluzik et al. • Lipolysis and Noradrenergic Activity Hormonal and biochemical assays NE concentration in plasma and microdialysate samples was measured by HPLC with electrochemical detection after batch alumina extraction as previously described (18). Serum total free (f) and total (T) T3 and T4 were assayed by commercially available RIA kits (Immunotech, Prague, Czech Republic). TSH was measured with an electrochemiluminescence method (Elecsis 2010, Roche, Basel, Switzerland), the sensitivity of TSH assay was 0.005 mU/liter. Glycerol was measured colorimetrically with a commercial kit (Randox). Changes in sc abdominal adipose tissue blood flow were determined using the ethanol dilution technique, based on the Fick’s principle (11). According to this method, differences between ethanol concentration in the perfusate (inflow) and in the dialysate (outflow) reflect changes in blood flow. Ethanol was measured using a standard enzymatic assay (Sigma Diagnostics, St. Louis, MO). For simplicity, the microdialysate ethanol concentration/ perfusate ethanol concentration ratio is referred to as “ethanol ratio.” Statistical analysis Results are presented as mean values ⫾ sem. Differences between basal and isoprenaline-stimulated lipolysis were analyzed by paired t tests. Differences between groups of subjects were analyzed by ANOVA, followed by Student-Newman-Keuls post hoc test. The level of statistical significance was set at P ⬍ 0.05. Results Clinical, anthropometric, and major laboratory characteristics of HYPER, HYPO, and control subjects are summarized in Table 1. HYPER/HYPO patients had significantly lower/ higher BMI, than controls, respectively. Heart rate was significantly higher in HYPER patients compared with both HYPO patients and control subjects (Table 1). HYPO patients had significantly lower TT3, fT3, TT4, fT4 levels, and significantly higher serum TSH and plasma NE levels compared with control subjects (Table 1). As expected, hyperthyroidism resulted in suppressed TSH and markedly increased TT3, fT3, TT4, and fT4 levels. No differences in plasma NE levels were found between HYPER and control subjects (Table 1). Serum glycerol levels were significantly lower in HYPO and higher in HYPER patients relative to control subjects. Free fatty acids were higher in HYPER patients than in both HYPO patients and control subjects. In contrast, no significant differences among the experimental TABLE 1. Clinical, anthropometric, and major laboratory characteristics of the HYPO, HYPER, and healthy control (HC) subjects enrolled in this study Age BMI (kg/m2) TT3 (nmol/liter) fT3 (pmol/liter) TT4 (nmol/liter) fT4 (pmol/liter) TSH (mU/liter) NE (nmol/liter) Glycerol (mol/liter) FFA (mol/liter) Insulin (mU/liter) Glucose (mmol/liter) Heart rate (BPM) HC HYPO HYPER 34.0 ⫾ 12.0 23.0 ⫾ 1.9 2.71 ⫾ 0.32 6.1 ⫾ 1.1 132 ⫾ 18.8 13.9 ⫾ 1.1 1.9 ⫾ 0.6 5.98 ⫾ 0.80 202 ⫾ 39 498 ⫾ 89 8.7 ⫾ 1.3 4.73 ⫾ 0.11 73 ⫾ 3 41.4 ⫾ 14.0 28.6 ⫾ 2.1a 1.03 ⫾ 0.12b 2.2 ⫾ 0.3b 49.0 ⫾ 14.8b 4.2 ⫾ 2.8b 75.9 ⫾ 24.1b 12.40 ⫾ 2.65a 89 ⫾ 33.8a 399 ⫾ 99 11.6 ⫾ 3.1 4.8 ⫾ 0.15 67 ⫾ 4 36.8 ⫾ 12.6 20.6 ⫾ 1.9c 9.37 ⫾ 1.11b,d 31 ⫾ 11b,d 272.7 ⫾ 26.6b,d 54 ⫾ 33d 0.01 ⫾ 0.001d 4.92 ⫾ 0.87c 449 ⫾ 56.2a,c 788 ⫾ 141a,c 9.3 ⫾ 2.1 4.98 ⫾ 0.17 84 ⫾ 4a,c All values are expressed as means ⫾ SEM. FFA, Free fatty acids; BPM, beats per minute. a P ⬍ 0.05 and b P ⬍ 0.001 vs. HC; c P ⬍ 0.05 and d P ⬍ 0.001 vs. HYPO. Haluzik et al. • Lipolysis and Noradrenergic Activity groups were found in plasma glucose and serum insulin levels (Table 1). Ethanol ratios were similar in controls and HYPO patients, whereas they were significantly decreased in HYPER patients in comparison to both controls (P ⬍ 0.05) and HYPO (P ⬍ 0.05) (Fig. 1). Compared with glycerol and NE values measured in healthy subjects (214.3 ⫾ 5.1 mol/liter and 294.9 ⫾ 19.5 pmol/liter, respectively) basal sc fat glycerol and NE levels were