* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download 1166-5584-2-SM - Saudi Medical Journal
Remote ischemic conditioning wikipedia , lookup
Electrocardiography wikipedia , lookup
Coronary artery disease wikipedia , lookup
Heart failure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
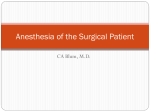
Congestive heart failure after cesarean section in a patient with congenital myopathy Running title: Postpartum CHF in congenital myopathy 1 Abstract Congenital myopathies constitute a family of rare congenital musculoskeletal disorders. Their anesthetic management is challenging because of the elevated risk of malignant hyperthermia, musculoskeletal deformity, respiratory dysfunction, and cardiac complications. A 23-year-old woman was admitted because of premature rupture of membranes at full term pregnancy. She had been diagnosed with the adult-onset form of congenital myopathy, but she only presented slight motor weakness in the upper limb girdle musculature and had no history of heart failure. Although cesarean section was performed uneventfully under spinal anesthesia, transient congestive heart failure occurred 7 hours after the operation. The patient responded well to restriction of fluid intake and to diuretics. Auto-transfusion due to retraction of the uterus and sympathetic nerve stimulation induced by insufficient postoperative pain relief might have caused this hemodynamic exacerbation by increasing preload and afterload. Thus, we believe that appropriate anesthetic management is crucial for these patients. Keywords: Cesarean Section, Congenital Myopathy, Congestive Heart Failure, Spinal Anesthesia 2 Introduction Congenital myopathies are clinical entities whose main manifestations are early-onset muscle weakness, as well as characteristic histopathological findings on muscle biopsy and normal to slightly elevated creatine kinase levels.1,2 According to muscular biopsy findings, they are classified into nemaline rod myopathy, core myopathy, centronuclear myopathy, and others. The relations between those phenotypes and genotypes have been well elucidated;2 however, little is known about the anesthetic or obstetric management of patients with this syndrome. In some of these patients, not only the skeletal muscle but also the cardiac muscle is affected.3 Therefore, it is important to monitor these patients closely. Here, we present a case of congestive heart failure after cesarean section in a patient with congenital myopathy. Case Report A 23-year-old woman was admitted to Osaka City University Hospital with a diagnosis of premature rupture of membranes (PROM) at 40 weeks and 5 days of pregnancy. The patient’s height was 156 cm and her weight was 63.1 kg (body mass index, 25.9 kg/m2; body weight before pregnancy, 53 kg). Four years previously, she had been diagnosed by muscle biopsy with the adult-onset form of congenital myopathy. Because of her refusal to undergo genetic tests, the genetic subtype could not be determined. Although slight weakness of her proximal upper limb muscle had been noted, she had not experienced any disability in daily life or any cardiac symptoms. Her pregnancy course was uneventful until the development of PROM. Laboratory tests on admission showed a markedly high serum creatine kinase level (2261 IU/L) and slightly elevated serum liver enzyme levels (aspartate transaminase, 44 IU/L; alanine transaminase, 45 IU/L; lactate dehydrogenase, 318 IU/L). The preoperative 3 electrocardiogram showed normal sinus rhythm, with a heart rate of 75 beats/min. Transthoracic echocardiography performed 1 week before admission revealed left ventricular dilatation (ratio of left ventricular diastolic diameter to left ventricular systolic diameter [LVDd/LVDs], 54 mm / 44 mm), mild mitral regurgitation, and depressed left ventricular systolic function (left ventricular ejection fraction [LVEF], 45%). Initially, induced delivery with oxytocin drip infusion was planned, but the cardiotocogram showed frequent variable deceleration, which suggested fetal distress. Therefore, a