* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Congenital Heart Disease from the Block
Cardiac contractility modulation wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Electrocardiography wikipedia , lookup
Heart failure wikipedia , lookup
Echocardiography wikipedia , lookup
Artificial heart valve wikipedia , lookup
Coronary artery disease wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Rheumatic fever wikipedia , lookup
Myocardial infarction wikipedia , lookup
Cardiac surgery wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Aortic stenosis wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Atrial septal defect wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
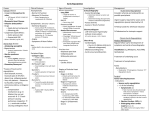
Congenital Heart Disease from the Block (as in J-Lo from the block, pun definitely intended!) Premchand Anne, MD, MPH PGY IV 9/1/2005 Objectives ►Fetal and neonatal ► DA ► Pathophysiology circulation Left to Right shunts Obstructive Valvular regurgitation Cyanotic congenital heart disease Fetal Circulation Fetal Circulation: four shunts Placenta ► Receives 55% of total CO ► Lowest vascular resistance Ductus venosus ► From placenta: has 70% sats ► Highest PO2: umbilical vein (30) Foramen ovale ► 1/3 of RA return goes to LA Oxygenate brain and coronaries better (PO2=28) Lower body: PO2=24 Ductus arteriosus ► PA => Descending Aorta => placenta Neonatal Circulation ► Change in gas exchange from placenta to lungs Increase in systemic vascular resistance due to absence of placenta and closure of DA due to presence of increased PO2 Reduction of PVR after lung expansion due to oxygen, increased LA return, fall in RA pressure due to DA closure and increase in systemic pressure => closure of foramen ovale Rapid initial fall, slower fall by 6-8 weeks and then after 2 years Objectives ► Fetal and neonatal circulation ►DA ► Pathophysiology Left to Right shunts Obstructive lesions Valvular regurgitation Cyanotic congenital heart disease DA closure ► Within 10-15 hours of birth ► Postnatal increase in Oxygen is the strongest stimulus for closure; premies don’t respond as well to oxygen. ► PGE2 decreases after birth due to loss of placenta and increased pulmonary blood flow to wash it off. ► Indomethacin closes PDAs ► Maternal ingestion of ASA can cause Persistent Pulmonary Hypertension of the Newborn (premature closure of DA and poor development of arterioles) ► PGE1 keeps DA open. Pulmonary arteries and DA respond in opposite manner Objectives ► Fetal and neonatal circulation ► DA ► Pathophysiology Left to Right shunts Obstructive lesions Valvular regurgitation Cyanotic congenital heart disease Left to Right Shunts ► ASD ► VSD ► PDA ► ECD Left to Right Shunts-ASD ASD ► RA and RV dilated ► RV dilation => increased time for repolarization => RBBB on EKG ► NO CHF until 6-8 weeks when PVR drops considerably. ASD Left to Right Shunts-VSD VSD ► LA and LV dilated in a small to moderate VSD: does this make sense? Shunt occurs only during systole, where the blood goes from LV to pulmonary artery There is increased pulmonary return to LA and then to LV => dilation ► RV, LA, LV are all dilated in a large size VSD ► Complication of large VSD=Eisenmenger’s => generalized cyanosis VSD Left to Right Shunts-PDA PDA ► Onset of CHF is similar to that of a VSD ► Complication of a large PDA=> Eisenmenger’s => differential cyanosis (lower body cyanosis): WHY? PDA ECD ► Endocardial cushion is responsible for upper part of ventricular septum and lower part of atrial septum ► Absence leads to VSD, primum ASD, clefts in mitral and tricuspid valves Left to Right Shunts-ECD ECD ► Primum ASD = Secundum ASD; RA and RV are dilated with widely split and fixed S2 and systolic ejection murmur at left upper sternal border. ► RBBB due to prolonged repolarization ► Obligatory shunt with LV -> RA lesion ECD Objectives ► Fetal and neonatal circulation ► DA ► Pathophysiology Left to Right shunts Obstructive lesions Valvular regurgitation Cyanotic congenital heart disease Obstructive Lesions ► Ventricular Outflow obstruction Aortic stenosis Pulmonary stenosis Coarctation of the aorta ► Stenosis of AV valves Mitral stenosis Tricuspid stenosis Ventricular Outflow Obstruction AS, PS, COA ► All three