significantly lower in HYPO (88.2 ⫾ 9.9 mol/liter, P ⬍ 0.01; and 90.4 ⫾ 2.9 pmol/liter, P ⬍ 0.01, respectively), and higher in HYPER patients (566 ⫾ 42 mol/liter, P ⬍ 0.01 and 458.0 ⫾ 69.1 pmol/liter, P ⬍ 0.01, respectively) (Figs. 2 and 3). Compared with basal values, local isoprenaline administration induced a significant increase of both glycerol and NE levels in controls (466.2 ⫾ 12 mol/liter, P ⬍ 0.01 and 1082.7 ⫾ 50.8 pmol/liter, P ⬍ 0.001, respectively), as well as in HYPO (123.0 ⫾ 10.2 mol/liter, P ⬍ 0.05 and 199.7 ⫾ 8.4 pmol/liter, P ⬍ 0.01, respectively), and HYPER patients (2135.0 ⫾ 172.0 mol/liter, P ⬍ 0.01 and 2765.8 ⫾ 521.8 pmol/liter, P ⬍ 0.001, respectively) (Figs. 2 and 3). The rel- J Clin Endocrinol Metab, December 2003, 88(12):5605–5608 5607 FIG. 3. Norepinephrine concentration in the abdominal sc fat tissue during basal conditions and after isoprenaline-stimulated lipolysis in healthy control (HC), HYPO, and HYPER subjects. Results are presented as scatter plots of individual values with bars showing means. *, P ⬍ 0.01 vs. healthy controls; ⫹, P ⬍ 0.01 vs. HYPO subjects. ative magnitude of the isoprenaline-induced increase in glycerol levels was significantly smaller in HYPO (39 ⫾ 19.4%, P ⬍ 0.05) and higher in HYPER (277 ⫾ 30.4%, P ⬍ 0.01) than in controls (117 ⫾ 5.6%, P ⬍ 0.01). Local changes in NE concentrations after isoprenaline stimulation followed a similar pattern in all three groups: 267 ⫾ 17.2% of increase in the control group, 120 ⫾ 9.2% in HYPO (P ⬍ 0.05), and 503 ⫾ 113% in HYPER patients (P ⬍ 0.01). Discussion FIG. 1. Ethanol ratio (dialysate ethanol concentration/perfusate ethanol concentration) in healthy control, HYPO, and HYPER subjects. Results are presented as means ⫾ SEM. *, P ⬍ 0.05 vs. healthy controls; ⫹, P ⬍ 0.05 vs. HYPO subjects. FIG. 2. Glycerol concentration in the abdominal sc fat tissue during basal conditions and after isoprenaline-stimulated lipolysis in healthy control (HC), HYPO, and HYPER subjects. Results are presented as scatter plots of individual values with bars showing means. *, P ⬍ 0.01 vs. healthy controls; ⫹, P ⬍ 0.01 vs. HYPO subjects. Normal thyroid function is essential to regulate lipid metabolism. It is, however, uncertain whether THs directly affect lipolysis in the sc adipose tissue and to what extent those changes may overall contribute to determine the metabolic phenotype of patients with thyroid dysfunctions. Our study was designed to determine local noradrenergic activity and basal and isoprenaline-stimulated lipolysis in the abdominal sc adipose tissue of patients with thyroid dysfunctions. We found that the thyroid functional status strongly influences both the noradrenergic and lipolytic activities of sc abdominal adipose tissue in vivo. HYPO patients displayed significantly decreased sc fat NE and glycerol concentrations compared with healthy subjects, whereas the opposite applied to HYPER patients. The parallel changes in basal sc fat levels of NE and glycerol observed in patients with thyroid dysfunctions suggest that altered lipolysis in these subjects may result from local modification in adrenergic activity. We suggest that one explanation of this finding is the effect of the thyroid status on the adrenergic receptors number and sensitivity (5, 6, 19). Alternatively, adrenergic postreceptor signaling in the adipose tissue may be involved on multiple levels, including adenylate cyclase activity (7, 9, 20). Isoprenaline-stimulated lipolysis was also less pronounced in HYPO patients than in healthy controls. It is, therefore, likely that the altered lipolytic response in patients with thyroid disorders results from a combination of local NE changes and other mechanisms, including modulation of other lipolysis regulating hormones or enzymes by THs. For 5608 J Clin Endocrinol Metab, December 2003, 88(12):5605–5608 example, THs have been shown to influence