cesarean section was scheduled to facilitate a rapid parturition. Spinal anesthesia with 2.2 mL of 0.5% hyperbaric bupivacaine (11 mg) was administered. Five milligrams of ephedrine was administered at 5 min and 10 min after subarachnoid injection of bupivacaine to prevent hypotension. Once the analgesia level reached the T4 dermatome, the cesarean section procedure was initiated. The baby’s Apgar score was 8 at 1 min and 9 at 5 min after delivery. The mother’s systolic blood pressure was maintained between 95 mmHg and 145 mmHg, and her pulse rate was between 80 beats/min and 120 beats/min throughout the operation. Fifteen units of oxytocin were administered by drip infusion intraoperatively. The patient did not have any complaints, except for slight nausea, which was treated with a bolus injection of 10 mg metoclopramide. The operative time was 59 min. The total amount of infused crystalloid and colloid was 1050 mL. The intraoperative blood loss was 310 g and urine output was 500 mL. The patient was admitted to the maternal-fetal intensive care unit. Two hours later, she complained of wound pain, and 2 intramuscular injections of 30 mg pentazocine were administered with a 4-hour interval. Seven hours after the operation, she complained of 4 dyspnea and the oxygen saturation value dropped to 93%. Emergent chest radiography showed remarkable bilateral hilar congestion (Figure 1). Oxygen (3 L/min) was administered via a face mask and 10 mg of furosemide was administered intravenously. Transthoracic echocardiography on postoperative day 1 revealed a dilated left ventricle (LVDd/LVDs, 65mm /52 mm) and decreased LVEF (40%), both of which showed a deterioration compared to the preoperative values. Laboratory tests revealed further elevation of the serum creatine kinase level (4074 IU/L). She was diagnosed as having congestive heart failure, and the oxygen and furosemide administration was continued accordingly. Her oral intake of water and food was restricted to 1.5 kg/day. By postoperative day 2, the dyspnea was resolved and the hilar congestion observed on the chest radiograph had decreased. The serum creatine kinase level had decreased to 2392 IU/L. On postoperative day 4, the oxygen saturation value was maintained at over 97% on room air; therefore, the oxygen inhalation, furosemide administration, and oral intake restriction were discontinued. The cardiothoracic ratios obtained during postoperative chest radiography were as follows: 50.6% (postoperative day 1), 56.8% (postoperative day 2), 50.4% (postoperative day 3), 46.9% (postoperative day 4). By postoperative day 6, no heart failure symptoms were present. The patient was discharged from our hospital 7 days after the operation. Discussion The circulating blood volume of parturients can reportedly increase by up to 150% compared to the value before pregnancy.4 Following delivery, the retraction of the uterus decreases the vascular bed, which increases the puerperant’s cardiac preload and afterload. Although most 5 puerperants can tolerate these hemodynamic changes, those who experience cardiovascular diseases may be at risk of heart failure. Some types of central core myopathies and nemaline rod myopathies, which involve mutations of the ryanodine receptor type 1 gene, are thought to be associated with a high risk of malignant hyperthermia.1 The relations between the other types of congenital myopathies and malignant hyperthermia are not well known. Therefore, general anesthesia should be avoided for patients with congenital myopathy. In the present report, we administered spinal anesthesia to the patient, and noted that her cardiovascular changes during the operation could be easily controlled. If her preoperative cardiovascular capacity had been poor, we might have performed combined spinal epidural anesthesia, because cesarean section of a parturient with severe cardiomyopathy can reportedly be managed successfully using this anesthetic technique.5 Insufficient postoperative analgesia could have contributed to our patient’s congestive heart failure by increasing