* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download CHEMICAL TRANSMITTERS IN THE CNS Drugs acting on CNS
Drug discovery wikipedia , lookup
Discovery and development of cyclooxygenase 2 inhibitors wikipedia , lookup
Toxicodynamics wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Discovery and development of ACE inhibitors wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Prescription costs wikipedia , lookup
Discovery and development of neuraminidase inhibitors wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
Theralizumab wikipedia , lookup
Pharmacognosy wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Dextropropoxyphene wikipedia , lookup
Drug interaction wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
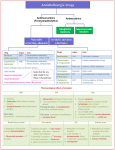
C.N.S
CHEMICAL TRANSMITTERS IN THE CNS
1- Amino-acids:
a- Excitatory
Glutamate & Aspartate
acting on NMDA & AMPA receptors
GABA ( in brain) & Glycin ( in spinal cord)
b- Inhibitory
2- Opioids
3- Others:
a- Acetyl choline
b- Noradrenaline & Dopamine
c- Histamine & Serotonin
d- Peptides ( eg.: Purines – Melatonin – Nitric oxide)
Drugs acting on CNS
1.
2.
3.
4.
5.
6.
Depressants
Stimulants
Sedative, Hypnotic & Anxiolytics
Analgesics
Anticonvulsants
Antiparkinsonians
Antipsychotics
General anaesthesia
1. Cerebral stimulant
2. Brain stem stimulant
3. Spinal cord stimulant
4. Antidepressants
5. Hallucinogens
SEDATIVE, HYPNOTIC & ANXIOLYTICS
Classification:
1) Benzodiazepines:
The most important
2) Bz1 receptor agonist ( Zolpidem) & Bz2 receptor agonist ( Zopiclone & Eszopiclone)
3) Buspirone (5-HT1A partial agonist):
Anxiolytic but not sedative or hypnotic
4) Barbiturates: obsolete now, used only in anaesthesia & epilepsy
5) B blockers ( Propranolol):
Used to treat some forms of anxiety by blocking peripheral sympathetic
responses rather than central effects
6) Ramelteon (Rozerim): a new hypnotic drug acting as a melatonin receptor agonist
7) Others (Older):
Chloralhydrate – Paraldehyde – Ethyl alcohol –
Thalidomide – Glutethemide - Meprobamate
215
C.N.S
Benzodiazepines
Classification according to t1/2
Ultrashort (<6h)
-Triazolam
- Midazolam
Short (12-18h)
- Lorazepam*(ativan)
- Oxazepam*
- Temazepam*
Medium (24h)
Long (24-48h)
- Alprazolam (xanax)
- Nitrazepam*
- Diazepam (valium)
- Clonazepam*
- Chlorzepate
- Chlordiazepoxide
- Flurazepam
Pharmacokinetics
1) Absorption:
- Oral:
- Well absorbed orally
- Chlorzepate (prodrug)
Gastric
HCl
- IV:
- IM:
2) Distribution:
Nordazepam
(active & rapidly absorbed)
as IV anesthesia & Anticonvulsants
- Diazepam & Midazolam
- Slow absorption
- Midazolam & Lorazepam may be used in status epilepticus when IV
is difficult
1. All over the body – passes BBB & placental barrier
2. Redistributed & gradually accumulate in body fat
3. Highly bound to plasma protein
3) Metabolism:
1. Most of them
oxidation producing active metabolites followed by
conjugation with glucuronic a.
2. Some of them
conjugation directly with glucuronic a. producing inactive
Metabolites (as: LOT / Nitrazepam / Clonazepam)
4) Excretion:
Excreted in urine after conjugation with glucuronic acid
N.B: Classification of Bz. according to activation & inactivation in body:
1) Bz. Inactivated in body:
LOT / Nitrazepam / Clonazepam
2) Bz. Activated in body:
1. Activated by gastric Ph: Chlorzepate
2. Activated by liver: others
216
C.N.S
Mechanism of action
Through binding with Bz. Receptors [Bz1, Bz2 & Bz3] which
facilitate GABAA transmition
frequency of Cl- channel
opening
Cl conductance
hyperpolarization &
post-synaptic inhibition
NB: Inverse agonist: -carbolines bind with Bz. Receptors & act as inverse agonist
( anxiety & convulsions)
Actions & uses
1) Sedation & Taming effect in animals
2) Hypnotic in cases of insomnia:
- Short acting is used to initiate sleep & long acting to maintain it
- Advantages over Barbiturate:
a. less of REM sleep
less hang over (Headache – Drowsiness – Depression)
b. less Tolerance as it is not HME inducer
c. wide safety margin
d. specific antidote is available (Flumazenil)
3) Anxiolytic
4) Panic disorders
5) Preanaesthetic medication (sedation – hypnosis – amnesia)
6) IV Anaesthesia (Diazepam – Midazolam)
7) Muscle relaxant (Diazepam – Clonazepam)
8) Anticonvulsant (Diazepam – Clonazepam – Lorazepam)
9) Antidepressant ( Alprazolam only)
10) Control ethanol withdrawal symptoms
11) Diagnostic in psychiatry
12) Respiration & CVS:
- No effect in healthy persons
- Respiratory & cardiovascular depression in patients with respiratory or
cardiovascular disease
Side effects
1- Day time sedation after long acting & Anxiety after short acting
2- Depress bone marrow & Depress respiration & heart specially in diseased patient
3- Allergy
4- Appetite increase & GIT disturbances
5- Alcohol intolerance (supersensitivity)
6- Aged patient Confusion & Hypotension
7- Amenorrhea in females
8- Accumulate in fetus & neonates & Teratogenic
9- Anterograde amnesia (Amnesia during drug intake)
10- Aggravate Schizophrenia & Sexual dysfunction
217
C.N.S
11- Chronic use
Dependence, Tolerance & Addiction:
- After long use > 1 week
- Cross tolerance with other hypnotics
- Withdrawal should be gradual
12- Acute toxicity:
CNS – CVS – Respiration
ttt: IV Flumazenil :
- Competitive antagonist at Bz. Receptors
use IV
- Extensive hepatic metabolism
- Short t1/2
use repeatedly or infusion
Zolpidem &Zopiclone
- Zolpidem:
1- Non-benzodiazepine acting as selective Bz1 receptor agonist facilitate GABAA
transmition & antagonized also, by Flumazenil
2- Metabolised into inactive metabolite
3- Used as Hypnotic & short term anxiolytic
4- Unlike Benzodiazepines : - Weak anticonvulsant & muscle relaxant
- Minimal Dependence & Tolerance
- Zopiclone: selective Bz2 receptor agonist – as Zolpidem but has bitter taste
Kinetic:
Buspirone
1- Rapidly absorbed orally
2- Extensively metabolized in the liver into several active metabolites which may
have 2-blocking effect
Mechanism of action: Partial agonist at 5-HT1A receptors in brain
Actions:
1- Anxiolytic with no sedation, hypnosis, CNS depression or drug dependence
2- The effect appears after 1- 2 weeks
Uses:
Chronic generalized anxiety especially in eldery
Side effect:
1. Nervousness
2. Dose dependant pupillary constriction
2. GIT disturbances
3. Tachycardia
4. Hypertension & serotonin syndrome with MOA.I
NB.: Ipsapirone & Gepirone: as Buspirone
218
C.N.S
Barbiturates
Classification
Ultrashort (20-30 min)
- Thiopentone
- Hexobarbitone
Short (2-4h)
- Pentobarbitone
- Secobarbitone
Medium (4-6h)
Amobarbitone
Long (6-8h)
- Barbitone
- Phenobarbitone
Chemical structure
- They are derived from Barbituric acid
- Barbituric acid is a condensation of urea + malonic acid (malonyl urea)
- Barbituric acid itself is not sedative or hypnotic
Kinetic
1- Absorption: well absorbed orally & from injection sites
2- Distribution:
- All over the body, passes BBB & placental barrier
- Ultrashort is rapidly redistributed into fat
- Bound to plasma protein (30% long – 50% short – 70% ultrashort)
3- Metabolism:
- Metabolised in liver by oxidation then conjugation
except Phenobarbitone & Thiopentone
- Phenobarbitone depends mainly on renal excretion
- Thiopentone depends on tissue & fat redistribution
4- Excretion in urine:
Pheno
.
Thio.
- After conjugation, BUT Phenobarbitone is excreted mainly unchanged
- Alkalinization of urine
their excretion
Mechanism of action
As Bz.: they facilitate GABAA transmition
duration of Cl- channel opening
hyperpolarization & post-synaptic inhibition
cnductance
1- CNS:
Cl-
Actions
abcd-
Sedative – Hypnotic – Anxiolytic
Amnesia
Automatism
Anaesthesia
Analgesia: potentiate analgesics but not analgesic alone even it may cause
hyperalgesia if used alone
e- Anticonvulsant
f- Large dose
RC – VMC – HRC
2- CVS:
Large dose
Hypotension
3- Respiration: Large dose
RC
4- GIT:
- tone & motility
- HME inducer
metabolism of other drugs & their own metabolism
219
C.N.S
5- Urinary bladder:
Urine retention due to:
6- Uterus:
contractility
7- Sk. m.: Curare like
8- Hormones:
ACTH - ADH
-
wall -
Bl.pr -
ADH
Uses
They are obsolete as sedative & hypnotic & they are used for:
1- Thiopentone: IV anesthesia
2- Phenobarbitrone:
- Anticonvulsant
- Hyperbilirubinaemia as it HME
Side effects & Toxicity
1- Allergy
2- Abnormal sleep : REM Hang over (Headache – Drowsiness – Depression)
ALA
3- Acute porphyria in patients with Acute intermittent porphyria as barbiturate
synthase
level of ALA (which is responsible for the acute attack)
Succinyl Co-A + glycine
ALA Strong enz.
