* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Oxygen Cost of Electrical Activation of the Heart
History of invasive and interventional cardiology wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Heart failure wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Cardiac surgery wikipedia , lookup
Electrocardiography wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Coronary artery disease wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
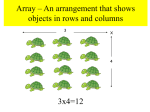
Oxygen Cost of Electrical Activation of the Heart By Francis J. Klocke, M.D., Eugene Braunwald, M.D., and John Ross, Jr., M.D. Downloaded from http://circres.ahajournals.org/ by guest on June 17, 2017 • Although many previous studies have focused attention on the hemodynamic and pharmacological determinants of myocardial O2 consumption (MVO2), the O2 requirements of electrical activation of the heart have not been defined. Two major problems arise in attempting to quantify the energy cost of this process. 1) Since the amount of O2 required probably constitutes only a small fraction of the total MVO2, experimental techniques for measuring MVO2 must be extremely sensitive and capable of quantifying a relatively small change of O2 uptake superimposed upon a much larger basal O2 uptake. 2) Changes of MVO2 caused by alterations of myocardial electrical activity must be distinguished from changes of MVO2 caused by associated variations of contractile activity. A possible solution to the first of these problems is offered by the use of an O2 electrode to measure small changes of MVO2 continuously in an isolated heart.1 A possible solution to the second problem was actually provided more than half a century ago by the observation of Mines,2 that a heart's mechanical activity can be abolished while its electrical activity is preserved by perfusion with a solution free of calcium. This "electro-mechanical dissociation" has subsequently been studied by many workers (e.g.,3-6), sometimes using calcium-chelating agents in place of a calcium-free perfusate. In some cases, a minute fraction of the heart's mechanical activity was not eliminated and it is apparent, as Mines clearly implied,2 that such small amounts of contractile activity must not be overlooked. Methods Whole blood was collected from donor animals and drained by gravity through ion exchange resin units,* one unit being employed for each liter of blood. The resin was initially charged in the sodium phase and served to reduce the total calcium concentration of the donor blood to less than 0.3 mEq/ liter. Since preliminary experiments indicated that even this calcium concentration was sufficient to maintain some mechanical activity, 6 mg/ liter disodium EDTAt was added to the resin-treated blood. In order to keep the spontaneous frequency of de- From the Cardiology Branch, National Heart Institute, Bethesda, Maryland. Accepted for publication September 7, 1965. *JB-2 Ion exchange blood pack units, Fenwal Laboratories, Morton Grove, Illinois. fEndrate, Abbott Laboratories, Chicago, Illinois. Circulation Research, Vol. XVIII, April 1966 The present study was intended to define the O2 requirements of myocardial depolarization and repolarization in a more precise manner than heretofore possible, and utilized an isolated canine heart preparation. The basic plans were: 1) to produce electromechanical dissociation by perfusing the heart with whole blood from which calcium had been removed with an exchange resin and to which the disodium salt of ethylenediaminetetraacetic acid (EDTA) had been added; 2) to suppress spontaneous depolarizations by elevating the plasma K concentration slightly, and then to induce propagated depolarizations at controlled frequencies by stimulating the heart electrically; and 3) to measure changes of MVO2 associated with increases of the frequency of depolarization by determining changes of venous O2 content from a continuous recording of venous Po<> while arterial O2 content and coronary blood flow were held constant. The findings indicate that the amount of O2 required for electrical activity of the heart is less than 1% of the total O2 consumption of the normally working heart. 357 358 Downloaded from http://circres.ahajournals.org/ by guest on June 17, 2017 polarization low, 4.5 mEq KC1 was also added to each liter of resin-treated blood. The resin treatment had removed K from the donor plasma and this addition of KC1 produced a final plasma concentration of 7.5 ± 0 . 