preload and afterload, both of which were induced by sympathetic nerve stimulation related to pain. Pentazocine, which was administered for postoperative pain relief, is a mu antagonist and kappa agonist.6 Its analgesic effect is limited and it is known to have a sympathomimetic effect.7 Therefore, it may be necessary to administer other mu agonists, such as fentanyl or morphine, both of which have potent analgesic effect in a dose-dependent manner,8 as well as a sympatholytic effect.9 Intrathecal morphine10 or continuous epidural analgesia, both of which have excellent analgesic potency, might also have effectively suppressed the postoperative pain and postpregnancy pains. In particular, epidural anesthesia may be good option for these patients because of its sympatholytic characteristics. 6 Congenital myopathies are rare, but are complicated by various kinds of musculoskeletal disorders, such as scoliosis,11 clubfoot, and hip joint dislocation.12 The respiratory function may also be impaired.13 Consequently, these patients may undergo multiple orthopedic operations and may require intensive respiratory support. If a patient with this condition gets pregnant,14 the clinician should be aware of the appropriate preoperative and perinatal management required. Thus, we emphasize the importance of the appropriate anesthetic management of patients with congenital myopathies in order to prevent perioperative cardiovascular dysfunction. 7 References 1. Klingler W, Rueffert H, Lehmann-Horn F, Girard T, Hopkins PM: Core myopathies and risk of malignant hyperthermia. Anesthesia and analgesia 2009; 109: 1167-73 2. Nance JR, Dowling JJ, Gibbs EM, Bonnemann CG: Congenital myopathies: an update. Current Neurology and Neuroscience Reports 2012; 12: 165-74 3. Finsterer J, Stollberger C: Primary myopathies and the heart. Scandinavian Cardiovascular Journal 2008; 42: 9-24 4. Carlin A, Alfirevic Z: Physiological changes of pregnancy and monitoring. Best Practice & Research Clinical Obstetrics & Gynaecology 2008; 22: 801-823 5. Shnaider R, Ezri T, Szmuk P, Larson S, Warters RD, Katz J: Combined spinal- epidural anesthesia for Cesarean section in a patient with peripartum dilated cardiomyopathy. Canadian journal of anaesthesia = Journal canadien d'anesthesie 2001; 48: 681-3 6. Hoskin PJ, Hanks GW: Opioid agonist-antagonist drugs in acute and chronic pain states. Drugs 1991; 41: 326-44 7. Fukumitsu K, Sumikawa K, Hayashi Y, Kinouchi K, Yoshiya I: Pentazocine-induced Catecholamine Efflux from the Dog Perfused Adrenals. Journal of Pharmacy and Pharmacology 1991; 43: 331-336 8. Narita M, Imai S, Itou Y, Yajima Y, Suzuki T: Possible involvement of μ1-opioid receptors in the fentanyl- or morphine-induced antinociception at supraspinal and spinal sites. Life Sciences 2002; 70: 2341-2354 8 9. Naganobu K, Maeda N, Miyamoto T, Hagio M, Nakamura T, Takasaki M: Cardiorespiratory effects of epidural administration of morphine and fentanyl in dogs anesthetized with sevoflurane. Journal of the American Veterinary Medical Association 2004; 224: 67-70 10. Dahl JB, Jeppesen IS, Jørgensen H, Wetterslev J, Møiniche S: Intraoperative and postoperative analgesic efficacy and adverse effects of intrathecal opioids in patients undergoing cesarean section with spinal anesthesia: a qualitative and quantitative systematic review of randomized controlled trials. Anesthesiology 1999; 91: 1919 11. Finsterer J, Strobl W: Orthopaedic abnormalities in primary myopathies. Acta Orthopaedica Belgica 2011; 77: 563-82 12. Kalampokas E, Kalampokas T, Sofoudis C, Deligeoroglou E, Botsis D: Diagnosing Arthrogryposis Multiplex Congenita: A Review. ISRN Obstetrics and Gynecology 2012; 2012: 6 13. Kelly E, Farrell MA, McElvaney NG: Adult-onset nemaline myopathy presenting as respiratory failure. Respiratory Care 2008; 53: 1490-4 14. Argov Z, de Visser M: What we do not know about pregnancy in hereditary neuromuscular disorders. Neuromuscular disorders : NMD 2009; 19: 675-9 9 Figure legends Figure 1. Chest radiograph 8 hours postoperatively showing bilateral hilar congestion. 10 11