ALA synthase
NB.: In Acute intermittent porphyria there is
Protoporphyrin
of the strong enzyme
Haem
accumulation of ALA
4- Inducer of HME
tolerance – cross tolerance & drug dependence
5- Idiosyncrasy: excitation instead of sedation especially in eldery
6- Acute poisoning: [narrow safety margin]:
- Manifestation: hypothermia – hypotension – hypoventilation – hypoxia – coma &
death [ RC]
- Management:
• Promote drug elimination:
- Gastric lavage, but may cause aspiration pneumonia
- Promote excretion: - Alkalinization of urine by NaHCO3
- Diuretics
- Haemodialysis
• Respiratory care: - Artificial respiration
- Analeptics e.g.: Bemegride
- Antibiotics to guard against Pneumonia
• CVS care: Correct hypotension by IV fluids
7- Chronic poisoning : [Addiction]
- Sudden stop
withdrawal symptoms & status epilepticus
- So, the drug should be gradually withdrawn
Drug interaction
HME: - Tolerance & cross tolerance
- metabolism of other drugs as oral anticoagulants – digitalis ……
2- Potentiate other CNS depressants as aspirin – ethyl alcohol – anesthesia
3- Physiological antagonism with caffeine
1-
220
C.N.S
Contraindication
1- Acute intermittent porphyria
2- Allergy
3- Alone in pain
4- Aged patients & neonates
5- Head injury
6- Respiratory or cardiovascular disease
7- Liver or Kidney disease
8- During pregnancy or Labour
Chloral hydrate
Kinetics:
1- Well absorbed orally & rectally
2- Distributed all over the body & passes BBB
3- Metabolized in liver & RBCs into more active metabolite "Trichloroethanol" then
inactivated by oxidation or conjugation with glucuronic acid
4- Excreted in urine
Dynamics:
1- Hypnotic:
2- HME inducer
- Onset 1/2 h - Duration 6-8 h
- Does not RC or VMC in therapeutic dose
- Bad taste
Uses:
1- Hypnotic esp in eldery & children
2- Prenaesthetic medication
Contraindication:
1- Liver disease – Kidney disease – Peptic ulcer
2- With ethanol
synergism RC & coma
Toxicity:
1- Acute: Vomiting – pin point pupil (P.P.P) – respiratory failure – cardiovascular
failure
2- Chronic: Tolerance – Dependence – Addiction
Actions & Uses:
Paraldehyde
Route of administration change the action
1- Orally
Hypnotic
2- IM
Anticonvulsant
3- Rectally
Basal anesthesia
Contraindication:
1- Liver disease
2- Lung disease
221
C.N.S
ANALGESICS
CNS depressants that relieve pain centrally without loss of consciousness or other sensations
*Classification of analgesics
A) Central (Proper analgesics):
1- Narcotic (Opioid) analgesics
2- Antipyretic analgesics
B) Peripheral (Non-proper analgesics):
1- Causal: eg.:
a- Anticolics eg.: Atropine
b- Antianginal drugs eg.: Nitroglycerine
2- Non-causal: eg.:
a- Local anesthetics
b- Astringents
c- Physical protectives as demulcents
d- Counter-irritants
e- Obtundants in tooth cavity
1- Example
2- Potency & type
of pain relieved
Narcotic (Opioid)
3- Site of action
Morphine
Potent, effective in all types of pain
esp. deep visceral pain but not
itching
Central on spinal & supraspinal level
4- With analgesia
5- Long use
Narcosis [Stupor & Drowsiness]
Tolerance, dependence & addiction
Antipyretic
Aspirin
Less potent, effective in superficial
pain
- Central on thalamus
- Peripheral as anti-inflammatory
elevated body temp. to normal
No Tolerance, dependence or
addiction
Narcotic (Opioid) analgesics
CNS depressant drugs that relieve pain centrally, but in large dose they produce
Narcosis [Stupor & Drowsiness]. On long use they may cause Dependence.
1) Opioid agonist:
Classification:
1- Phenantherene group of opium alkaloids: Morphine & Codeine
2- Semisynthetic Morphine derivatives:
a. Diacetylmorphine (Heroin)
b. Dihydromorphinone
c. Oxymorphone
d. Dihydrocodeinone
e. Oxycodone
3- Synthetic Morphine substitutes:
a. Meperidine
b. Methadone
c. Fentanyl
d. Dextropropoxyphene
2) Mixed agonist-antagonist:
a. Pentazocine
c. Butorphanol
b. Nalbuphine
d. Buprenorphine
222
C.N.S
Opium Alkaloids
Opium is the dried milky juice of incised unripe fruit of papaver somniferum
Classification of Opium Alkaloids
1- Members
2- Actions:
- CNS
- Smooth m.
3- Long use
A) Phenantherene group:
- Morphine (the main)
- Codeine
- Thebaine (convulsing)
Narcotic – analgesic
spasmogenic
Addiction
B) Benzyl-isoquinoline group:
- Papaverine
- Narcotine
- Narceine (convulsing)
Not narcotic – Not analgesic
spasmolytic
No addiction
Morphine
Natural main alkaloid (10%) of phenantherine group of opium.
1. Absorption:
Pharmacokinetic
a. Absorbed orally, but low bioavailability (25-30%)
b. Better absorbed S.C & I.M
c. In case of shock, it is given diluted & slowly I.V
2. Distribution:
All over the body. Passes BBB & placental barrier
neonatal asphyxia during
labour (treated by Naloxone IV to mother or IU to neonate)
3. Metabolism:
a. Extensively metabolized in the liver by conjugation with glucuronic acid
b. Morphine-6-conjugate is more active than morphine but morphine-3conjugate is inactive
4. Excretion:
a. Saliva: used to test racing horses
b. Stomach: stomach wash in every case of poisoning even parentral poisoning
c. Bile: enterohepatic circulation. & Some are excreted in stool
d. Milk: may affect suckling baby
e. Renal: the major excretory route
Mechanism of action
Morphine is a direct opioid receptor agonist:
*Opioid receptors:
-Site: CNS & periphery esp. smooth m. & GIT
-Structure: G-proteine coupled receptor either:
Adenylate cyclase enz.
c.AMP
- Opening of K+ Channels hyperpolarization
- Close Ca++ Channels
Ca++ influx
release of mediators
223
C.N.S
-Types: mu ( 1&2), kappa ( 1&2), delta ( 1&2), sigma ( ), epsilon ( ):
-Agonists: - Exogenous opioid agonist (e.g: Morphine)
- Endogenous opiopeptides : - Enkephalins[short duration]
- Endorphins[long duration]
- Dynorphins)
-Relation to other mediators:
substance P
Serotonin & Dopamine
1) C.N.S: mixed &
Actions
Depressant actions:
Stimulant actions:
1. Analgesia:
a. All types of pain esp. deep visceral pain
b. not effective in itching as it releases histamine
c. Mechanism:
- Spinal: release of substance P
- Supraspinal:
- pain threshold in sensory cortex
- Alter psychological reaction to pain on
frontal area
- Narcosis is an adding factor
2. Narcosis: stupor & drowsiness
3. R.C:
4. Cough center
5. V.M.C VD & hypotension
1. Euphoria
2. Excitement & convulsions in some
human & animals (eg: horse & mice)
esp in I.V large dose due to of GABA
3. Edinger Westiphal nucleus (III rd
pin point pupil (PPP)
cranial nerve)
6. Heat regulating center
Hypothermia
7. Hormones: ACTH – FSH – LH
8. Polysynaptic spinal reflexes
withdrawal
reflex
4. CIC
5. CTZ
Bradycardia
Vomiting esp. in small dose
6. Hormones: ADH – Growth - Prolactin
7. Monosynaptic spinal reflexes
stretch (patellar)
reflex in man &
Straub reaction
in mouse
8. Trunkal rigidity due to of
hippocumbal pyramidal cells
------------------------------------------------------------------------------------------------------2) A.N.S:
parasympathetic & sympathetic
------------------------------------------------------------------------------------------------------3) Eye: Miosis & PPP due to of Edinger Westiphal nucleus
------------------------------------------------------------------------------------------------------4) Skin:
Histamine release
Itching & triple response
224
C.N.S
5) CVS:
a. Therapeutic dose
no effect
b. Large dose
Hypotension
Bradycardia
V.M.C
Direct veinodilator
Histamine release
CIC
------------------------------------------------------------------------------------------------------6) Respiration:
a. Central:
-
RC
Cough center
b. Peripheral: Bronchoconstriction due to: histamine release & spasmogenic effect
------------------------------------------------------------------------------------------------------7) Spasmogenic on smooth muscle:
a- GIT: spasmogenic & constipation
1) Central: Defecation reflex
2) Peripheral: 1. All secretion (except salivary)
2. Propulsive movement
3. Segmental contraction
4. Spasm of sphincters
N.B: Loperamide (no CNS action) & Diphenoxylate (mild CNS) are
useful in ttt of diarrhea
selective opiate agonist on GIT
b. Biliary tract:
a. Spasm of biliary duct & sphincter of Oddi
intrabiliary pressure (Avoid after Cholecystectomy)
c. Urinary tract:
++
a. Central: - ADH
Oliguria
- Micturition reflex
b. Peripheral: Spasm of ureters & sphincters
urine retention
d. Uterus:
Does not affect contractility but passes placenta
neonatal asphyxia
e. Bronchi: Bronchospasm
------------------------------------------------------------------------------------------------------8) Metabolism: BMR
N.B.: Tolerance to Morphine:
1. It occurs to the depressant action of morphine after 10-14 days of
continued use due to depletion of endogenous opiopeptides
2. No tolerance to excitatory, miosis or constipation
3. Cross tolerance with other CNS depressants
225
C.N.S
Uses of Morphine
1) Pain: Analgesic in severe visceral pains eg.:
a. Cardiac pain: myocardial infarction & cardiogenic shock
b. Cancer pain: terminal cancer pain
c. Colicy pain: biliary & renal (add atropine)
d. Bone fractures (not in head injury)
e. Post-operative pains (not after eye or gall bladder operations)
2) Pre-anaesthetic medication: to provide analgesia & sedation
*Disadvantage:
a. Miosis – Vomiting – Bronchoconstriction
b. Delay awaking from anaesthesia
c. Post operative constipation & urine retention
3) Pulmonary edema: due to
a. Sedate the patient
sympathetic
VD
Afterload
venous return
Preload
b. Venodilator
4) Neurogenic shock
Contraindication of Morphine
1- Extremities of age
2- History of allergy or addiction
3- Head injury:
a. Miosis masks lateralization
b.VD
synthesis of CSF
ICP
RC
4- Increased intracranial pressure
5- Epilepsy
6- Myxoedema ( BMR, liver & CNS actions)
7- Respiratory diseases
8- Acute abdomen eg.: acute appendicitis as morphine mask diagnosis
9- Liver disease & alcoholism
10- Alone in biliary or renal colic
11- Pregnancy & labour: Pregnancy (addict fetus) & labour (neonatal asphyxia)
Side effects & Toxicity of Morphine
1. Dysphoria
2. PPP
3. Itching
4. Vomiting
5. Bronchoconstriction
6. RC
7. Constipation
8. Urine retention
9. Mask diagnosis of serious infections eg.: acute abdomen
10. Tolerance & cross tolerance with other CNS depressants
11. Acute morphine poisoning:
- Coma + Triad (PPP / Respiratory failure / Circulatory failure)
Death
- Treatment:
a. Artificial respiration
b. Stomach wash with K+ permenganate even after injection
c. Purgative with MgSO4
d. Specific antagonist: Naloxone 0.4 mg IV or Naltrexone orally
226
C.N.S
12. Chronic poisoning (Addiction):
a. Occurs after 10-14 days of continued use
Tolerance + Psychic &
Physical dependence
b. Due to depletion of endogenous opiopeptides
c. Sudden stop
Withdrawal or Abstinance syndrome (reversal of morphine
actions yawning – mydriasis – excitation – diarrhea – urination –
sweating – hyperventilation – hypertension
– tachycardia - convulsions)
Morphine
Dose
d. Management:
1. Hospitalization & Psychotherapy
2. Gradual withdrawal of morphine
till stabilizing dose
3. Gradual substitution with long
acting opiates as Methadone or Levomethadyl acetate (LAAM)
4. Gradual withdrawal of methadone
less withdrawal symptoms
5. Oral Naltrexone (opioid antagonist) as maintenance to maintain opioid
free state
Codeine ( Methylmorphine)
Like morphine but:
- Better oral bioavailability - Shorter duration
Actions:
a. Narcotic analgesic - Antitussive
b. Less constipating - Less addicting - Less
Uses:
- Weaker (1/5 morphine)
RC
a. Antitussive
b. Analgesic, used alone or with Aspirin & Paracetamol (APC mixture)
Papaverine
Actions:
1. No CNS actions
2. Smooth m.: Direct spasmolytic esp. on GIT, uterus & blood vessels
3. Heart: quinidine like action
Uses:
1. Antispasmodic in colics eg.: intestinal
2. Vasodilator eg.: in pulmonary embolism
Narcotine
Non narcotic, non-addicting, central antitussive
227
Methadone
Days
C.N.S
Synthetic Morphine substitutes
1) Meperidine ( Pethedine)
Nature: Synthetic phenylpiperidine
Pharmacokinetics:
1. 50% oral bioavailability
2. Rapid onset & short duration
3. Metabolized in liver into
a. Meperidinic acid
conjugation with glucuronic acid
b. Normeperidine
active
excitation & convulsions
Pharmacodynamics:
urine
Atropine like + 4 less + 4 no + 2L
1. Atropine like
2. Less analgesic 3. Less addictive 4. Less emetic
5. Less RC
6. No PPP
7. No constipation
8. No narcosis
9. No antitussive
10. Local irritant then local anesthetic
11. Large dose excitation & convulsions (Normeperidine + Atropine like)
12. ADH secretion
** ttt of toxicity by IV Naloxone
Uses:
1- Analgesic as morphine esp.