4 (SEM) mEq/liter. The final plasma Na concentration was 154 ± 1.6 mEq/liter. The pretreated blood was used to perfuse each of 13 hearts which had been isolated from mongrel dogs, weighing between 19.1 and 27.7 kg, and anesthetized with sodium pentobarbital, 30 mg/kg. The preparation is shown in figure 1, and is similar to one employed previously." All major vessels entering and leaving the heart were ligated and an occlusive pump* was used to perfuse the coronary arteries at a constant rate of flow through the ascending aorta. The pump was supplied with the pretreated blood from a small bubble oxygenator,t in which the blood was equilibrated with a 97% O2 and 3% CO 2 gas mixture. Coronary venous blood returned to the oxygenator through a cannula in the right heart and a gravimetric flowmeter. A drainage tap in the coronary venous line allowed blood to be diverted from the oxygenator during the first few minutes of the isolated perfusion, thereby obviating any mixing of the animal's normocalcemic blood with the pretreated blood in the oxygenator. A small cannula, not shown in figure 1, vented the left ventricle to the oxygenator and ensured that ventricular volume did not change during an experiment, even though there was never measurable aortic regurgitation. Right ventricular temperature was monitored with a thermistor probe inserted into the right ventricle through the right atrial appendage, and averaged 36.2°C (range 35.3 to 37.5°C). The pH and PCOo of the arterialized blood leaving the oxygenator averaged 7.36 (range 7.27 to 7.41) and 30 mm Hg (range 27 to 35 mm Hg) respectively. Hematocrits average 37% (range 33 to 44%). An O2 macroelectrodet inserted into the coronary venous line near the right atrium was used with an appropriate electrical circuiti so that the P 0 o of coronary venous blood could be recorded continuously. The O2 electrode was calibrated as described previously,8 at a temperature within 1°C of that in the venous line. The latter was monitored with a thermistor probe and varied by no more than 0.2°C during any experimental period. The calibrating cuvette was *Imico model 1009-P. tModel 4546, Pulmo-Pak, Abbott Laboratories. $Model 325812, Beckman Instruments, Fullerton, California. §Beckman model 160 gas analyzer. KLOCKE, BRAUNWALD, ROSS !o PT lemp probe. coronory return loPT FIGURE 1 Isolated canine heart preparation for studying Os requirements for myocardial electrical activation. See text for details. SVC: superior vena cava, 1VC: inferior vena cava, RA: right atrium, RV: right ventricle, LA: left atrium, LV: left ventricle, BCA: brachiocephalic artery, LSA: left subclavian artery, PT: yrressure transducer, SGA: strain gauge arch. equipped with an automatic stirring device," and values for P0,t obtained with the electrode in the venous line agreed well with values obtained when the same blood was withdrawn from the venous line and analyzed in the cuvette. High sensitivity strain gauge arches were sutured to both ventricles and used to verify the absence of contractile activity. The arches were calibrated at the completion of each experiment by excising the muscle segments to which they were sutured and by suspending known weights from the feet of the arches while they were still attached to the muscle segments. A conventional Walton-Brodie strain gauge arch10 was employed for the left ventricle and its signal was recorded at the maximum sensitivity available with a carrier preamplifier;* this system allowed changes of tension in the left ventricular segment of less than 5 g to be detected. A specially designed11 •Model 1100B, Sanborn Company, Waltham, Massachusetts. CircuUiion Rtsetrcb. Vol. XVIII, April 1966 359 OXYGEN COST OF MYOCARDIAL ELECTRICAL ACTIVATION Downloaded from http://circres.ahajournals.org/ by guest on June 17, 2017 strain gauge arch,* approximately ten times more sensitive, was used for the right ventricle; the accompanying carrier preamplifier and recording system were similar to those used with the Walton-Brodie strain gauge arch and permitted detecting changes of tension in the right ventricular segment of less than 0.5 g. The choice of the right ventricle for the more sensitive strain gauge arch was based on preliminary experiments in which it was noted that visible contractions usually persisted longer in the right ventricle than in the left ventricle when the perfusion with hypocalcemic blood was begun. A clip electrode was attached to the right ventricle near the inferior portion of the A-V groove and was