the lipolytic action of growth hormone (21) and directly affect the activity of hormone sensitive lipase in adipose tissue (22). Moreover, the adipose tissue itself produces a number of hormones, such as leptin, adiponectin, resistin, and others, that can influence local lipolysis and/or triglyceride synthesis through paracrine mechanisms (23–25). However, no information is currently available regarding the effect of THs on the adipose tissue paracrine functions in vivo. We found a discrepancy between local and systemic NE levels in both HYPO and HYPER patients. In fact, our group and others had previously shown that hypothyroidism is accompanied by increased systemic NE levels, whereas no change in this parameter was found in HYPER patients (1, 26). The possible explanation for this discrepancy could be that plasma NE concentration reflects the net amount of this hormone released from different tissues, whereas microdialysate NE concentration measures the quantity released in adipose tissue. Local blood flow in our study was significantly higher in HYPER and unchanged in HYPO patients compared with controls. Thus, if anything, increased local blood flow would cause higher NE outflow from adipose associated with low NE sc abdominal adipose tissue concentrations (27). Therefore, higher sc fat NE levels in HYPER patients result from increased sympathetic activity in sc abdominal adipose. This suggestion is further supported by other studies showing that the role of systemic catecholamines in the regulation of adipose tissue lipolysis is only minor relative to that of catecholamines locally released from sympathetic nerve endings (28, 29). In summary, in the present study we demonstrated that altered thyroid function is accompanied by changes in abdominal sc fat adrenergic and lipolytic activities, which may explain some of the phenotypic features observed in patients with functional thyroid disorders. Acknowledgments We thank Ms. Diana Riegerova, Jana Novotna, Romana Bajtlova, Christina Kukura, and Shiromi Perera for their technical assistance. Received April 4, 2003. Accepted June 14, 2003. Address all correspondence and requests for reprints to: Karel Pacak, M.D., Ph.D., DSc Chief, Unit on Clinical Neuroendocrinology, Building 10, Room 9D42, National Institute of Child Health and Human Development, National Institutes of Health, 10 Center Drive, MSC-1583, Bethesda, Maryland 20892-1583. E-mail: [email protected]. The study was supported by a grant agency of the Czech Republic, GACR, no. 303/00/1555. References 1. Levey GS, Klein I 1990 Catecholamine-thyroid hormone interactions and the cardiovascular manifestations of hyperthyroidism. Am J Med 88:642– 646 2. Duntas LH 2002 Thyroid disease and lipids. Thyroid 12:287–293 3. Brent GA 2000 Tissue-specific actions of thyroid hormone: insights from animal models. Rev Endocr Metab Disord 1:27–33 4. Rubio A, Raasmaja A, Maia AL, Kim KR, Silva JE 1995 Effects of thyroid hormone on norepinephrine signaling in brown adipose tissue. I. 1- and 2-Adrenergic receptors and cyclic adenosine 3⬘, 5⬘-monophosphate generation. Endocrinology 136:3267–3276 Haluzik et al. • Lipolysis and Noradrenergic Activity 5. Londos C, Brasaemle DL, Schultz CJ, Adler-Wailes DC, Levin DM, Kimmel AR, Rondinone CM 1999 On the control of lipolysis in adipocytes. Ann NY Acad Sci 892:155–168 6. Langin D, Lucas S, Lafontan M 2000 Millennium fat-cell lipolysis reveals unsuspected novel tracks. Horm Metab Res 32:443– 452 7. Chaudhry A, Granneman JG 1997 Effect of hypothyroidism on adenylyl cyclase activity and subtype gene expression in brown adipose tissue. Am J Physiol 273:R762–R767 8. Rubio A, Raasmaja A, Silva JE 1995 Thyroid hormone and norepinephrine signaling in brown adipose tissue. II: Differential effects of thyroid hormone on  3-adrenergic receptors in brown and white adipose tissue. Endocrinology 136:3277–3284 