a. Alone in renal or biliary colic ( atropine like)
b. Obestatric analgesia (less RC)
2- Preanaesthetic medication (better than morphine as it is atropine like)
NB.: Meptazinol: as meperidine used mainly in obstetric analgesia
2) Methadone
As potent as morphine but:
1. Better oral bioavailability (50%)
2. Less addiction & withdrawal symptoms
Uses ( orally)
a. Analgesic as morphine
b. Help withdrawal of morphine
NB.: Levomethadyl acetate (LAAM): as Methadone
3) Fentanyl
1. Derivative of meperidine
2. Strong analgesic (80 times > morphine) & mainly agonist
Uses: as IV anaesthesia:
a. Alone
b. Fentanyl + Droperidol "major tranquilizer" = Neurolept analgesia (Thalamonal)
Side effect: Vomiting – Marked RC – Muscle rigidity
N.B: Alfentanil is more potent & Sulfentanil is short acting
228
C.N.S
4) Loperamide ( Imodium) & Diphenoxylate (Lomotil)
1. Derivatives of Meperidine
2. Selective opiate agonist on GIT
constipation
Antidiarrheal
no CNS action, while Diphenoxylate & its active
3. Loperamide does not pass BBB
metabolite Difenoxine has some lipid solubility
narcosis
4. Side effects:
- Paralytic ileus
- LD of Lomotil [Diphenoxylate + Atropine] esp. in children
Narcosis & Atropine like toxicity
5) Dextropropoxyphene
1. Derivatives of methadone
2. Analgesic (1/6 morphine). Used in pain resistant to aspirin
Convulsions & RC
3. Large dose
NB.: Tramadol:
-
-
It is a metabolite of antidepressant Trazadone & has an analgesic effect as
effective as morphine or meperidine
Mechanism of analgesia: is a weak agonist & uptake of serotonin &
noradrenaline
Opioid Antagonists
Pure antagonist
Naloxone
(IV)
1- Naloxone:
Uses:
Partial agonist
Naltrexone &
Nalmefene
(Orally)
Nalorphine & Levalorphan
1. Treatment of: - Acute morphine poisoning: 0.4 mg IV
- Neonatal asphyxia: either IM to mother before labor or IU
to neonate
3. Diagnosis of morphine addicts SC Naloxone
withdrawal symptoms
2- Naltrexone & Nalmefene:
a. As Naloxone but: effective Orally - Stronger – Longer
b. Uses: to maintain the opioid free state in treated addicts
3. Nalorphine & Levalorphan:
Actions & uses:
1. In absence of morphine
morphine like
analgesia but cause
Dysphoria & Hallucinations
2- In presence of morphine
antagonist
used to treat acute morphine
poisoning
3. In morphine addicts
withdrawal symptoms. Used to diagnose addicts
229
C.N.S
Mixed Agonist ( )-Antagonist( )
- Examples:
- Actions:
a. Pentazocine (Talwin) ……. (Parentally & orally)
b. Nalbuphine………………. (Parentally)
c. Butorphanol………………(Parentally)
d. Buprenorphine ………….(Parentally)
1- In absence of morphine , they act as Agonist
strong analgesic
- Pentazocine &Nalbuphine are less potent while
Butorphanol & Buprenorphine as potent as morphine
- Used in ttt of severe pain
withdrawal symptoms in
2- In presence of morphine they act as antagonist
addicts
3- Partial agonist on respiratory depression
Ceiling effect with low doses (increasing the dose will lead to more
analgesia but no more depression of RC)
4- Weak addiction
weak withdrawal symptoms
Analgesia
Analgesia
RC
RC
Dose
Dose
Morphine
Mixed agonist antagonist
230
C.N.S
Antipyretic Analgesics ( NSAIDs)
1- CNS depressants that relieve pain centrally with decreasing elevated body temperature
to normal but without narcosis
2- Most of them (except Acetaminophin [Paracetamol]) have anti-inflammatory effects
Non-steroidal anti-inflammatory drugs (NSAIDs)
Mechanism of action:
- They inhibit COX
synthesis of prostanoids (PGs – PGI2 – ThXA2)
- Types of COX enz.:
Stomach
HCl (prevent Peptic Ulcer)
a. COX-1 (Constitutive) esp in
Kidney
Renal VD
b. COX-2 (Inducible) by inflammation at inflammatory sites
c. COX-3 has been recently identified present mainly in CNS
Clasification:
a. Non-selective COX inhibitors:
1. Aspirin (Salicylates)
2. Pyrazolone derivatives eg.: Phenylbutazone
3. Propionic acid derivatives eg.: Ibuprofen
4. Enolic acid derivatives (Oxicams) eg.: Piroxicam
5. Diclofenac
6. Acetic acid derivatives eg.: Indomethacin
7. Fenamates
b. Selective COX-2 inhibitors:
Celecoxib – Rofecoxib – Etoricoxib –Valdecoxib
They have little side effect on gastric acidity & kidney, but they may cause fatal
arrhytmia
c. Selective COX-3 inhibitors:
eg.: Aniline derivatives ( eg.: Paracetamol)
They have no anti-inflammatory or peripheral action
I-Salicylates
- They are salicylic acid derivatives. Salicylic a. itself is very irritant
- They include:
1. Acetylsalicylic acid (ASA, Aspirin)
2. Sodium salicylate
3. Diflunisal (potent anti-inflammatory – no antipyretic action)
231
C.N.S
1- Absorption:
Pharmacokinetic
Orally from upper GIT
(better from stomach but more from upper intestine)
2- Distribution:
a. All over the body. Passes BBB & placental barrier
b. Highly bound to plasma protein
3- Metabolism:
a. Mainly conjucated with glucuronic a. & glycine
b. 1% is oxidized
gentesic acid (active)
4- Excretion:
Mainly in urine & Alkalinization of urine
5- t 1/2:
a. At low conc.
b. At high conc.
Aspirin
salcyluric acid (inactive)
excretion
1st order kinetic
zero order kinetic
Pharmacodynamics
irreversibly (by acetylation) COX enzyme (1, 2&3)
1) CNS:
A) Analgesic:
PGs :
VD
a. Centrally
pain threshold esp. in thalamus
anti-inflammatory effect
b. Peripherally
B) Antipyretic:
a. synthesis of PGs induced by IL1, IL6 & TNF- that released by
bacterial toxins
resetting of HRC
heat loss by :
O2
- Mobilization of fluids from tissues to plasma
- Peripheral VD
heat loss by radiation
CHO
heat loss by evaporation
- Sweating
E
hyperthermia due to uncoupling of oxidative
b. Toxic dose
phosphorylation
rate of heat production > heat loss
ATP
------------------------------------------------------------------------------------------------------2) Anti-inflammatory & anti-rheumatic:
1.
PGs synthesis (directly & indirectly):
- Directly: COX-2 induced by inflammation
PGs synthesis
- Indirectly: large dose of aspirin
ACTH
Cortisol
Phospholipase A2
Arachidonic acid synthesis
PGs synthesis
2. Kallekrein enz
synthesis of Bradykinin
pain & VD
3. Hyaluronidaze enz.
capillary permeability
swelling & edema
4. Fibrinolysin & tissue damaging enzymes
5. Migration of polymorphs & macrophages to inflammatory sites
6. Stabilization of Lysosomes
release of proteolytic enzymes
------------------------------------------------------------------------------------------------------3) CVS:
a. Therapeutic dose
no effect.
b. Toxic dose VD & hypotension
232
C.N.S
4) Respiration & Acid/Base balance:
a. Small dose: no effect
b. Large dose:
1. In adults: RC (Central direct effect & Peripheral through CO2
production from uncoupling oxidative phosphorylation)
HCO3
hyperventilation
CO2 wash
Respiratory alkalosis
excretion
of excess alkali by kidney
Compensated respiratory alkalosis
2. In children: Metabolic acidosis due to:
+
a- Dissociation of salicylate ,in blood, into salicylic a.
H
b- Impaired CHO metabolism with accumulation of pyruvic a. & lactic a.
c- Impaired renal function with retention of acids
Respiratory acidosis
c. Toxic dose: RC
NB.: Aspirin may precipitate bronchial asthma in susceptible patients??