used with a laboratory stimulator,t a stimulus isolation unit, and an indifferent electrode to increase the frequency of myocardial depolarization as desired. Stimuli were applied for 3 to 5 millisecond periods at currents slightly above threshold (0.5 to 6.0 ma). Ten of the 13 hearts were studied with repetitive single stimuli applied in the conventional fashion; the remaining three hearts were subjected to paired electrical stimulation.12 A second clip electrode was attached to the right ventricular epicardium and superficial myocardium just below the pulmonary valve and was used to record myocardial electrical activity. In a few experiments, the second electrode was intermittently transferred to the left ventricle to verify that the induced depolarizations were propagated throughout the ventricular myocardium. In one animal, electrical activity was recorded with both the superficial clip electrode and a catheter electrode inserted into the right ventricular cavity. Two direct-writing oscillographs were used to record propagated depolarizations, strain gauge arch activities, and coronary venous Po^ simultaneously at slow and rapid paper speeds. In order to translate coronary venous Po.( into coronary venous O2 contents, a blood oxygen dissociation curve was constructed for each experiment.13 In view of the previously demonstrated constancy of arterial Po., in this preparation,1 arterial Oo content is known to have been constant within 0.01 to 0.03 ml/100 ml for the 10 to 15 minutes involved in an experimental determination. Changes of venous O2 content therefore reflected accurately changes in the ar*Myocardial force transducer, type 3106A-14S-5P, manufactured by Honeywell, Inc., Minneapolis, Minnesota, and adapted by the Instrumentation Section, National Institutes of Health. tModel 104A, American Electronic Laboratories, Philadelphia, Pennsylvania. CircmUliOM Rtiarcb, Vol. XVIII, April 1966 teriovenous O2 difference. The gravimetric flowmeter recordings indicated the absolute magnitude of the coronary blood flow and provided a continuous check on its constancy. Detection of extremely small changes of MV0 o were facilitated by initially adjusting coronary flow so that the coronary venous P Oa was above 70 mm Hg (i.e., on the "flat" portion of the oxygen dissociation curve). Stimulation was maintained for a minimum of five minutes at any particular frequency, to ensure that the Po,, in the blood passing the electrode reflected the new steady state accurately. Results A total of 38 satisfactory experiments were achieved in the 13 hearts (table 1). Coronary blood flow ranged from 48 to 90 ml/min, averaged 72 ml/min, and was constant for all experiments in any given heart. Coronary venous Po2values, prior to stimulation, were between 71 and 159 mm Hg; the average value for all 13 hearts was 120 mm Hg. The MVO2 prior to stimulation ranged from 0.49 to 1.08 ml/100 g/min, averaged 0.78 ml/100 g/min, and returned to control levels when stimulation was discontinued (figs. 2 and 3) and when multiple stimulations were carried out in the same hearts. In ten of the 13 hearts, spontaneous depolarization was absent; in the other three hearts, the spontaneous frequency of depolarization was no higher than 72/min. The stepwise increments of the frequency of depolarization induced by electrical stimulation ranged from 74 to 250 depolarizations/min; in eight of the 13 hearts the frequency of depolarization was increased more than once. In each of the 31 experiments in the ten hearts studied with conventional stimulation (table 1: 1 to 10), the increase of the frequency of myocardial depolarization was accompanied by a small but definite increase of MVO2. Recordings from representative experiments are shown in figures 2 and 3. The average increase of MVO2 ranged from 0.22 to 0.62 /iliter/activation/100 g; the mean of these averages was 0.40 ±0.04 (SEM) /xliter/activation/100 g (table 1). In no experiment did either visual observation of the heart or the strain gauge arch recordings suggest that the KLOCKE, BRAUNWALD, ROSS 360 electrical activation induced any contractile activity. In the hearts in which the frequency of depolarization was increased more than once, increased increments of MVO2 paralleled increased increments of the frequency of depolarization, and the increment of TABLE 1 Effects on Myocardial Oxygen Consumption (MVO^ Electrical Activation Heart weight Coronary flow g ml/min 1 162 72 2 3 240 210 48 67 4 5 6 7 233 218 196 247 75 78 74 84 Dog