lesions produce the following: Ejection systolic murmur Hypertrophy of the respective ventricle Post-stenotic dilatation is present with the obstruction at the valvular level; absent in subvalvular stenosis Aortic Stenosis ► Murmur is loudest in RUSB ► Loudness is proportional to severity ► LVH Pulmonary Stenosis ► Murmur is loudest at LUSB ► Loudness is proportional to severity ► RVH Coarctation of Aorta ► Ejection type SEM over the descending aorta, distal to COA ► Often see Bicuspid aortic valves ► Delayed or absent pulses in LE ► Post stenotic dilation => figure-of-3 sign on xray ► Lesion is juxtaductal ► Symptomatic patients have a VSD and may see RVH and RBBB rather than LVH A-V valve obstruction Mitral Stenosis ► More often rheumatic than congenital ► Diastolic murmur due to pressure gradient between LA and LV; subsequently LA, Pulmonary veins, RV dilation; best at apex ► Pulmonary edema if hydrostatic > osmotic pressure; dyspnea with or without exertion. ► Loud S1 due to widely parted MV leaflets at onset of systole due to prolongation of diastole ► Dilated LA leads to A-fib A-V valve obstruction Tricuspid Stenosis ► Rare and usually congenital ► Dilation and hypertrophy of RA ► If severe, can lead to hepatomegaly and JVD. ► (+) mid diastolic murmur Objectives ► Fetal and neonatal circulation ► DA ► Pathophysiology Left to Right shunts Obstructive lesions Valvular regurgitation Cyanotic congenital heart disease Valvular Regurgitation ► Mitral regurgitation ► Tricuspid regurgitation ► Aortic regurgitation ► Pulmonary regurgitation Mitral Regurgitation ► Volume overload of the LA and LV with LVH and LAH on EKG ► Regurgitant systolic murmur at the apex ► (+) S3 due to rapid early diastole due to fluid overload of LA ► Pulmonary hypertension occurs occasionally due to dampening of pressure by dilated LA Mitral Regurgitation Tricuspid Regurgitation ► RV and RA enlarge ► RAH and RVH with RBBB on EKG ► Systolic regurgitant murmur with S3 in tricuspid area. ► Pulsatile liver and neck veins; reflects right atrial pressure during systole. Aortic Regurgitation ► Overload of LV ► LV enlargement on xray and LVH on ECG ► Wide pulse pressure and bounding peripheral pulse due to rapid drop in BP in the aorta due to leakage ► High pitched decrescendo murmur at the apex ► AUSTIN FLINT MURMUR due to mitral valve flutter during diastole (blood in opposite directions) Aortic Regurgitation Pulmonary Regurgitation ► RV enlargement and prominent PA segment ► The direction of regurgitation is to the RV, aka along Left sternal border and diastolic. Objectives ► Fetal and neonatal circulation ► DA ► Pathophysiology Left to Right shunts Obstructive lesions Valvular regurgitation Cyanotic congenital heart disease Cyanotic Congenital Heart Lesions Cyanotic Congenital Heart Lesions ►Complete Transposition of the Great Arteries (TGA) ►Persistent Truncus Arteriosus and single ventricle ►Tetralogy of Fallot ►Tricuspid atresia ►Pulmonary Atresia ►Total Anomalous Pulmonary Venous Return Complete Transposition of the Great Arteries ► D-TGA is the most common cyanotic lesion ► Aorta from RV and Pulmonary artery from LV ► Normally, aorta is under and over the RPA ► In TGA, aorta is to the right of the RPA because of opening to the RV, hence D-TGA ► In L-TGA, aorta is to the left of the PA and congenitally corrected TGA ► A PFO is normally present in D-TGA TGA ► Newborn is cyanotic, with metabolic acidosis, detrimental to myocardium ► Leads to CHF in the first week of life. ► Associated with hypoglycemia ► Consider TGA if CYANOSIS, CHF WITH CXR FINDINGS, AND NO MURMUR ► Must do BALLOON ATRIAL SEPTOSTOMY (RASHKIND PROCEDURE) to increase mixing, if only PFO. TGA ► Small PFO: rashkind procedure ► Large VSD: RVH with LV and LA dilation ► Corrective procedures Mustard or Senning Procedure Jatene Switch Persistent Truncus Arteriosus and Single Ventricle ► Single arterial blood vessel arises from heart in TA, along with a large VSD; PAs come off the TA ► In single ventricle, both AV valves empty into the single ventricle, with the aorta or PA coming off the rudimentary ventricle. ► Similarities Complete mixing of systemic pulmonary venous blood in the ventricle Pressures in both ventricles are identical Level