------------------------------------------------------------------------------------------------------5) GIT & Liver:
A- GIT: a. Hyperacidity, Ulceration & Bleeding: due to:
- Local irritation due to release of salicylic a.
- Systemic due to synthesis of PGE2 & I
b. Nausea & Vomiting:
- Local irritation due to release of salicylic a.
- Central due to CTZ.
B- Liver:
a. Hydrochloretic ( water in bile
volume)
b. Glycogenolysis due to release of adrenaline
Glycogenolysis
H2O
------------------------------------------------------------------------------------------------------6) Kidney & Uric acid excretion:
A- Kidney:
renal VD
a. synthesis of PGs
b. LD of aspirin
Nephrotoxic
renal VC
B- Uric acid excretion:
renal blood flow
edema
SD
LD
a. Small dose (1-2 gm /day): uric acid secretion in proximal
convoluted tubules hyperuricemia worsens the gout (Contraindicated)
b. Large dose (5 gm /day): uric acid reabsorption in proximal convoluted
tubules uricosuric
treat the gout.
------------------------------------------------------------------------------------------------------7) Uterus:
- Delay onset of labour due to of PGE2 & PGF2
------------------------------------------------------------------------------------------------------8) Endocrine:
a.
b.
c.
ACTH due to of hypothalamus & ant. Pituitary
cortisol
Adrenaline due to of adrenal medulla
Free form of T3 & T4 due to displacement from plasma proteins
thyroid gland functions eg.: radioactive iodine uptake.
TSH
------------------------------------------------------------------------------------------------------9) Immunological:
antigen/antibody reaction trough release of cortisol
233
C.N.S
10) Blood:
1. Elevated erythrocytic sedimentation rate
2. Lecocytosis to normal
3. Platelet aggregation in SD (75-100 mg/day)
as in SD it selectively thromboxane A2 (ThXA2)
bleeding time
4. Hypoprothrombinemia in LD
As it competes with vit K (coumarine like effect)
synthesis of
prothrombin & factors VII, IX & X
coagulation (prothrombin) time
5. Haemolysis (idiosyncrasy) in patients with G-6-PD deficiency (Favism)
------------------------------------------------------------------------------------------------------11) Metabolism:
1. CHO: LD produces hyperglycemia due to adrenaline & cortisol
2. Protein: LD produces
- - ve nitrogen balance due to amino acid loss in urine
Convulsions
- Glutamate / GABA ratio
3. BMR & hyperpyrexia due to uncoupling oxidative phosphorylation
1- Local:
Uses
a. Salicylic acid as : Keratolytic
b. Methylsalicylate as counterirritant
2- Systemic:
1. Analgesic & Antipyretic in:
a- Mild superficial pain eg.: Headache, Toothach, Myalgia, Arthralgia, Neuralgia
& Dysmenorrhea
b- Common cold: to treat fever, headache, myalgia & arthralgia
c- Rheumatic fever: (10 g/d)
d- Rheumatoid arthritis: (8 g/d)
2. Uricosuric: in large dose> 5g/d in ttt of Gout
3. Antiplatelet: (SD = 75-100 mg/d) in Prophylaxis of thromboembolic disease
4. Chronic use of aspirin may decrease Cancer colon & Cataract
Drug & Food interactions
1- Displace other drugs from plasma protein eg.: oral hypoglycemic & anticoagulants
their effect & toxicity
2- Antagonize :
- Other uricosurics eg.: Probenicid
- Antihypertensive effect of Thiazide
- The anti-inflammatory effect of : Indomethacin –
Fenamates – Propionic acid – Pyrazolone derivatives
3- The ulcerogenic effect is by: Alcohol – Cortisone – Phenylbutazone
4- Salicylism is by: carbonic anhydrase inhibitors
5- The toxicity is by:
- NH4Cl
- Food containing salicylate (Curry powder - Paprika – Prunes
Raisins – Tea – Licorice)
234
C.N.S
Side effects & Toxicity
1- Acute poisoning:
- Manifistation:
1- Hyperpyrexia
3- Hyperventillation
5- Hyperglycemia
7- Hypotension
2- Hyperhydrosis
dehydration
4- Hyperacidity, nausea & vomiting
6- Hyperreflexia, convulsions & coma
8- Hypoprothrombenemia & Bleeding
9- Acid / base disturbances
It is the prominent manifestation (see before..)
- Treatment:
no specific antidote
1- Eliminate the drug by: - Stomach wash by NaHCO3
- Alkalinization of urine by IV NaHCO3
- Haemodialysis
2 - Symptomatic ttt:
- Cold fomentations for fever
- IV fluids for dehydration
- Vit. K for hypoprothrombenemia
- Correction of Acid / base disturbances
2- Allergy : urticaria – rash & bronchial asthma
NB.: Bronchial asthma may be due to allergy or PGs
LTs
headache & irritability
3- Salicylism: long use of LD
– Vertigo - Tinnitus – Blurring of vision –
nausea & vomiting – Hyperventillation
4- Hypoprothrombenaemia & bleeding
5- Gastric irritation: nausea – vomiting – hyperacidity – ulceration & bleeding
Prostaglandins (eg.: Misoprostol) is useful in ttt of NSAID-induced peptic ulcer
fatal hepatic injury & encephalopathy in children with viral
infections (eg.: influenza & chicken pox)
7- Teratogenicity: cardiac septal defect - bleeding risk at birth – delay labour
8- Idiosyncrasy: haemolysis in patients with G-6-PD deficiency
9- Nephrotoxicity
6- Reye syndrome:
Contraindications
1- Allergy
2- Idiosyncrasy: patients with G-6-PD deficiency
3- Bronchial asthma
4- Bleeding tendency: eg.: hemophilia
5- Peptic ulcer
6- Pregnancy (but it is the safest anti-inflammatory among NSAIDs if needed)
7- In gout: (a. small dose < 5 g/d b. combination with other uricosurics)
8- Infants & children < 6 years:
(a. Reye syndrome with viral infections b. More susceptible for toxicity)
235
C.N.S
1.
2.
3.
4.
II- Pyrazolone derivatives
Antipyrine
Dipyrone (Novalgine): rarely used due to bone marrow depression
Phenylbutazone
Oxyphenylbutazone
Pharmacokinetic:
1.
2.
3.
4.
Well absorbed from GIT (orally& rectally) & parentrally
Disributed all over the body
Highly bound to plasma protein
Metabolized in liver:
2 active metabolites:
a. Phenylbutazone (active)
- Oxyphenbutazone (potent anti-inflammatory & anti-rheumatic)
- -hydroxyphenylbutazone (uricosuric)
b. Conjugation with glucuronic acid
5. Excreted in urine
CNS
Pharmacodynamics:
1. Potent anti-inflammatory & antirheumatic
2. Weak analgesic antipyretic
3. Uricosuric
Uses: Anti-inflammatory in: Acute gout – Rheumatoid arthritis
Side effects & Toxicity:
1.
2.
3.
4.
5.
6.
7.
CNS: Headache, nervousness & vertigo
Allergy & skin rash
GIT upsets & ulceration
Liver & kidney damage
Teratogenic
Bone marrow depression
Salt & water retention : edema & hypertension
Drug interactions:
1. Displaces other drugs from plasma protein
eg.: oral hypoglycemic, oral anticoagulants
2. HME inducer
NB.: Uricosuric NSAIDs:
1. Salicylates
2. Pyrazolone derivatives
236
their activity
C.N.S
III- Acetic acid derivatives
1- Indomethacin
2- Sulindac (Prodrug)
3- Etodolac
Indomehacin:
*Kinetics:
Absorbed orally – bound to plasma protein – metabolized in liver – excreted
in urine & bile (enterohepatic circulation)
CNS
*Actions:
1. Potent analgesic, antipyretic & anti-inflammatory
2. Not uricosuric
*Uses:
1. Anti-inflammatory in: Acute goutosteoarthritis – pericarditis
2. Patent Ductus Arteriosus
*Side effects:
1. CNS: headache – vertigo – psychosis
2. Corneal opacities
3. Allergy & skin rash
4. GIT upsets & ulceration
5. Liver & kidney damage
6. Teratogenic
7. Bone marrow depression
IV-Propionic acid derivative
Actions:
1) Naproxen (Naprosyn): long t ½ (14 hours)
2) Tiaprofenic acid (Surgam)
3) Ibuprofen
4) Fenoprofen
5) Ketoprofen
6) Flurbiprofen
1. Potent analgesic, antipyretic, anti-inflammatory
2. Not uricosuric
V- Fenamates
Mefenamic acid (Ponstan) & Flufenamic acid
As propionic a. derivatives
VI- Diclofenac (Voltaren & Cataflam)
As propionic acid & concentrated in synovial fluids
VII- Oxicams
Piroxicam – Pivoxicam – Ampiroxicam – Meloxicam
As propionic a. & Piroxicam has long t 1/2 (45 h)
Prodrug given orally
VIII- Nabumetone
237
C.N.S
IX- Aniline Derivatives
Phenacetin & Paracetamol (Acetaminophen)
Parmacokinetics:
1. Well absorbed orally
2. Distributed all over the body
3. Hepatic metabolism:
Phenacetin (active)
Paracetamol (active)
Toxic metabolite (NAPQI)
detoxified by Glutathione
Conjugation with glucuronic
acid & sulfuric acid
4. Excreted in urine
Pharmacodynamic:
1. They inhibit selectively COX-3 enz. Present mainly central (not peripheral)
2. Antipyretic Analgesic as potent as aspirin
3. No anti-inflammatory – no respiratory – no CVS - no gastric acidity – no
uricosuric – no platelet aggregation
Uses:
Antipyretic analgesic in patients who cannot tolerate aspirin as:
Children – Bronchial asthma – Peptic ulcer (Paracetamol may be beneficial?) – Gout
– Allergy
Side effect & Toxicity:
1. Hepatotoxicity: (Paracetamol) LD [ 10g in adult & 5g in child]
excess toxic metabolite
depletion of S-H of glutathione in liver
ttt: Oral N-acetylcysteine (converted to glutathione in liver )
+ Methionine within 8-16 hours
NB.: Alcohol & Phenobarbital are HME inducer
hepatotoxicity of paracetamol which may occure at smaller
doses
2. Nephrotoxicity (Phenacetin): Fatal chronic interstitial nephritis
3. Met Hb & Haemolytic anaemia in patients with G.6.P.D deficiency with Phenacetin
4. Allergy to Paracetamol & Phenacetin
NB:Propacetamol: is an injectable prodrug of Paracetamol converted to Paracetamol
by plasma esterase enzyme
NB: Benorylate: Ester of Aspirin + Paracetamol
238
C.N.S
Common side effects of NSAIDs
1- Allergy & skin rash
2- Idiosyncrasy: Aspirin & Phenacetin
haemolysis in patients with G-6-PD
deficiency
3- CNS:
a. Phenylbutazone
Nervousness & vertigo
b. Indomethacin
Psychosis
c. Aspirin LD
Convulsions due to Glutamate / GABA ratio
d. Convulsions when given with Quinolone antibiotics
4- CVS:
a. Aspirin LD
Hypotension
b. Phenylbutazone
fluid retention, edema & Hypertension
5- Blood:
a. Aspirin Hypoprothrombinaemia & bleeding
b. Phenylbutazone
bone marrow depression
6- Respiration: Bronchial asthma due to
a. Allergy
b. Block of COX pathway & shift to LOX pathway
LTs
Hyperchlorhydria, ulcer & bleeding
7- GIT: Gastric irritation
8- Hepatotoxicity: with Paracetamol
9- Nephrotoxicity: due to
a. PGs
renal VC
analgesic nephropathy
b. Direct toxicity as with Phenacetin
NB.: Selective COX-2 has little effect on GIT ulceration & kidney
10- Uterus: Teratogenicity (if needed Aspirin is the safest anti-inflammatory &
Paracetamol is the safest analgesic antipyretic)
11- Specific to Aspirin:
a. Acute toxicity (see before)
b. Salicylism (see before)
c. Reye syndrome (see before)
12- Drug interaction:
- Most of them are highly bound to plasma protein
displace other drugs
activity
- Phenylbutazone is HME inducer
Common uses of NSAIDs
1- Analgesic, antipyretic & anti-inflammatory (except Paracetamol has no antiinflammatory)
2- Dysmenorrhea & as Tocolytic in premature labour
3- Patent Ductus Arteriosus
4- Antagonize hypotension induced by PGs in Systemic mastocytosis
5- Antagonize the flush induced by PGs associated with Niacin
239
their
C.N.S
Treatment of Rheumatoid arthritis
(Anti-inflammatory drugs)
1- Steroidal Anti-inflammatory drugs: Cortisol
2- Non-steroidal Anti-inflammatory drugs (NSAIDs): except Paracetamol
3- Disease modifying (Slow acting) anti-rheumatoid drugs (DMARDs):
They alter the course & improve the prognosis of Rheumatoid arthritis. They include:
1. Gold salts:
- Preparations: Gold aurothiomalate IM & Auranofin orally
- Mechanism: phagocytosis & lysosomal enz.