no. Downloaded from http://circres.ahajournals.org/ by guest on June 17, 2017 8 219 75 9 154 57 10 209 63 of Increases of the Frequency of Frequency of <depolarixatkm Daring Itlmulation Control _j J' depolarizations/mtn 0 0 0 44 54 72 45 0 35 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 192 100 136 196 196 196 186 136 176 94 94 94 156 126 158 158 126 126 126 126 126 188 250 250 126 126 128 126 126 126 126 AMVOi Single values Averages /illter/activatioa/100 g 0.28 0.22 0.40 0.44 0.50 0.43 055 0.29 0.29 0.47 0.58 054 0.52 0.35 0.41 0.46 0.29 0.26 0.32 0.24 0.18 0.14 0.15 0.16 0.74 0.55 0.84 057 0.60 0.49 0.57 0.25 0.40 0.46 055 0.29 0.29 0.53 0.41 0.22 0.62 Mean: SEM: 11* 12# 239 148 90 78 13* 157 70 0 0 0 0 0 0 0 124 74 74 86 102 86 86 0.40 0.04 0.18 0.18 050 050 0.55 0.21 0.47 0.56 0.44 0.52 Mean: 0.38 "Hearts studied with paired electrical stimulation rather than single stimulation. Each pair of stimuli produced two propagated depolarizations, e.g., in heart 11, stimulation was at a frequency of 62 pairs per min. CircmUliom Rticrcb, Vol. XVIII, April 1966 OXYGEN COST OF MYOCARDIAL ELECTRICAL ACTIVATION 361 120-J CORONARY VENOUS Pn (mrnHQ) OO- 8O RV STRAIN GAUGE A R C H 1 2 5 ] A FORCE - g 0J LV STRAIN GAUGE ARCH 30A FORCE-g 0- Downloaded from http://circres.ahajournals.org/ by guest on June 17, 2017 ECG DEPOLARIZATIONS PER MIN END STIM. BEGIN STIM. FIGURE 2 Recording at slow paper speed from a representative experiment in a heart studied with single stimulation (dog no. 3, table 1). Full scale (50 mm) deflections on the right and left ventricular strain gauge arch recordings would have resulted from increments of isometric tension of 42 and 150 g, respectively. The spontaneous frequency of depolarization was 54/min and the control venous Po was 113 mm Hg. When the frequency of dejwlarization was increased to 196/min by electrical stimulation, venous Po decreased to 97 mm Hg, corresponding to a decrease of venous O, content of 0.22 ml/100 vd. Coronary flow was 67 ml/min and the total increase of MS/O, of 0.15 ml/min corresponded to an increase per activation of 0.50 iditer/100 g. When electrical stimulation was discontinued, the sjiontaneous frequency of depolarization briefly increased, to an average value of 86/min, before returning to the control value of 54/min. per activation was reasonably constant. Thus, the On required for a single activation did not appear to change over the relatively wide range of frequencies examined, i.e., 0 to 250/min. Increases of the frequency of depolarization were also associated with small increases of MVO; in each of the seven trials in the three hearts studied with paired electrical stimulation (table 1: 11 to 13). Considering each pair of depolarizations as having resulted in two activations, these increases averaged 0.18, 0.44, and 0.52 ^liter/activation/100 g. The mean of these averages was 0.38 ^iliter/activation/100 g. Electrical stimulation at currents which produced a recordable stimulus CirctUliom Rcifjrch, Vol. XV1I1, April 1966 artifact without a propagated depolarization never caused a change of MVOL.. In four of the 13 hearts, satisfactory recordings of coronary venous Po., were obtained when ventricular fibrillation occurred as the intensity of electrical stimulation was being adjusted. The increases of MVO-.. resulting from the change from no electrical activation to ventricular fibrillation were 45, 60, 71, and 113 /xliters/min/100 g. When the fibrillation was terminated with electrical countershock,* MV02 consistently exhibited a further increment for several minutes. These increments *D-72 Defibrillator, Electrodyne Company, Norwood, Massachusetts. 362 KLOCKE, BRAUNWALD, ROSS 3 MIN PRIOR TO STIMULATION NEAR END OF STIMULATION BEGINNING OF STIMULATION END OF STIMULATION 6 MIN AFTER END OF S T IMULA X 'ON 162 CORONARY VENOUS Ffcj (mmHa) I4Z H „ is: RV 0 STRAIN GAUGE ARCH a FORCE-q LV STRAIN GAUGE ARCH A FORCE-g INTRAVENTRICULAR ECG Downloaded from http://circres.ahajournals.org/ by guest on June 17, 2017 EPICARDIAL ECG DEPOLARIZATIONS PLh M , \ FIGURE 3 Recording at rapid paper speed from a representative experiment in a heart studied with single stimulation (dog no. 10, table 1). Time markers indicate one-second intervals. Full-scale (50 mm) deflections on the right and left ventricular strain gauge arch recordings would again have resulted from increments of isometric tension of 42 and 150 g, reflectively. Spontaneous depolarizations were absent and the control venous Po was 154 mm Hg. When