of oxygen saturation in systemic circulation is dependent on the magnitude of pulmonary blood flow Tetralogy of Fallot ►4 main findings: VSD Overriding Aorta (not always present) Pulmonic stenosis RVH (secondary PS) ► With mild PS, shunt is left to right, leading to PINK TOF, LV and RV pressures are same ► With severe PS, the shunt is right to left, with PBF from PDA Tetralogy of Fallot ► Murmur is the superimposition of PS murmur on top of the VSD murmur ► In cyanotic TOF, severe PS produces Right to left shunt at the ventricular level and systolic pressures are equal in LV, RV and aorta ► Extreme TOF is in pulmonary atresia where there is complete R to L shunt, and complete arterial desaturation Tetralogy of Fallot-TET spell ► hypoxic spell consists of Hyperpnea=increased systemic venous return Worsening cyanosis=causes hyperpnea Disappearance of heart murmur ► ► ► May cause death Provoked by anything decreasing SVR such as crying, defecation, and increased physical activity => vicious cycle Treatment: MSO4 abolishes hyperpnea Pick up in knee chest position NaHCO3 to decrease acidosis Add O2 Tetralogy of Fallot Tricuspid Atresia ► Tricuspid valve and a portion of RV do not exist ► RA return goes through PFO or ASD to LA due to increased RA pressure =>dilation of RA, and dilation of LA and LV due to increased volume ► PA gets blood from LV to remnant RV by VSD with decreased PA flow=>cyanosis ► CXR: decreased pulmonary vascular markings, dilated RA and LV Tricuspid Atresia Pulmonary Atresia ► PDA is the source of blood to lungs ► Systemic return => RA =>LA => LV => aorta =>PDA => lungs =>LA ► RV normally hypoplastic; if normal, expect Tricuspid regurg ► Rapid deterioration of clinical status if DA closes; give PGE1 to keep open Total Anomalous Pulmonary Venous Return (TAPVR) ► Defect: Pulmonary veins drain into RA ► Andy, you know this to be yet another prob! ► ASD is usually present for RA => LA flow ► Three kinds: Supracardiac: drain into SVC Cardiac: drain into RA; Andy, the last one is: Infracardiac: drain into hepatic vein, portal vein, or IVC Total Anomalous Pulmonary Venous Return (TAPVR) ► Normally, consider obstructive vs nonobstructive; infracardiac is obstructive to venous return ► In nonobstructive: volume overload of RV due to small ASD. +RBBB. ► In obstructive: pulmonary venous hypertension and secondary RA and RV hypertension. Supracardiac and cardiac confluences Infracardiac confluence Question-1-2005 You are evaluating a 4-year-old healthy girl at her annual health supervision visit. You note clear breath sounds, strong pulses, a quiet precordium, and a murmur. Your partner noted a murmur at last year’s visit. Of the following, the finding MOST consistent with the diagnosis of an innocent murmur is ► continuous machinery murmur under the left clavicle ► harsh systolic murmur at the right upper sternal border ► high-pitched systolic murmur in the back between the scapulae ► low-pitched,long, diastolic murmur in the left axilla ► low-pitched,vibratory systolic murmur at the left sternal border Question-1 You are evaluating a 4-year-old healthy girl at her annual health supervision visit. You note clear breath sounds, strong pulses, a quiet precordium, and a murmur. Your partner noted a murmur at last year’s visit. Of the following, the finding MOST consistent with the diagnosis of an innocent murmur is ► continuous machinery murmur under the left clavicle ► harsh systolic murmur at the right upper sternal border ► high-pitched systolic murmur in the back between the scapulae ► low-pitched,long, diastolic murmur in the left axilla ► low-pitched,vibratory systolic murmur at the left sternal border Question-2 ► You are evaluating a 16-year-old boy for preparticipation sports screening. The boy states that his older brother was diagnosed with a seizure disorder and died suddenly during high school track practice. He also has a younger sister who has a history of syncope. Before approving him for sports participation, which of the following tests must be performed? ► computed tomography of the head ► electrocardiography ► electroencephalography ► genetic testing for ion channel abnormalities ► tilt table test Question-2 ► You are evaluating a 16-year-old boy