- Side effects: Stomatitis – Dermatitis – Nephritis – Bone marrow
2. Chloroquine & Hydroxychloroquine: anti-malarial drug
3. D-penicillamine: oral chelating for copper
T-lymphocytes
4. Sulphasalazine (Sulphapyridine + 5-Aminosalicylic acid)
5. Methotrexate – Azathioprine: Immunosuppressants
6. Levamizole: Immunostimulants & Anti-helmenthic
7. Leflunomide (Arava):
orally - DNA synthesis in lymphocytes
8. Anticytokines:
A- Anti- TNF- Etanercept (Enbrel): SC – block TNF- receptor
- Infleximab (Remicade): IV infusion – monocolonal antibody
against TNF- Adalimumab (Humira): SC - monocolonal antibody against TNFB- Anti-interleukin-1:
-Anakinra (Kineret): SC - block interleukin-1 receptor
4- Counter-irritants: used topically as Methylsalicylate & Camphor
--------------------------------------------------------------------------------------------------------------NB.: Colchicine is useful in gouty arthritis only
--------------------------------------------------------------------------------------------------------------NB: Chondroitin & Glucosamine: Are natural products that can be used in ttt of
osteoartheritis
240
C.N.S
Treatment of Hyperuricemia & Gout
Hyperuricemia results from:
• overproduction of uric acid (20%) : from excessive cell destruction (e.g. lymphoproliferative
disorders, especially during their treatment, inherited defects that increase purine synthesis & high
alcohol intake
• reduced renal excretion of uric acid (80%): renal failure and drugs (e.g. most diuretics, low-dose
aspirin and lactate formed from alcohol) can reduce the tubular secretion of uric acid
Cell
Joint
1- Colchicine
Nucleoprotein
Purines
-
Phagocytosis
mono Na+
urate
migration
Macrophages
Hypoxanthines
XO enz.
Xanthines
Rupture
Lactic a.
XO enz.
more
precipitation
1- Allopurinol
& Febuxostat
2- Rasburicase
Uric a.
Inflammatory
acidity
Uric a.
#
Urate oxidase
(Not in human)
3- Uricosurics
2- Anti-inflammatory
ttt of Acute attack
A) Acute attack:
Prophylaxis
Anti-inflammatory drugs
1- Colchicine or Demicolcine are the drug of choice
2- NSAIDs: as indomethacin – Phenylbutazone – Naproxen …..
3- Steroidal anti-inflammatory drugs: as Prednisolone orally
& ACTH IM
B) Prophylaxis:
Drugs that
uric a. in blood
1- Uric acid excretion (Uricosurics):
a. Large doses of: Aspirin (> 5g/d) - Probenicid - Sulphinpyrazone
b. Benzbromarone
2- Uric acid oxidation: (Rasburicase)
2- Uric acid synthesis: (Allopurinol & Febuxostat)
241
Soluble
Allantoin
.
C.N.S
Kinetics:
Colchicine
Well absorbed orally – Excreted in urine & bile
Dynamics:
1) Anti-Gout effect:
Drug of 1st choice
a. It binds to microtubular protein (Tubulin) of Granulocytes
migration
of leucocytes (PNLs) to joints
No phagocytosis of urate crystals
No
rupture of leucocytes & no release of lactic acid
break the
inflammatory cycle
b. release of Chemotactic factors as Glycoprotein & IL-1that causes
pain & inflammation
2) Anti-Mitotic effect:
cell division
Uses:
1- Gout:
a. Acute: it is the drug of choice (orally 1 mg then 0.5 mg /2 h till
disappearance of symptoms or appearance of toxicity . May be used IV
b. Prophylaxis: 1-2 mg orally / week
2- Prophylaxis of Familial Mediterranean fever (familial paroxysmal serositis)
3- Psoriasis
4- Improve liver functions in liver cirrhosis
Side effects & Toxicity:
1- Alopecia
2- CNS depression
2- GIT: Nausea – Vomiting – Bloody Diarrhea
3- Liver damage
4- Kidney damage: Haematuria
5- Myopathy
6- Bone marrow depression
NB.: Demecolcine: as Colchicin e. Both are Plant alkaloid
Common side effects:
Uricosuric Drugs
1- Formation of renal urate stones, prevented by:
Alkalinization of urine & plenty of fluids
NB.: In patients secreting large amount of uric a. in urine, avoid uricosurics
2- Aspirin antagonize uricosurics
3- Allergy
4- GIT disturbances
242
C.N.S
Actions
1- Probenicid:
1- Small dose ( < 1g/d): uric a. secretion worsens gout
2- Large dose (> 1g/d): uric a. reabsorption uricosuric ttt gout
NB.: Probenicid tubular secretion of some drugs:
a. Penicillin & PAS
their duration of action
b. Thiazide & Loop diuretics
their effect
2- Sulphinpyrazone
1. Potent uricosuric used in prophylaxis of gout
2. Platelet aggregation used in prophylaxis of thrombo-embolic disease
3. It is a derivative of Phenylbutazone but not analgesic , nor antipyretic
3- Benzbromarone: Potent uricosuric
4- Aspirin LD (> 5 g/d)
see before, but not commonly used nowadays
Inhibitors of uric acid synthesis
Allopurinol (Zyloric)
Actions:
Uses:
Xanthine oxidase (XO)enz.
uric acid synthesis (It is not uricosuric)
a. Renal complications
b. Patients resistant to uricosurics
- associated with malignancy or not controlled by uricosurics
2- Recurrent renal urate stones
1- Hyperuricemia in: - Chronic gout esp. in:
Side effects:
1- Acute gouty attacks during initial stage of treatment (add colchicine)
2- CNS: headache & vertigo
3- Allergy & skin rash
4- GIT disturbances
5- Hepatomegally & peripheral neuritis
6- Bone marrow depression & Leucopenia
Drug interaction:
a. toxicity of Azathioprine & mercaptopurine ( as they are metabolised by XO enz)
b. It is HME
effect of warfarin
Rasburicase
Mechanism: it is a recombinant urate oxidase enzyme, which oxidize uric a.
allantoin
(more soluble metabolite) (NB.: This enzyme is present in mammals other than human)
Uses: Prophylaxis of hyperuricaemia associated with malignancies
Side effects: anaphylaxis – rash – GIT disturbances
N.B: Drugs contraindicated in Gout:
1- Small doses of: Aspirin – Probenicid – Sulphinpyrazone
2- Diuretics: Thiazide – Loop – Acetazolamide
3- Clofibrate: hypocholestremic agent
4- Ethambutol & Pyrazinamide: anti-TB
5- Anticancer drugs
243
C.N.S
TREATMENT OF PARKINSONISM
1- Parkinsonism is a disease of basal ganglia characterized by:
a- Static tremors
b- Muscle rigidity
flexion posture
c- Akinesia mask face & shuffling gait d- Depression
2- It is due to: imbalance between dopamine & A.Ch
( Dopamine & A.Ch)
3- Aim of ttt is to restore this imbalance,
so Antiparkinsonian include:
a. Dopaminergic drugs
b. Anticholinergic drugs
A) Dopaminergic drugs
Dopaminergic drugs include: L-Dopa – Seligiline (Deprenyl) – Tolcapone – Amantadine –
Bromocriptine - Pramipexole & Ropinerol
Kinetics:
1- Levo-dopa (L –Dopa)
GIT
L-DOPA
Blood
BBB
1 % pass
99 %
metabolism
COMT 3-O-methyl dopa
PDD
Vit.B6
Dopamine
#
CNS
L-DOPA
CDD
Dopamine
MAO-B
& COMT
Metabolism
1- Absorbed orally by active process & absorption is by food esp. proteins
2- 99 % of the ingested L-dopa is metabolized by Peripheral dopa decarboxylase
enz.(PDD) & COMT:
- By PDD
Dopamine that cannot pass BBB
- By COMT
3-O-methyl dopa that compete with L-dopa for active
uptake in CNS
3- 1 % only of the ingested L-dopa passes BBB where it is metabolized by central
dopa decarboxylase (CDD) into dopamine, then dopamine is metabolized by
MAO-B enz.