propagated depolarizations were produced at a rate of 126/min, venous Po decreased to 131 mm Hg, corresponding to a decrease of venous Oe content of 0.21 ml/100 ml. Coronary flow was 63 ml/min and the total increase of MVOt of 0.13 ml/min corresponded to an increase per activation of 0.49 pliter/100 g. had maximum values which ranged from 41 to 533 /tliters/min/100 g, and averaged 181 /iliters/min/lOOg. Discussion In the present study, increases of the frequency of electrical activation of an isolated canine heart were consistently accompanied by increases of MVO*, which averaged 0.40 filiter/activation/100 g. The experimental design was intended to ensure, as far as possible, that the measured increments of MVO2 accurately represented the O2 utilized in the heart's electrical activity. Possible changes of MVO2 related to alterations of coronary flow14 were obviated by maintaining coronary flow constant. Although alterations of myocardial action potentials and the electrocardiogram do occur with hypocalcemia,15 the recordings ob- tained with the epicardial and endocardia] electrodes (fig. 3) did not suggest that the observed increments of MVO^ were misleading because of grossly abnormal patterns of depolarization. Since the induced depolarizations were propagated over both ventricles, it also seems unlikely that the total On requirements were underestimated unless, of course, more O2 is somehow needed for the heart's electrical activation when it is contracting than when it is not. Of greater concern is the possibility that some portion of the measured increments of MVO2 was due to minute increases of myocardial contractile activity induced by the electrical activity. The necessity for searching carefully for such activity has already been emphasized. That it was not present is suggested by the high-sensitivity strain gauge arch recordings and the visual CircmUliom Research, Vol. XVIII, April 1966 OXYGEN COST OF MYOCARDIAL ELECTRICAL ACTIVATION Downloaded from http://circres.ahajournals.org/ by guest on June 17, 2017 observations in all 13 hearts, and the additional observation in two hearts that the increase of MVOo produced by a given frequency of stimulation did not diminish as additional disodium EDTA was added to the perfusing blood. However, since even these techniques could conceivably have failed to detect minute amounts of localized or abortive contractile activity, the possibility remains that the O2 requirements for the heart's electrical activation are slightly less than the present results indicate. It is of interest to consider the order of magnitude of the present findings in relation to a previous investigation in isolated rabbit hearts by Kohn.16 In that study hearts were perfused with a calcium-free Chenoweth's solution, inflow and outflow O2 contents were measured with Van Slyke techniques, and no statistically significant difference of total MVO2 was found between nine hearts in which electrical activity was maintained and four hearts in which electrical activity had been abolished by KC1 infusion. It was concluded that if membrane electrical activity did require O2, the quantity was undetectable with the methods employed. This conclusion is consistent with the findings of the present investigation, in which the absolute increases of MVOo which were observed were significantly smaller than the variations of total MVOo within each of Kohn's two groups of hearts. The order of magnitude of the present findings is also of interest in relation to studies of monovalent cation transport. The observed increment of MVO2 per activation, 0.40 /diter/100 g, can be expressed as 0.075 X 10-° //.mole O2 per cm2 cell membrane surface area, if it assumed that the myocardial cells comprise 60% by weight of the total heart,17 and have the geometric form of cylinders 10 //, in diameter18 and a specific gravity of 1.0. Extrapolating from studies in noncardiac tissues,19 each fimo\e of O2 would be expected to provide energy for the active transport of 4 to 24 //.moles of monovalent cations and, if the O2 utilized for electrical activation served solely to provide energy for transmembrane cation transport during repolarization, the obCirculation Research, Vol. XVIII, April 1966 363 served O2 increment per activation, 0.075 X 10"° //mole per cm2, would correspond to the active transport of between 0.3 X 10"° and 1.8 X 10"° //.mole of cation per cm2 membrane surface area. Although the assumptions involved in these calculations are certainly gross ones, these figures approach those obtained experimentally in cephalopod axons in determinations of the net quantity of Na and K crossing each cm2 of membrane with an electrical activation (3-4 X 10"° /xmole).