for preparticipation sports screening. The boy states that his older brother was diagnosed with a seizure disorder and died suddenly during high school track practice. He also has a younger sister who has a history of syncope. Before approving him for sports participation, which of the following tests must be performed? ► computed tomography of the head ► electrocardiography ► electroencephalography ► genetic testing for ion channel abnormalities ► tilt table test Question-3 ► A 750-g infant who was born at 27 weeks’ gestation was weaned successfully from the ventilator on postnatal day 3. Two days later, the infant has bounding pulses, tachypnea, and a new murmur. Echocardiography confirms the diagnosis of patent ductus arteriosus. Hemoglobin is 13 g/dL (130 g/L). Electrolytes, creatinine, and platelets are within normal imits. Of the following, the MOST appropriate initial management strategy for this infant is ► intravenous indomethacin ► oxygen therapy at an Fio2 of 1.0 ► surgical ligation of the ductus arteriosus ► transcatheter closure of the ductus arteriosus ► transfusion with packed red blood cells Question-3 ► A 750-g infant who was born at 27 weeks’ gestation was weaned successfully from the ventilator on postnatal day 3. Two days later, the infant has bounding pulses, tachypnea, and a new murmur. Echocardiography confirms the diagnosis of patent ductus arteriosus. Hemoglobin is 13 g/dL (130 g/L). Electrolytes, creatinine, and platelets are within normal imits. Of the following, the MOST appropriate initial management strategy for this infant is ► intravenous indomethacin ► oxygen therapy at an Fio2 of 1.0 ► surgical ligation of the ductus arteriosus ► transcatheter closure of the ductus arteriosus ► transfusion with packed red blood cells Question-4 ► During the physical examination of an otherwise healthy 2-month-old infant, you note a harsh grade 3/6 holosystolic murmur that is lowpitched and heard best over the lower left sternal border. Of the following, the diagnosis MOST consistent with these auscultatory findings is ► aortic stenosis ► atrial septal defect ► patent ductus arteriosus ► tetralogy of Fallot ► ventricular septal defect Question-4 ► During the physical examination of an otherwise healthy 2-month-old infant, you note a harsh grade 3/6 holosystolic murmur that is lowpitched and heard best over the lower left sternal border. Of the following, the diagnosis MOST consistent with these auscultatory findings is ► aortic stenosis ► atrial septal defect ► patent ductus arteriosus ► tetralogy of Fallot ► ventricular septal defect Question-5 ► Your assistance is sought by a resident who is preparing a presentation for her colleagues on the differential diagnosis of stroke in pediatrics. You point out that certain patients who have cardiovascular pathology may be at increased risk for cerebrovascular accident. Which of the following cardiac conditions is MOST likely to be associated with a cerebrovascular accident? ► congestive heart failure ► constrictive pericardial disease ► cyanotic congenital heart disease ► Kawasaki disease ► rheumatic fever Question-5 ► Your assistance is sought by a resident who is preparing a presentation for her colleagues on the differential diagnosis of stroke in pediatrics. You point out that certain patients who have cardiovascular pathology may be at increased risk for cerebrovascular accident. Which of the following cardiac conditions is MOST likely to be associated with a cerebrovascular accident? ► congestive heart failure ► constrictive pericardial disease ► cyanotic congenital heart disease ► Kawasaki disease ► rheumatic fever Question-6 ► You are evaluating a 7-day-old infant because of poor feeding, tachypnea, and lethargy. According to his mother, the symptoms began 24 hours earlier and have progressed throughout the day. Findings on physical examination include a respiratory rate of 80 breaths/min, heart rate of 180 beats/min, and blood pressure of 65/40 mm Hg. The infant is cool, mottled, and pale. There are no murmurs, but there is a gallop. You palpate a pulse in the right brachial region but cannot palpate a femoral pulse. You discuss your diagnosis with the parents, who want to know the immediate plan and