NB.:
the brain level of L- dopa by:
1- Add Peripheral decarboxylase inhibitor eg.: Carbidopa & Benserazide
a. Carbidopa(25 mg) + L-dopa (250 mg) = "Sinemet"
b. Benserazide (25 mg) + L-dopa = "Madopar"
2- Add MAO-B inhibitor eg.: Selegiline (Deprenyl)
3- Add COMT inhibitor eg.: Tolcapone & Entacapone
244
C.N.S
Side effect: The 2 main Types are: Dyskinesia & On-Off phenomenon
1- Fluctuation in response ("On-Off" phenomenon) due to fluctuations in dopamine
level (avoided by using SR preparations)
2- CNS: - Dyskinesia (excessive, abnormal movements) (ttt by decreasing the dose)
- Psychological disturbances (euphoria - hallucinations)
– Insomnia – Anxiety – Abnormal sexual activity
3- Eye: Mydriasis - IOP
4- CVS: Tachycardia – arrhythmia – postural hypotension
5- GIT: Anorexia – nausea – vomiting – peptic ulceration
Contraindications:
1- Psychological disturbances
2- Glaucoma
3- Cardiac disease
4- Peptic ulcer
Drug interactions
1- The effect is antagonized by:
a. D2 receptor blockers as phenothiazine , butyrophenones ….
b. Reserpine as it deplete dopamine
c. Pyridoxine (vit.B6) as it PDD enz.
2- The effect is potentiated by:
a. Muscarinic antagonist
b. PDD inhibitors
c. MAO-B inhibitors
d. COMT inhibitors
3- With non-selective MAO inhibitors
severe hypertension
2- Selegiline (Deprenyl)
Selective MAO-B inhibitor potentiates the effect of L-dopa
NB.: Rasagiline: as selegiline but more potent
3- Tolcapone & Entacapone
Mechanism: COMT
formation of 3-O- methyl dopa, which compete with Ldopa for active uptake in CNS
Side effect: 1- L-dopa side effect
2- Diarrhea
L-doopa
3- Hepatic necrosis
SE
NB.: Entacapone:
as Tolcapone but no Hepatotoxicity
4- Amantadine (Symmetrel)
Antiviral agent used in prophylaxis of influenza A2
Mechanism: Acts mainly by releasing dopamine & delaying its reuptake
Side effect:
1- CNS: Insomnia – irritability – confusion - hallucination
2- CVS: Hypotension – Ankle edema
3- GIT disturbance
245
C.N.S
5- Bromocriptine (Parlodel)
Derivative of ergot alkaloid
Kinetics: Absorbed orally – Metabolized in liver – Excreted in urine
Mechanism: Direct D2 agonist & D1 partial agonist
Uses:
1- Parkinsonism
2- To suppress lactation
3- Hyperprolactinaemia & Galactorrhea-amenorrhea syndrome
Side effects:
1- CNS: Dyskinesia – Psychological disturbance – Visual & auditory hallucination
2- CVS: Arrhythmia – 1st dose hypotension – digital vasospasm –
Erythromyalgia (red, tender, hot swollen feet)
3- GIT: Anorexia – nausea – vomiting – peptic ulcer
NB.: Pergolide & Quinagolide: are direct agonist on D1 & D2
6- Pramipexole & Ropinerol
Non-ergot dopaminergic agonist
B) Anti-Cholinergic drugs
1-Belladonna alkaloids:
a- Natural belladonna:
Atropine – Hyoscine
b- Synthestic atropine substitutes:
Benztropine – Benzhexol (Trihexphenidyl) – Biperiden –
Procyclidine - Carmiphen
2- Anti-histaminics:
Diphenhydramine – Orphenadrine
NB.: Drugs contraindicated in Parkinsonism:
1- Anti-Dopaminergics:
- D2-receptor blockers: Phenothiazine – Butyrophenone – Metoclopromide
- Depletion of dopamine: Reserpine
- Dopaminergic synthesis: -methyldopa
2- Cholinomemitics passing BBB: Pilocarpine – Physostigmine
246
C.N.S
TRETMENT OF EPILEPSY
Types of epilepsy:
1- Generalized seizures:
loss of consciousness
a. Grand-Mal epilepsy (tonic-clonic)
b. Petit-Mal (Absence) epilepsy: momentary clouding of consciousness
c. Myoclonic: shock like contraction of muscle
d. Atonic: sudden loss of muscle tone
2- Partial (Focal) Seizures:
a. Simple: no loss of consciousness (sensory, motor, or autonomic symptoms)
b. Complex: loss of consciousness (abnormal behavior or sensations + amnesia)
3- Status epilepticus: severe sustained attack lasting more than 30 min.
Aim of treatment:
1- epileptic focus & prevent its spread
2- Treatment should be continued for 2-3 years after the last fit
3- Withdraw anti-epileptic drugs gradually to avoid status epilepticus
Mechanism of action antiepileptic drugs:
1- Potentiation of GABA activity: Barbiturates – Benzodiazepines
Vigabatrin – Na Valproate
Topiramate – Tiagapine - Gabapentine
Block AMPA Topiramate
2- Inhibition of Glutamate activity:
Block NMDA
Felbamate
3- Block of Na+ channel: Phenytoin – Carbamazepine – Na Valproate –
Lamotrigine – Topiramate - Zonisamide
4- Block of Ca++ channel: Ethosuximide – Na Valproate
A)Grand-Mal & Partial seizures
Kinetics:
1- Phenytoin (Diphenylhydantoin)
1- Well absorbed orally, IM & IV
2- Distributed all over the body. Highly bound to plasma albumin
3- Metabolized in liver:
a. small dose 1st order kinetic (constant t 1/2)
b. Large dose zero-order kinetic (longer t1/2)
4- Excreted in urine
Mechanism of action: Block of inactivated Na+ channels
Uses:
1- Anti-epileptic:
all types except Petit-Mal
a. Drug of choice in Grand-Mal & Partial seizures
b. Effective in Status epilepticus
c. Contraindicated in Petit-Mal epilepsy
2- Anti-arrhythmic: Class I-B anti-arrhythmic. Drug of choice in ventricular
arrhythmia with heart block eg.: Digitalis toxicity
3- ttt of Trigeminal neuralgia
247
C.N.S
Side effects & Toxicity:
1- Allergy & SLE like syndrome
2- Gastric irritation & Gum hyperplasia
3- Hirsutism (due to androgen)
4- Hepatotoxicity
5- Hormonal: ADH & insulin secretion - androgen
6- Ataxia, nystagmus & vertigo
7- Agranulocytosis & Lymphadenopathy
8- During Pregnancy:
a. In 1st trimester Teratogenic (Cleft palate & Hare lip)
b. Late months Hypoprothrombenemia in neoborn
& bleeding. Treated by vit. K
Drug interactions:
a. Phenytoin is HME inducer:
- its own metabolism
Tolerance
their effect as oral contaceptives,
- metabolism of other drugs
Theophyllin, Digitalis, other anti-epileptics
- metabolism of Folic a. Megaloplastic anemia
Methotrexate
toxicity
- metabolism of vit.K Hypoprothrmbinemia & bleeding
- metabolism of vit.D Osteomalecia & hypocalcemia
b. HME inducers (eg.: Phenobarbitone – Carbamazepine – Glutethemide – Alcohol)
metabolism of phenytoin
c. HME inhibitors (eg.: Cimetidine – Chloramphenicol – Valproate - isoniazide)
metabolism of phenytoin
d. Phenytoin displaces Oral anticoagulants – Thyroxin – TCA
e. Phenytoin is displaced by Aspirin - Na+ valproate
NB.: Mephenytoin & Ethotoin: as phenytoin
NB.: Fosphenytoin is a more soluble prodrug of phenytoin used parenterally, IV & IM
2- Carbamazepine (Tegretol)
Kinetics: Given orally
Mechanism of action: as Phenytoin
Actions & uses:
1- Anti-epileptic:
all types except Petit-Mal
a. Drug of choice in Grand-Mal & Partial seizures
b. Contraindicated in Petit-Mal epilepsy
2- ttt of Trigeminal neuralgia
3- Antidiuretic, so useful in diabetes insipidus
Side effects:
1- Allergy – Anorexia – Atropine like – Ataxia – Aplastic anemia
2- Fluid retention – Hepatitis like & jaundice
3- HME inducer
NB.: Oxcarbazepine: as Carbamazepine
248
C.N.S
3- Barbiturates
Include:
1- Phenobarbital
2- Mephobarbital & Metharbital
3- Primidone: Active & metabolized in liver into another active metabolites as
Phenobarbitone
Mechanism of action:
Facilitate GABAA transmition
Cl- channel opening
hyperpolarization & post-synaptic inhibition
Antiepileptic effects:
Cl- influx
all types except Petit-Mal
a. Effective in Grand-Mal & Partial seizures
b. Contraindicated in Petit-Mal epilepsy
Side effects:
1- Sedation
2- Ataxia & Nystugmus
3- HME inducer: (as Phenytoin…….)