9. Wahrenberg H, Wennlund A, Arner P 1994 Adrenergic regulation of lipolysis in fat cells from hyperthyroid and hypothyroid patients. J Clin Endocrinol Metab 78:898 –903 10. Riis AL, Gravholt CH, Djurhuus CB, Norrelund H, Jorgensen JO, Weeke J, Moller N 2002 Elevated regional lipolysis in hyperthyroidism. J Clin Endocrinol Metab 87:4747– 4753 11. Fellander G, Linde B, Bolinder J 1996 Evaluation of the microdialysis ethanol technique for monitoring of subcutaneous adipose tissue blood flow in humans. Int J Obes Relat Metab Disord 20:220 –226 12. Rosdahl H, Hamrin K, Ungerstedt U, Henriksson J 1998 Metabolite levels in human skeletal muscle and adipose tissue studied with microdialysis at low perfusion flow. Am J Physiol 274:E936 –E945 13. Lonnroth P, Jansson PA, Smith U 1987 A microdialysis method allowing characterization of intercellular water space in humans. Am J Physiol 253: E228 –E231 14. Bruce S, Tack C, Patel J, Pacak K, Goldstein DS 2002 Local sympathetic function in human skeletal muscle and adipose tissue assessed by microdialysis. Clin Auton Res 12:13–19 15. Kennergren C, Mantovani V, Strindberg L, Berglin E, Hamberger A, Lonnroth P 2003 Myocardial interstitial glucose and lactate before, during, and after cardioplegic heart arrest. Am J Physiol Endocrinol Metab 284:E788 –E794 16. Meixensberger J, Kunze E, Barcsay E, Vaeth A, Roosen K 2001 Clinical cerebral microdialysis: brain metabolism and brain tissue oxygenation after acute brain injury. Neurol Res 23:801– 806 17. Dabrosin C 2001 Technical aspects of microdialysis of human breast. Scand J Clin Lab Invest 61:269 –272 18. Pacak K, Palkovits M, Yadid G, Kvetnansky R, Kopin IJ, Goldstein DS 1998 Heterogeneous neurochemical responses to different stressors: a test of Selye’s doctrine of nonspecificity. Am J Physiol 275:R1247–R1255 19. Richelsen B, Sorensen NS 1987 ␣2- and -Adrenergic receptor binding and action in gluteal adipocytes from patients with hypothyroidism and hyperthyroidism. Metabolism 36:1031–1039 20. Hellstrom L, Wahrenberg H, Reynisdottir S, Arner P 1997 Catecholamineinduced adipocyte lipolysis in human hyperthyroidism. J Clin Endocrinol Metab 82:159 –166 21. Richelsen B 1997 Action of growth hormone in adipose tissue. Horm Res 48(Suppl)5:105–110 22. Kern PA, Ranganathan G, Yukht A, Ong JM, Davis RC 1996 Translational regulation of lipoprotein lipase by thyroid hormone is via a cytoplasmic repressor that interacts with the 3⬘ untranslated region. J Lipid Res 37:2332– 2340 23. Minokoshi Y, Kim YB, Peroni OD, Fryer LG, Muller C, Carling D, Kahn BB 2002 Leptin stimulates fatty-acid oxidation by activating AMP-activated protein kinase. Nature 415:339 –343 24. Steppan CM, Bailey ST, Bhat S, Brown EJ, Banerjee RR, Wright CM, Patel HR, Ahima RS, Lazar MA 2001 The hormone resistin links obesity to diabetes. Nature 409:307–312 25. Yamauchi T, Kamon J, Minokoshi Y, Ito Y, Waki H, Uchida S, Yamashita S, Noda M, Kita S, Ueki K, Eto K, Akanuma Y, Froguel P, Foufelle F, Ferre P, Carling D, Kimura S, Nagai R, Kahn BB, Kadowaki T 2002 Adiponectin stimulates glucose utilization and fatty-acid oxidation by activating AMPactivated protein kinase. Nat Med 8:1288 –1295 26. Vavrejnova V, Nedvidkova J, Husek P, Zamrazil V, Nemec J 1992 Increased levels of noradrenaline in hypothyroidism and its association with cardiovascular system function. Vnitr Lek 38:1195–1200 27. Nonogaki K 2000 New insights into sympathetic regulation of glucose and fat metabolism. Diabetologia 43:533–549 28. Lafontan M, Berlan M 1993 Fat cell adrenergic receptors and the control of white and brown fat cell function. J Lipid Res 34:1057–1091 29. Barbe P, Galitzky J, Riviere D, Senard JM, Lafontan M, Garrigues M, Berlan M 1993 Effects of physiological and pharmacological variation of sympathetic nervous system activity on plasma non-esterified fatty acid concentrations in man. Br J Clin Pharmacol 36:25–30