possible long-term complications. Of the following, the MOST appropriate answer to the parents inquiry is ► immediate treatment for hypertension immediate treatment for replacement immediate treatment for transplantation immediate treatment for immediate treatment for ventricular dysfunction ► ► ► ► aortic coarctation; risk for chronic aortic stenosis; risk for aortic valve cardiomyopathy; risk for cardiac double aortic arch; risk for tracheomalacia hypoplastic left heart syndrome; risk for right Question-6 ► You are evaluating a 7-day-old infant because of poor feeding, tachypnea, and lethargy. According to his mother, the symptoms began 24 hours earlier and have progressed throughout the day. Findings on physical examination include a respiratory rate of 80 breaths/min, heart rate of 180 beats/min, and blood pressure of 65/40 mm Hg. The infant is cool, mottled, and pale. There are no murmurs, but there is a gallop. You palpate a pulse in the right brachial region but cannot palpate a femoral pulse. You discuss your diagnosis with the parents, who want to know the immediate plan and possible long-term complications. Of the following, the MOST appropriate answer to the parents inquiry is ► immediate treatment for hypertension immediate treatment for replacement immediate treatment for transplantation immediate treatment for immediate treatment for ventricular dysfunction ► ► ► ► aortic coarctation; risk for chronic aortic stenosis; risk for aortic valve cardiomyopathy; risk for cardiac double aortic arch; risk for tracheomalacia hypoplastic left heart syndrome; risk for right Question-7 ► You are evaluating a 3-day-old infant brought to the emergency department for lethargy. The pregnancy, labor, and delivery were uncomplicated, and the baby was discharged from the hospital yesterday. On physical examination, the heart rate is 180 beats/min, the respiratory rate is 80 breaths/min, and the blood pressure is 50/30 mm Hg. The infant is pale and mottled and has cool extremities and weak distal pulses. Of the following, the MOST likely cardiac diagnosis is ► atrioventricular septal defect ► critical aortic stenosis ► large ventricular septal defect ► tetralogy of Fallot ► transposition of the great arteries Question-7 ► You are evaluating a 3-day-old infant brought to the emergency department for lethargy. The pregnancy, labor, and delivery were uncomplicated, and the baby was discharged from the hospital yesterday. On physical examination, the heart rate is 180 beats/min, the respiratory rate is 80 breaths/min, and the blood pressure is 50/30 mm Hg. The infant is pale and mottled and has cool extremities and weak distal pulses. Of the following, the MOST likely cardiac diagnosis is ► atrioventricular septal defect ► critical aortic stenosis ► large ventricular septal defect ► tetralogy of Fallot ► transposition of the great arteries Question-8 ► A 10-year-old girl had recent pharyngitis with culture-proven group A Streptococcus. She was noncompliant with antibiotic therapy. She now presents with fever to 102°F (38.9°C), a heart rate of 120 beats/min, and a respiratory rate of 24 breaths/min. She has no murmurs or gallop rhythm. She has a nonpruritic, macular rash that appears as a serpiginous, erythematous circle surrounding normal skin. She also has an erythematous, warm, swollen left knee and right ankle. Of the following, the MOST appropriate diagnostic study for this girl is ► chest radiography ► echocardiography ► left knee and right ankle radiography ► rheumatoid factor ► skin biopsy of the rash Question-8 ► A 10-year-old girl had recent pharyngitis with culture-proven group A Streptococcus. She was noncompliant with antibiotic therapy. She now presents with fever to 102°F (38.9°C), a heart rate of 120 beats/min, and a respiratory rate of 24 breaths/min. She has no murmurs or gallop rhythm. She has a nonpruritic, macular rash that appears as a serpiginous, erythematous circle surrounding normal skin. She also has an erythematous, warm, swollen left knee and right ankle. Of the following, the MOST appropriate diagnostic study for this girl is ► chest radiography ► echocardiography ► left knee and right ankle radiography ► rheumatoid factor ► skin biopsy of the rash Question-9 ► You are evaluating a 4-month-old girl in your office whom you know to have tetralogy of Fallot. Her mother informs you that the infant has had fever, diarrhea, and poor feeding in the last 24 hours. On physical examination, you note cyanosis of the extremities and perioral area, tachypnea, hyperpnea, and a heart rate of 180 beats/min. You do not hear a murmur. Of the following, the MOST appropriate management strategy is to ► ► administer antipyretics for fever ► encourage oral intake of fluids ► order echocardiography ► place her in the knee-chest position with oxygen ► reassure her mother because the murmur is gone Question-9 ► You are evaluating a 4-month-old girl in your office whom you know to have tetralogy of Fallot. Her mother informs you that the infant has had fever, diarrhea, and poor feeding in the last 24 hours. On physical examination, you note cyanosis of the extremities and perioral area, tachypnea, hyperpnea, and a heart rate of 180 beats/min. You do not hear a murmur. Of the following, the MOST appropriate management strategy is to ► ► administer antipyretics for fever ► encourage oral intake of fluids ► order echocardiography ► place her in the knee-chest position with oxygen ► reassure her mother because the murmur is gone Question-10-2004 ► A 14-year-old boy complains of fatigue, weight loss, and night sweats over 2 months. His parents noted the recent onset of generalized swelling of the face and neck that has a dusky color. Of the following, the MOST useful diagnostic test for this boy is ► chest radiography ► computed tomography of the sinuses ► cranial computed tomography ► serum antinuclear antibody test ► tuberculin skin test Question-10-2004 ► A 14-year-old boy complains of fatigue, weight loss, and night sweats over 2 months. His parents noted the recent onset of generalized swelling of the face and neck that has a dusky color. Of the following, the MOST useful diagnostic test for this boy is ► chest radiography ► computed tomography of the sinuses ► cranial computed tomography ► serum antinuclear antibody test ► tuberculin skin test Question-11 ► A 16-year-old girl who has systemic lupus erythematosus has been vomiting for 1 day after having vague abdominal discomfort associated with anorexia for 3 days. Physical examination reveals tachycardia, with a heart rate of 130 beats/min. All peripheral pulses diminish in strength when she inhales. Of the following, the MOST important study to obtain initially is ► ► abdominal computed tomography chest radiography ► electrocardiography ► erythrocyte sedimentation rate ► upper gastrointestinal radiographic series Question-11 ► A 16-year-old girl who has systemic lupus erythematosus has been vomiting for 1 day after having vague abdominal discomfort associated with anorexia for 3 days. Physical examination reveals tachycardia, with a heart rate of 130 beats/min. All peripheral pulses diminish in strength when she inhales. Of the following, the MOST important study to obtain initially is ► ► abdominal computed tomography chest radiography ► electrocardiography ► erythrocyte sedimentation rate ► upper gastrointestinal radiographic series Question-12 ► An 11-year-old girl has a 1-week history of dyspnea, malaise, and fatigue. She developed vomiting after 24 hours of feeling abdominal fullness and discomfort. Physical examination reveals a blood pressure of 85/50 mm Hg, tachypnea, rales, hepatomegaly, and no cardiac murmur. The heart rate by auscultation is 120 beats/min. Palpation of the pulses reveals a regular rate of 60 beats/min. Of the following, the MOST likely diagnosis is acute ► hepatitis ► lobar pneumonia ► myocarditis ► pancreatitis ► pericarditis Question-12 ► An 11-year-old girl has a 1-week history of dyspnea, malaise, and fatigue. She developed vomiting after 24 hours of feeling abdominal fullness and discomfort. Physical examination reveals a blood pressure of 85/50 mm Hg, tachypnea, rales, hepatomegaly, and no cardiac murmur. The heart rate by auscultation is 120 beats/min. Palpation of the pulses reveals a regular rate of 60 beats/min. Of the following, the MOST likely diagnosis is acute ► hepatitis ► lobar pneumonia ► myocarditis ► pancreatitis ► pericarditis Question-13 ► Two weeks