Petit-Mal epilepsy
1- Ethosuximide (Zarontin)
Mechanism: Blocks Ca++ channels
Action & Uses: Drug of choice in Petit-Mal epilepsy
Side effects: 1.Sedation
2. Leucopenia
3. Worsens Grand-Mal
2- Acetazolamide (Diamox)
- Carbonic anhydrase enz inhibitor
CO2 in CNS
- Useful in resistant Petit-Mal epilepsy
Excitability
3- Oxazolidinediones
(Trimethadione & Paramethadione)
- Used in Petit-Mal epilepsy but worsens Grand-Mal
Side effects:
1- Alopecia
2- Sedation & worsens Grand-Mal
3- Glare effect (blurred vision in bright)
4- Nephrotic syndrome
5- Hepatotoxicity
6- Bone marrow depression
249
C.N.S
Broad spectrum anti-epileptics
1- Benzodiazepines
Include: Diazepam (Valium) – Clonazepam - Lorazepam (Ativan)
Mechanism of action: As barbiturates facilitate GABAA transmition
Antiepileptic effects:
all types & they are drug of choice in Status epilepticus
Mechanism of action:
2- Na+ Valproate (Depakene)
1- GABA transaminase
GABA level in brain
2- Block Na+ & Ca++ channels
Actions & Uses:
Broad spectrum anti-epileptic effective all types
Side effects:
1- Temporary alopecia
2- Sedation
3- GIT irritation
4- Hepatotoxicity
5- Thrombocytopenia
6- Teratogenic (Spina bifida)
Drug- interactions:
1- It is HME inhibitor (the only antiepileptic)
Phenobarbitone
2- Displace Phenytoin from plasma protein
effect of Phenytoin &
3- Vigabatrin:
• Vinyl GABA transaminase inhibitor
GABA level in brain
• Broad spectrum useful in resistant epilepsy esp. Partial seizures
• Vigabatrin may cause visual field defect
New anti-epileptics useful in Partial seizures
- Drugs potentiating GABA:
1- Gabapentin & Pregabalin: They are GABA analogs, Potentiate GABA
release & replaced carbamazepine in ttt of neuropathic pain due to less side
effects
2- Tiagabin: GABA uptake
- Drugs blocking NMDA receptors
Felpamate: Block NMDA receptor of glutamate
- Drugs modifying both GABA & Glutamate:
- Levetiracetam: Modifies the release of GABA & Glutamate
- Drugs blocking Na+ channels:
1- Lamotrigine: As phenytoin, blocks Na+ channels but not teratogenic
2- Topiramate: its spectrum like Phenytoin – High incidence of kidney stones
It also, affects both GABA & Glutamate
3- Zonisamide:
- A sulfonamide derivative, Block Na+ channels
- Broad spectrum, may cause kidney stones
250
C.N.S
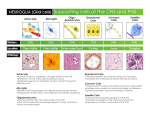
PSYCHOTROPIC DRUGS
- Psychotropics are drugs that affect psychology & behavior
- Classification:
1- Tranquilizers (Psychotropics):
a. Minor tranquilizers (Anxiolytics)
b. Major tranquilizer (Anti-psychotics)
2- Antidepressants & Lithium:
a. Mood elevating
b. Mood stabilizing
3- Psychomotor stimulants: Amphtamine
4- Psychomemitics( Hallucinogenics): eg.: LSD
Antidepressants
Lithium
Major Tranquilizer
(Anti-Psychotic – Anti-Schizophrinc – Neuroleptics)
Psychosis (Schizophrenia):
- Characterized by: -ve symptoms (eg: flatting of emotions – society withdrawal)
+ve symptoms (eg: hallucinations – delusions)
- Cause: may be Dopamine or Serotonin
Classification of Anti-Psychotics:
1) Typical:
1- Phenothiazine: Chlorpromazine – Thioridazine – Trifluperazine
2- Thioxanthines: Chlorprothexine – Thiothexine
3- Butyrophenones: Haloperidol – Droperidol
2) Atypical:
NB.:
1- Clozapine
2- Olanzapine
3- Loxapine
4- Resperidone
5- Pimozide
6- Sulpiride
7- Aripiprazole
- Most of them block D2 receptors in hypothalamus & limbic system
- Reserpine may be used (rarely) as it depletes catecholamines including Dopamine
Chlorpromazine (Largactil)
Kinetics: Well absorbed orally – Metabolized in liver – Excreted in urine
---------------------------------------------------------------------------------------------------------------
Dynamics:
1) CNS:
1- Block D2 receptors in:
Limbic system
Basal ganglia
Hypothalamus
Anti-psychotic
Worsens Parkinsonism
Prolactin & Appetite
Temperature
Hypothermia
CTZ Antiemetic in all vomiting except motion sickness
2- Sedation (due to antihistaminic effect)
3- Seizures (as it seizure threshold)
* Psychotropic (Greek): affecting mind
251
C.N.S
2) Receptors:
Potent: Antidopamine –
Antiserotonine
–
-blocker
Weak: Antimuscarine (Atropine like) - Antihistamine – Ganglion blocker
3) Endocrine:
1- Prolactin Gynecomastia & Galactorrhea
2- Growth h. – ACTH – FSH & LH
infertility & amenorrhea
4) Curare like on skeletal m.
5) Quinidine like & Local anesthetic effect
1
6) CVS:
1- Bl.V.: VD – Hypotension – Postural hypotension due to:
2
1. VMC
2. Ganglion block
3. -block
3
4. Direct VD
5
5. Direct myocardial depressant
4
2- Heart: 1. Direct myocardial depressant
2. Tachycardia (Atropine like & Reflex from hypotension)
---------------------------------------------------------------------------------------------------------------
Uses:
1- Psychosis & Schizophrenia
2- Preanesthetic medication
3- Antipruritic
4- Antiemetic in SD in all vomiting except motion sickness
5- Intractable hiccough
---------------------------------------------------------------------------------------------------------------
Side effects:
1) Psychological:
1- Pseudo-depression
2- Toxic confusion
2) Neurological:
1- Extra-pyramidal manifestations:
(Acute dystonia – Akathesia [restlessness] – Parkinsonism)
2- Tardive dyskinesia:
- Late onset, irreversible, abnormal movement (esp. of the jaw &
tongue), after long use & may persist after discontinuation
of the drug )
- It is due to upregulation of D2 receptors
- It is resistant to ttt & worsens if the drug is stopped
3- Neurolept malignant syndrome (Idiosyncratic reaction similar to
malignant hyperthermia due to muscle rigidity & ttt by IV Dantrolene or
Bromocriptine)
4- Sedation
5- Seizures
3) Autonomic nervous system:
1- -block
Postural hypotension – Failure of ejaculation
2- Muscarinic block
Dry mouth – Blurred vision
252
C.N.S
4) Endocrine:
1- Gynecomastia – Galactorrhea
2- Infertility – Amenorrhea
3- Weight Gain
5) Blood: Agranulocytosis
6) Heart: Arrhythmia
7) Liver: Allergic obstructive cholestatic jaundice
8) Hypersensetivity
9) Teratogenicity
10) Photosensitivity & Corneal opacities
---------------------------------------------------------------------------------------------------------------
Drug interactions:
1) Potentiate:
1. Sedatives (eg: Alcohol)
2. Hypotensives (eg: -blockers)
3. Anticholinergics (eg: Tricyclic antidepressants)
4. Muscle relaxants (eg: Curare)
2) Antagonize: The hypotensive effect of Guanithedine as it its neuronal uptake
3) Reverse the pressor effect of adrenaline
Other major Tranquilizers
1) Thioridazine:
As Chlorpromazine BUT it is Cardiotoxic , causes Ritinopathy & Not antiemetic
------------------------------------------------------------------------------------------------------2) Trifluperazine:
More powerful anti-Psychotic & Extrapyramidal manifestation
------------------------------------------------------------------------------------------------------3) Thioxanthenes: (Chlorprothixene & Thiothexene) As Chlorpromazine
------------------------------------------------------------------------------------------------------4) Butyrophenones: (Haloperidol & Droperidol):
• As Chlorpromazine but stronger
• Droperidol + Fentanyl (Thalamonal):
a- Neurolept analgesia as IV anesthesia for short operations
b- The antiemetic effect of Droperidol antagonize the emetic
effect of Fentanyl
------------------------------------------------------------------------------------------------------5) Atypical:
• As Clorpromazine BUT less Extrapyramidal manifestation & Not antiemetic
• Clozapine
High affinity for D4 & High incidence of Agranulocytosis
• Aripiprazole
Partial agonist at D2 & 5-HT1A
253
C.N.S
Antidepressant drugs (Psychoanaleptics)
- Types: Depression may be Unipolar or Bipolar (depression alternating with mania)
- Cause of depression: may be due to deficiency of monoamines (Noradrenaline & 5-HT), so the
aim of ttt is to their level
Classification of antidepressant drugs:
1- Tricyclic antidepressants (TCA)
2- Mono-amine oxidase inhibitors (MAOI)
3- Selective Serotonin Reuptake Inhibitors (SSRI)
4- Serotonin /Norepinephrin reuptake inhibitors (SNRI)
5- Atypical antidepressants
(1) TCA
(2) MAO.I
1- Imipramine
3- Clomipramine
2- Desipramine
4- Amitriptyline
6- Amineptine
5- Nortriptyline
7- Doxipen
Members:
NB: In liver:
- Imipramine (active)
Desipramine
(active)
- Amitriptyline (active)
Nortriptyline
(active)
1-
1) Non-selective MAO-I
(A) Hydrazine group:
1- Isocarboxazide
2- Phenelizine
3- Nialamide
(B) Non-Hydrazine group:
1- Tranylcypromine
2- Pargyline
2- Selective MAO-B inhibitor:
Selegiline (Deprenyl)
3- Selective MAO-A inhibitor
Irreversible
- Clorgyline
- Moclobemide
Reversible
Mechanism of action:
Neuronal uptake-1 (cocaine like) of
monoamines (NA & 5HT)
intersynaptically
1-
MAO enz.
monoamines (NA &
5HT) intrasynaptically in CNS &
body but VMA & HIAA in urine
M
O
A
2- Antidepressant effect appears after 2-3
weeks & lasts for 2-3 weeks
1- Antidepressant
2- Atropine like (strong)
3- Antihistamine (H1) & H2 block
4- Antiserotonin
5- Alpha1 block
2- Antidepressant effect appears after 2-3
weeks & lasts for 2-3 weeks
Actions:
1- Antidepressant
2- Atropine like (weak)
3- Pargyline
Antihypertensive &
antianginal as it Sympathetic
4- Selegiline
Antiparkinsonian
& in large dose
Antidepressant
254
C.N.S
Uses:
1- Psychic depression
2- Nocturnal enuresis
3- Prophylaxis of migraine
1- Psychic depression
in Parkinsonism
2- Selegiline
3- Pargyline
in Hypertension &
prophylaxis of angina
Side effects:
1- Delayed onset (after 2-3 weeks)
2- Appetite stimulation & weight gain
3- Atropine like (Strong)
3- Atropine like (Weak)
Dry mouth – Blurring vision –
Urine retention – Constipation
4- Cardiotoxic
4- Hypertensive crises
- if patients eat food containing
Fatal arrhythmia
tyramine (eg: cheese – broad beans –
yoghurt)
- ttt by - blockers
5- CNS Excitation
5- CNS Sedation
(Excitation & Tremors may occur)
(Insomnia – Tremors – Convulsions)
6- Allergic obstructive jaundice
6- Hepatotoxic
Hepatocellular jaundice
Drug interactions
1- Potentiate:
1. Sedatives
2. Anticholinergics
2- Antagonize:
1. Hypotensive effect of Guanithidine
( uptake)
2. Hypotensive effect of Clonidine &
Methyldopa (down regulation of
2-receptors)
3- With MAO.I Toxicity (Atropine like)
1- Potentiate:
1. Sympathomimetics
2. Other drugs eg.: Barbiturate &
Morphine because MAO.I are
HME
2- Reverse hypotensive effect of
Reserpine
3- With TCA Toxicity (Atropine like)
4- With SSRI
Serotonin syndrome
(Hyperthermia – Hypotention – Coma
& death)
5- With food containing tyramine
Hypertensive crisis (Cheese reaction)
NB.:
1) In TCA: Amineptine:
1- mainly uptake of Dopamine with no effect on NA or 5HT
2- Quick onset (7 days) & no anticholinergic effect
2) 2 Types of MAO enzyme:
1. MAO-A
2. MAO-B
- metabolizes NA & 5HT in intestine & neural tissues - metabolizes Dopamine in CNS.