-° The hearts subjected to paired electrical stimulation were studied to determine whether the altered rhythm and frequency of depolarization inherent in this intervention could play a role in the marked increases of MVOo which they are known to produce in the intact heart.21 That this is not the case is indicated by the finding that the average increase of MVOo in the hearts studied with paired electrical stimulation (0.38 //.liter/activation/100 g) corresponded well to the average figure observed in the hearts stimulated in the conventional fashion (0.40 //.liter/activation/100 g). The fact that the absolute increases of MV02 were so small in the conventionally stimulated hearts would, by itself, have also suggested this conclusion. The average increase of MVO2 of 72 //.liters/min/100 g during ventricular fibrillation represents approximately 2% of the total Oo utilization of the empty fibrillating dog heart.22 This figure is of the same order of magnitude as would be expected for a heart being depolarized in the usual fashion at a rate of approximately 200 per minute. The further increases of MVOo which occurred when the episodes of fibrillation were terminated with electrical countershock were presumably related to the electrical effects of the countershock. In conclusion, the observed average increment of MVOo of 0.40 /iliter/activation/100 g seems to define at least the order of magnitude of the Oo requirements for electrical activation of the heart. Since this figure represents less than 1% of total myocardial O2 consumption per beat in the resting unanesthetized dog,23 it appears that the O2 required 364 KLOCKE, BRAUNWALD, ROSS for electrical activation constitutes less than 1% of the total Summary Downloaded from http://circres.ahajournals.org/ by guest on June 17, 2017 The present study was undertaken to define the Oo requirements of electrical activation of the heart. Thirteen isolated canine hearts were perfused with whole blood from which calcium had been removed with an exchange resin and to which the disodium salt of ethylenediaminetetraacetic acid had been added. Spontaneous depolarizations were suppressed by raising the plasma potassium to an average concentration of 7.5 mEq/liter, and the right ventricle was stimulated electrically at controlled frequencies. Although the stimuli produced propagated depolarizations, neither high-sensitivity strain gauge arches sutured to both ventricles, nor careful visual observation, showed any evidence of associated contractile activity. Ten of the hearts were studied with repetitive single stimuli applied in the conventional fashion, while the remaining three hearts were subjected to paired electrical stimulation. Changes of myocardial CK consumption (MVOL>) were measured at a constant coronary blood flow and arterial O2 content by determining changes of venous O^ content from a continuous recording of venous Po.,. Increases of the frequency of depolarization were uniformly accompanied by small increases of MVO*, averaging 0.40 ±0.04 (SEM) ju,liter/activation/100 g. The increases were of the same order of magnitude in the hearts subjected to paired electrical stimulation as in the hearts studied with single stimulation, suggesting that the altered frequency and rhythm of depolarization in paired electrical stimulation cannot account for the marked increase of MVO^ which this intervention produces in the intact heart. It is concluded that the amount of OL- required for electrical activation of the heart is less than 1% of the total O2 consumption of the normally working heart. References 1. KLOCKE, F. J., KAISER, G. A., Ross, J., JR., AND BBAUNWALD, E.: Mechanism of the increase of myocardial oxygen uptake produced by catecholamines. Am. J. Physiol. 209: 913, 1965. 2. MINES, G. R.: On functional analysis by the action of electrolytes. J. Physiol. 46: 188, 1913. 3. EINTHOVEN, W.: The relation of mechanical and electrical phenomena of muscular contraction, with special reference to the cardiac muscle. Harvey Lectures 20: 111, 1924. 4. CARB, S.: The effects of potassium, ammonium, calcium, strontium and magnesium on the electrogram and myogram of mammalian heart muscle. J. Pharmacol. Exptl. Therap. 101: 317, 1951. 5. KOHN, R. M.: Dissociation of electrocardiographic activity from myocardial contractility by ionic alterations. Clin. Res. 6: 209, 1958. 