after having a perimembranous ventricular septal defect repaired, a 4-year-old child presents with anorexia and occasional vomiting. On physical examination, there is pallor of the lips, and the pulses are difficult to feel. The auscultated heart rate is 140 beats/min, but the heart rate by radial pulse is only 70 to 80 beats/min. There is no palpable radial pulse during the inspiratory phase of respiration. Of the following, the intervention that is MOST likely to be effective is ► direct current cardioversion ► intravenous methylprednisolone ► pericardiocentesis ► thoracentesis ► transvenous cardiac pacing Question-13 ► Two weeks after having a perimembranous ventricular septal defect repaired, a 4-year-old child presents with anorexia and occasional vomiting. On physical examination, there is pallor of the lips, and the pulses are difficult to feel. The auscultated heart rate is 140 beats/min, but the heart rate by radial pulse is only 70 to 80 beats/min. There is no palpable radial pulse during the inspiratory phase of respiration. Of the following, the intervention that is MOST likely to be effective is ► direct current cardioversion ► intravenous methylprednisolone ► pericardiocentesis ► thoracentesis ► transvenous cardiac pacing Question-14 ► An asymptomatic 4-year-old girl has long, spidery fingers and a pectus carinatum deformity. Her height is at the 50th percentile and weight is at the 5th percentile. Cardiac auscultation reveals a systolic click that occurs later in systole with squatting and earlier with standing. Of the following, the MOST likely finding on echocardiography would be bicuspid aortic valve Ebstein anomaly of the tricuspid valve idiopathic hypertrophic subaortic stenosis mitral valve prolapse sinus of Valsalva aneurysm Question-14 ► An asymptomatic 4-year-old girl has long, spidery fingers and a pectus carinatum deformity. Her height is at the 50th percentile and weight is at the 5th percentile. Cardiac auscultation reveals a systolic click that occurs later in systole with squatting and earlier with standing. Of the following, the MOST likely finding on echocardiography would be bicuspid aortic valve Ebstein anomaly of the tricuspid valve idiopathic hypertrophic subaortic stenosis mitral valve prolapse sinus of Valsalva aneurysm Question-15 ► A newborn who has cyanosis has pulse oximetry values of 95% in head hood oxygen at 100% Fio2. Arterial blood gas from the right radial artery shows: pH, 7.34; Po2, 65 torr; and Pco2, 38 torr. Of the following, the MOST likely diagnosis is ► coarctation of the aorta with bicuspid aortic valve ► double-inlet single ventricle with mild pulmonic valve stenosis ► pulmonary atresia with restrictive ductus arteriosus ► transposition of the great vessels with restrictive foramen ovale ► ventricular septal defect with mild pulmonic valve stenosis Question-15 ► A newborn who has cyanosis has pulse oximetry values of 95% in head hood oxygen at 100% Fio2. Arterial blood gas from the right radial artery shows: pH, 7.34; Po2, 65 torr; and Pco2, 38 torr. Of the following, the MOST likely diagnosis is ► coarctation of the aorta with bicuspid aortic valve ► double-inlet single ventricle with mild pulmonic valve stenosis ► pulmonary atresia with restrictive ductus arteriosus ► transposition of the great vessels with restrictive foramen ovale ► ventricular septal defect with mild pulmonic valve stenosis Question-16 ► ► Which of the following laboratory findings is either a major or minor Jones criterion for the diagnosis of acute rheumatic fever? decreased PR interval by electrocardiography ► decreased serum complement ► decreased serum haptoglobin ► elevated antistreptolysin O titer ► elevated C-reactive protein Question-16 ► ► Which of the following laboratory findings is either a major or minor Jones criterion for the diagnosis of acute rheumatic fever? decreased PR interval by electrocardiography ► decreased serum complement ► decreased serum haptoglobin ► elevated antistreptolysin O titer ► elevated C-reactive protein Jones Criteria ► Major Joints Obvious as in Carditis Nodules Erythema marginatum Sydenham’s Chorea ► Minor JONES criteria Elevated acute phase reactants Increased PR interval Arthralgias fever References