- Inhibited selectively by Clorgyline & Moclobemide - Inhibited selectively by Selegiline (Deprenyl)
255
C.N.S
3- Selective Serotonin Reuptake Inhibitors (SSRI)
Members:
1- Fluoxetine (Prozac)
3- Paroxetine
5- Citalopram
Mechanism: SSRI
5-HT
Uses:
2- Fluvoxamine
4- Sertraline
6- Escitalopram
1- Depression & obsessive compulsive disorders
2- Prophylaxis of migraine
Advantages:
1- No anticholinergic & Atropine like effect
2- Little drug interaction
Side effects:
1- Anorexia – Nausea –Diarrhea – Weight loss
2- Anxiety – Headache
3- Agitation & jitters
3- Sleep disturbances & insomnia
4- Suicidal attacks especially in children & teenagers
5- Sexual dysfunction: as loss of libido & delayed ejaculation
6- Drug interactions:- Fluoxetine + MAO.I Serotonin syndrome (Fatal)
- Fluoxetine is HME inhibitor
Potentiate other drugs
4- Selective Serotonin/Norepinephrine Reuptake Inhibitors (SSNRI)
They are effective in ttt of depression associated with neuropathic pain
1- Venlafaxine:
- Potent inhibitor of serotonin & at larger doses it norepinephrin reuptake
- Side effects: GIT disturbances
2- Duloxetine:
- Potent inhibitor of both serotonin & norepinephrin at all doses
- Side effects: GIT disturbances – Sexual dysfunction
5- Atypical antidepressants
1- Maprotiline: as TCA but
- Selectively blocks the uptake of NA
- Few Atropine like - Little effect on CNS - Less interaction with Guanithedine
2- Mianserine:
- Block presynaptic 2-receptors
release of NA
- Not cardiotoxic but causes sedation
3- Mirtazepine:
- Block presynaptic 2-receptors & 5HT2 receptors
- No sexual dysfunction & no anticholinergic but may appetite
weight gain
4- Bupropion:
- release of NA
- No sedation but may cause seizure at high doses
256
C.N.S
Antimanic – Mood stabilizing drugs
Mania characterized by: Excessive exuberance & self confidence – Impulsive actions –
Irritability – Aggression – Grandiose delusions
Lithium
Lithium is an endogenous monovalent cation with no known physiological role
Kinetic:
1- Well absorbed orally
2- No hepatic metabolism
3- Excreted by kidneys
- excretion by: Osmotic diuretics & Na+ bicarbonate
- excretion by: Loop & Thiazide diuretics
------------------------------------------------------------------------------------------------------Mechanism of action:
Not clear but may:
1- Affect release of NA, Dopamine, 5HT or,
2- Depletion Phosphatidyl inositol in neuronal membranes of CNS (Inhibit
recycling of inositol) or,
3- Affect nerve conduction
---------------------------------------------------------------------------------------------------------------
Uses:
1- Acute Mania (but slow onset)
2- Manic-Depressive disorders (Bipolar depression) (esp. in manic phase)
---------------------------------------------------------------------------------------------------------------
Side effects:
1- CNS: Confusions - Convulsions
2- Thyroid: Thyroid synthesis
Smooth benign enlargement
3- GIT: Anorexia – Nausea –Vomiting – Diarrhea
4- Kidney: Polyurea (Nephrogenic diabetes insipidus) – Excessive Thirst
5- CVS: Arrhythmia – Hypotension
6- Teratogenic in early pregnancy
7- Acute toxicity: (extremely low safety margin)
Manifistations: - < 2.5 meq/L
Confusions - Drowsiness -Tremors
- > 2.5 meq/L
Convulsions
ttt: Osmotic diuretics - Na+ bicarbonate – Dialysis in severe cases
NB.: Antiepileptic drugs: Carbamazepine & Valproic acid can be used to alleviate some
symptoms of Mania
257
C.N.S
C.N.S STIMULANTS
1- Cerebral stimulants:
1. Amphetamine
2. Atropine
3. Metyhlxanthines
4. Methylphenidate: similar to Amphetamine without anorexigenic effect
5. Cocaine
2- Brain stem stimulants: Analeptics
3- Spinal cord stimulants: Strychnine
Methyl-xanthines
(Caffeine – Theophylline – Theobromine)
Kinetics:
1- Well absorbed from GIT (orally, rectally) & parenterally
2- Distributed all over the body, passes BBB & Placenta
3- Metabolized in the liver into Methyl uric acid which is soluble & don't
precipitate (so not contraindicated in Gout)
4- Excreted in urine
------------------------------------------------------------------------------------------------------Mechanism of action:
1- PDE enz. Type IV
c.AMP
2- Block adenosine receptors
------------------------------------------------------------------------------------------------------Actions:
.
NB.: Caffeine is more selective & potent on: CNS, Gastric acidity & Sk..m
1- CNS:
1.
2.
3.
2- CVS:
Direct effect:
Central effect:
Net result:
Caffeine
Cortex: Alertness – Wakefulness – Antifatigue
Medulla: RC – VMC – CIC
Spinal Cord: Hyper-reflexia
Theophylline
Heart
- +ve inotropic & chronotropic
- Work & Automaticity
-ve chronotropic ( CIC)
- SD No effect
- LD Direct action takes the upper
hand
Tachycardia - Arrhythmia
3- Respiration:
Blood vessel
VD but cerebral VC
VC
- SD No effect
- LD Direct action takes the
upper hand
Hypotension
- Direct: Bronchodilataion & Mast cell stabilization (Theophylline)
- Central: RC (Caffeine)
258
C.N.S
4- GIT:
Spasmolytic &
5- Kidney:
Acidity
Theophylline
1. Spasmolytic
2. Diuretic: Extrarenal ( CO) & Renal ( NaCl reabsorption)
6- Smooth m.: Theophylline Spasmolytic
7- Skeletal m.: Caffeine
Capacity for muscle work
---------------------------------------------------------------------------------------------------------------
Uses:
1- Theophylline:
a- Aminophylline:
1. Anticolic
2. Bronchial asthma: acute attack – status – prophylaxis
3. Cardiac asthma (Acute pulmonary edema):
+ve inotropic – Diuretic – Bronchodilatation
4. Diuretic
b- Pentoxifylline:
used in intermittent claudication ( flexibility of RBCs & platelet
aggregation)
2- Caffeine:
1. Acute Migraine headache (+ Ergotamine)
2. Myasthenia gravis (+ Neostigmine)
3. Mental & physical fatigue
4. Toxicity with CNS depressant
---------------------------------------------------------------------------------------------------------------
Side effects
1- Caffeine: [High therapeutic index]
- CNS: Headache – Insomnia – Irritability - Convulsions
- GIT: hyperacidity
2- Aminophylline: [Low therapeutic index]
1. Irritant: IV
Thrombophlebitis - Rectal
Proctatitis
2. Rapid IV
Velocity reaction & syncope
3. CNS: Headache – Insomnia – Irritability – Convulsions
4. CVS: Arrhythmia – Arrest – Hypotension
5. GIT: Irritation
3- Long use: Tolerance – Cross tolerance – Psychic dependence
---------------------------------------------------------------------------------------------------------------
Contraindications:
1- Arrhythmia
2- Angina
3- Peptic ulcer
---------------------------------------------------------------------------------------------------------------
Drug interaction:
1- Metabolism by:
2- Metabolism by:
1. Antimicrobials: Erythromycin & Quinolones 1. Anti-epileptics
2. Cimitidine
2. Rifampicin
3. Heart & liver disease
3. Smoking
259
C.N.S
Cocaine
Natural from coca leaves
Mechanism of action:
1- Local anesthetic: Block Na+ channels
2- Catecholamines: Neuronal uptake & MAO inhibitor
Actions:
1- L.A.: as surface anesthesia only
2- CNS: stimulation but less than Caffeine
3- CVS:
- Heart:
- SD
Bradycardia ( CIC)
- LD
Tachycardia ( catecholamines)
- B.V:
VC
4- Eye: Active Mydriasis + Decongestion + Loss of corneal reflex
Side effects:
1- Excitation & Convulsions
2- Arrhythmia
3- Death from respiratory failure
4- Dependence (No Tolerance)
Character:
Analeptics
1- Stimulate RC & VMC
2- Awaken deeply anesthetized patient
3- Toxic dose produces Clonic convulsions & with larger dose
Tonic
Classification:
1- Direct:
1. Bemegride: used in acute barbiturate poisoning
2. Phnylenetetrazole (Leptazole – Cardiazole): used in diagnosis of
epilepsy
3. Picrotoxin: has narrow safety margin
2- Indirect (Reflex): through stimulation of Chemoreceptors eg: Lobeline
3- Dual:
1. Coramine (Nikethamide)
2. Carbogen (5 % CO2 + 95 % O2)
3. Daptazole (Amiphenazole)
4. Doxapram : the safest – IV infusion
5. Ethamivan
NB.: Analeptics are OBSOLETE nowadays (Except carbogen & doxapram)
Other drugs having analeptic effects:
1. Reflex through of nerve ending eg: Ammonia – Alcohol – Camphor
2. Descending stimulation eg: Aminophylline
3. Ascending stimulation eg: Strychnine
4. Receptor blockers: as Naloxone & Flumazenil only if RC by opioid
or benzodiazepine
260
C.N.S
Alkaloid from Nux-Vomica seeds
Strychnine
Dynamic:
CNS: Stimulation
- Compete with Glycine in spinal cord
- Ascending: - Spinal cord
Polysynaptic
- Medulla
RC & VMC
- Cortex
Sensory area
Toxicity:
1- Tonic convulsions
2- Cause of death: Spasm of respiratory muscles
ttt:
1. Dark room
2. Stomach wash by tannic acid or K+ permanganate
3. Anticonvulsants
4. Specific antidote: Mephenesine IV
Psychomemitic drugs
- Mechanism:
- Actions:
- Long use:
1- LSD (Lysergic acid
diethylamide)
2- Cannabis (Hashish):
Tetrahydrocannabinol
5-HT1A agonist in CNS &
5-HT2 antagonist in periphery
Eye:
Mydriasis – Visual hallucination
CNS:
- Elation – Mood changes
- Bad trip of severe anxiety –
Depression & suicide
- Cannabinoid recept
c.AMP
- Block Ca++ channels
Eye:
Red conjunctiva - IOP
CNS:
- Loss of sense of: time – sounds
& distance
- Euphoria & uncontrolled
laughing
- Antiemetic (Tried in vomiting
due to cancer therapy)
- Tolerance but no physical
dependence
- Tolerance but no physical
dependence
3- Mescaline
4- Adrenochrome
261