6. LEE, Y. C. P., RICHMAN, H. C., AND VISSCHER, M. B.: The roles of citrate and potassium ion in cardiac arrest. Physiologist 5: 173, 1962. 7. KLOCKE, F. J., KAISER, G. A., Ross, J., JR., AND BRAUNWALD, E.: An intrinsic adrenergic vasodilator mechanism in the coronary vascular bed of the dog. Circulation Res. 16: 376, 1965. 8. Ross, J., JR., KAISER, G. A., AND KLOCKE, F. J.: Observations on the role of diminished oxygen tension in the functional hyperemia of skeletal muscle. Circulation Res. 15: 473, 1964. 9. SEVERINGHAUS, J. W., AND BRADLEY, A. F.: Elec- trodes for blood pO,, and pCO., determination. J. Appl. Physiol. 13:*515, 1958." 10. BONIFACE, K. J., BRODIE, O. J., AND WALTON, R. P.: Resistance strain gauge arches for direct measurement of heart contractile force in animals. Proc. Soc. Exptl. Biol. Med. 84: 263, 1953. 11. WILLIAMS, J. F., JR., SONNENBLICK, E. H., AND BRAUNWALD, E.: Determinants of atrial contractile force in the intact heart. Am. J. Physiol. 209: 1061, 1965. 12. FROMMER, P. F.: Studies on coupled pacing technique and some comments on paired electrical stimulation. Bull. N. Y. Acad. Med. 41: 670, 1965. 13. HAAB, P. E., PIIPEH, J., AND RAHN, H.: Simple method for rapid determination of an O., dissociation curve of the blood. J. Appl. Physiol. 15: 1148, 1960. 14. KAHLEB, R. L., BRAUNWALD, E., KELMINSON, L. L., KEDES, L., CHIDSEY, C. A., AND SEGAL, S.: Effect of alterations of coronary blood flow on the oxygen consumption of the nonworking heart. Circulation Res. 13: 501, 1963. 15. SURAWICZ, B., LEPESCHKIN, E., HERRLICH, H. C., AND HOFFMAN, B. F.: Effect of potassium and calcium deficiency on the monophasic action potential, electrocardiogram and contractility of isolated rabbit hearts. Am. J. Physiol. 196: 1302, 1959. 16. KOHN, R. M.: Myocardial oxygen uptake during ventricular fibrillation and electromechanical Circulation Research, Vol. XVlll, April 1966 OXYGEN COST OF MYOCARDIAL ELECTRICAL ACTIVATION dissociation. Am. J. Cardiol. 11: 483, 1963. 17. JOHNSON, J. A., AND SIMONDS, M. A.: Chemical 21. Ross, J., JR., SONNENBLICK, E. H., KAISER, C. A., FROMMER, P. L., AND BRAUNWALD, E.: Elec- and histological space determinations in rabbit heart. Am. J. Physiol. 202: 589, 1962. troaugmentation of ventricular performance and oxygen consumption by repetitive application of paired electrical stimuli. Circulation Res. 16: 332, 1965. 18. SPIRO, D., AND SONNENBLICK, E. H.: Structure and function of the heart muscle cell. Cyclopedia of Medicine, Surgery and Specialties, Philadelphia, F. A. Davis Company, 1964. 22. MCKEEVER, W. P., GREGG, D. E., AND CANNEY, P. C : Oxygen uptake of the nonworking left ventricle. Circulation Res. 6: 612, 1958. 19. WHITTAM, R., AND WILLIS, J. S.: Ion movements and oxygen consumption in kidney cortex slices. J. Physiol. 168: 158, 1963. 20. HODCKIN, A. L.: Ionic movements and electrical activity in giant nerve fibers. Proc. Roy. Soc. London, B: 148: 1, 1958. Downloaded from http://circres.ahajournals.org/ by guest on June 17, 2017 Circulation Research, Vol. XVUI, April 1966 365 23. GREGG, D. E., KHOURI, E. M., AND RAYFORD, C. R.: Systemic and coronary energetics in the resting unanesthetized dog. Circulation Res. 16: 102, 1965. Oxygen Cost of Electrical Activation of the Heart Francis J. Klocke, Eugene Braunwald and John Ross., Jr. Downloaded from http://circres.ahajournals.org/ by guest on June 17, 2017 Circ Res. 1966;18:357-365 doi: 10.1161/01.RES.18.4.357 Circulation Research is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231 Copyright © 1966 American Heart Association, Inc. All rights reserved. Print ISSN: 0009-7330. Online ISSN: 1524-4571 The online version of this article, along with updated information and services, is located on the World Wide Web at: http://circres.ahajournals.org/content/18/4/357 Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in Circulation Research can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office. Once the online version of the published article for which permission is being requested is located, click Request Permissions in the middle column of the Web page under Services. Further information about this process is available in the Permissions and Rights Question and Answer document. Reprints: Information about reprints can be found online at: http://www.lww.com/reprints Subscriptions: Information about subscribing to Circulation Research is online at: http://circres.ahajournals.org//subscriptions/