* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Help! My Brain`s Stuck! - Ontario Psychological Association
Substance dependence wikipedia , lookup
Autism therapies wikipedia , lookup
Rumination syndrome wikipedia , lookup
Kleptomania wikipedia , lookup
History of psychiatric institutions wikipedia , lookup
Excoriation disorder wikipedia , lookup
Conversion disorder wikipedia , lookup
Emergency psychiatry wikipedia , lookup
Mental disorder wikipedia , lookup
Mental status examination wikipedia , lookup
Pyotr Gannushkin wikipedia , lookup
Separation anxiety disorder wikipedia , lookup
Narcissistic personality disorder wikipedia , lookup
Autism spectrum wikipedia , lookup
Moral treatment wikipedia , lookup
Spectrum disorder wikipedia , lookup
Controversy surrounding psychiatry wikipedia , lookup
Dissociative identity disorder wikipedia , lookup
Child psychopathology wikipedia , lookup
Generalized anxiety disorder wikipedia , lookup
Classification of mental disorders wikipedia , lookup
Asperger syndrome wikipedia , lookup
History of psychiatry wikipedia , lookup
Abnormal psychology wikipedia , lookup
Obsessive–compulsive personality disorder wikipedia , lookup
Diagnostic and Statistical Manual of Mental Disorders wikipedia , lookup
Tourette syndrome wikipedia , lookup
History of mental disorders wikipedia , lookup
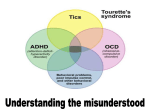
3/10/2015 “Help! My Brain’s Stuck!” Conflicts of Interest Repetitive Behaviours (RBs) in Children and Adolescents None to disclose Drs. Kim Edwards, Holly McGinn, & Sandra Mendlowitz Ontario Psychological Association Conference Friday February 20th, 2015 Test YOUR Repetitive Behaviour IQ 1. Which is not an RB? (multiple choice: pick 1) A. Trichotillomania B. Onychophagia C. Autism D. Dermatillomania 2. RB's are maintained by (multiple choice: pick 1) A. A cycle of reinforcement B. Elevated dopamine levels C. School failure D. Allergies Test YOUR Repetitive Behaviour IQ 3. What are the two most common comorbid disorders with Tourette Syndrome? 4. In early childhood (e.g., 2-6 yrs old), many children demonstrate some obsessive-compulsive behaviors that are part of normal development. (true/false) 5. Hair pulling usually develops as a result of a traumatic experience. (true/false) Learning Objectives Outline What are RBs? (1) Presentation & assessment of TS, OCD, & TTM (2) Similarities & differences among RBs Why study RBs? What causes & maintains RBs? (Behavioural Model) Tourette Syndrome (TS) Trichotillomania (TTM) (3) Behavioural model of RBs & treatment (4) Developmental issues impacting treatment Obsessive Compulsive Disorder (OCD) Similarities & Differences among RBs Developmental Issues Leaky Brake Analogy 1 3/10/2015 What are RB’s? Why Study RBs? Labels Body Focussed RBs Obsessive-Compulsive (OC) Spectrum Conditions Impulse Control Disorders Behaviours Dermatillomania/Excoriation (Skin Picking) Onychophagia (Nail Biting) Trichotillomania (Hair Pulling) Tics Compulsions Stereotypies (Autism) “Nervous Habits” or Actual Problems? RBs: Myths and Facts Not as severe as other psychiatric conditions Uncommon Socially acceptable Purposeful Only impact the individual with the RB Etiology Genetics Brain Circuits Cortico-striatal-thalamo-cortical (CSTC) circuits Neurotransmitters Dopamine, Serotonin, Noreepinephrine Environment Behavioural Model of RBs Internal Environment Tics TTM Behavioural Model of RBs External Environment Negative Reinforcement o absolved of expectations or demands Positive Reinforcement o attention, comfort, support, reward OCD 2 3/10/2015 Meet Brad Tics & Tourette Syndrome (TS) Tics: Assessment & Diagnostic Issues Sudden, rapid, recurrent, non-rhythmic motor movements or vocalizations Motor Blinking Simple Complex Facial grimace + Head twist Vocal Throat clearing Echolalia Tic Disorders (DSM 5): Tourette Syndrome Persistent (Chronic) Motor or Vocal Tic Disorder Provisional Tic Disorder Tics: Assessment & Diagnostic Issues Premonitory Urge Relatively common (20%) More common in boys (4:1) Comorbid Conditions (The “+” in TS+) ADHD = 50%, OCD = 30 - 40 % (Himle & Woods, 2005; Scahill et al., 2005; Scahill et al., 2009; Woods & Himle, 2004; Woods 2008) Course Peak Severity Ages 10-12 Comprehensive Behavioural Intervention for Tics Decline in severity for most Onset Ages 4-7 Internal Environment: Habit Reversal Training Awareness Training Competing Response External Environment: Positive and Negative Reinforcement Psychoeducation (e.g., Leckman et al., 1998; Woods & Specht, 2013) (Woods et al., 2008) 3 3/10/2015 CBIT Efficacy Tics: Tips & Tricks European clinical guidelines for TS & other tic disorders, 2011 Canadian guidelines for the evidence-based treatment of tic disorders, 2012 Education is often the only treatment needed Don’t forget about the comorbid conditions Shift in the way we think about tics Ignore vs. Increase awareness? Practice Parameters for the Assessment & Treatment of Children & Adolescents with Tic Disorders, 2013 (Bennett et al., 2013) TTM (Hair-Pulling Disorder) DIAGNOSTIC CRITERIA DSM 4TR – Impulse Control Disorders Not Elsewhere Classif. DSM-5: Obsessive Compulsive Disorders & Related Disorders Trichotillomania (TTM) DSM 4-TR DSM 5 Recurrent pulling out of one’s hair resulting in hair loss √ √ Increasing sense of tension immediately before pulling out the hair / when attempting to resist behavior √ Pleasure, gratification, or relief when pulling out the hair √ Repeated attempts to decrease or stop hair pulling. √ The disturbance (hair pulling- DSM 5) is not better accounted for by another mental disorder and is not due to a general medical condition (e.g., a dermatological condition) √ √ The disturbance (hair pulling- DSM 5) causes clinically significant distress or impairment in social, occupational, or other important areas of functioning √ √ The hair pulling is not better explained by the symptoms of another mental disorder (e.g., attempts to improve a perceived defect or flaw in appears in body dysmorphic disorder) Developmental Perspectives Pulling/Picking Sites Site % Adults % Children Scalp Eyebrows Eyelashes Legs Arms Pubic other More than one site 79 65 59 59 30 17 25 - 85 52 38 27 18 9 58 The Trichotillomania Impact Project: Exploring Phenomenology, Functional Impairment, & Treatment Utilization J Clin Psychiatry 67:12, December 2006 √ Developmental Perspectives Pulling/Picking Characteristics Pulling/Picking Characteristic Adults Children % of time Unpleasant urges prior 71-89% 29% never/almost never experienced pre-tension To achieve a certain bodily sensation 30-70% 13% never/almost never “pleasure or relief” Preceded by bodily sensation Preceded by anxiety 71-89% - 0-10% - Urge increases when resisting 71-89% - Post pulling anxiety 90-100% - Awareness of pulling 71-89% 4% never/almost never The Trichotillomania Impact Project: Exploring Phenomenology, Functional Impairment, & Treatment Utilization J Clin Psychiatry 67:12, December 2006 4 3/10/2015 TTM -Rituals Comorbid Disorders DSM Tactile stimulation of lips or face. A need to pull in a particular manner. Ritualistically placing, saving, or discarding hairs. Twirling, rolling, or examining the hair. Hairs that don’t feel right (i.e. coarse). Hairs that don’t look right (i.e. color). Compelled to achieve an absolutely even hairline. Need to extract an intact hair bulb. Need to bite or mince the hair or bulb Swallowing hair (trichophagy) http://www.ohsu.edu/ Depression Generalized Anxiety Disorder Simple Phobia Alcohol Abuse Substance Abuse OCD Social Phobia Eating Disorders % 57 27 19 19 16 13 11 11 http://www.ohsu.edu TREATMENT Cognitive Behavioral Therapy Identify dyfunctional thinking and challenge thoughts Relaxation training Treatment Habit Reversal Training Behavioral – Habit Reversal Training Awareness training Identify preceding urge, self-monitoring – place (tv, bedroom, bathroom, etc), emotions, sensory; aware of triggers Stimulus control Reduce urge; techniques to prevent pulling gloves; holding pencils REMOVE environmental cues! Wearing Competing response Incompatible behaviors at onset of urge in physically incompatible behavior – making a fist until the urge diminishes Engaging TTM – Keys to Successful Outcomes Thorough and knowledgeable assessment Emphasize treatment is a progress Motivational for change Use of first line treatments: Obsessive-Compulsive Disorder (OCD) Cognitive Behavioral (CBT) and Habit Reversal Training 5 3/10/2015 Meet Claire OCD: Assessment & Diagnostic Issues Obsessions and/or compulsions that take up more than an hour a day and cause significant distress or impairment Obsessions Recurrent and persistent thoughts, urges, or images that are intrusive and unwanted Compulsions Repetitive behaviors or mental acts that one feels driven to perform in response to an obsession or according to rules OCD: Assessment & Diagnostic Issues Treatment Guidelines for OCD (CBT and SSRIs) Efficacy Common themes: Contamination and cleaning Checking or symmetry Ordering or counting Fear of harm to self or others CBT alone or CBT with SSRI Lifetime prevalence = approx. 2%, chronic, fluctuates Practice Parameters for the Assessment & Treatment of Children & Adolescents with OCD, 2012 Mean age of onset is bimodal peaks at 11 and 23 years Early-onset OCD 1st Peak Age 11 2nd Peak Age 23 More common in boys than girls More likely comorbid with tics Generally more severe Cognitive Behavioural Therapy (CBT) Controlled studies support the efficacy of Cognitive Behavioural Therapy (CBT) that emphasizes Exposure and Response Prevention (ERP) Parental involvement is crucial for success Parents do not accept symptoms Child not responsible for controlling symptoms Child responsible for controlling symptoms Parents accept/tolerate symptoms CBT for OCD: Critical Components Treatment Component Operational Definition Psychoeducation Both the child and the family need to have an accurate understanding of OCD Symptom Monitoring Identify/track sx frequency and duration; Set targets to work towards Relaxation Training Deep Breathing, Muscle Tension Relaxation, Imagery Cognitive Strategies Generate and reinforce accurate thoughts to challenge obsessions and compulsions Exposure & Response Prevention (ERP) Confronting an OCD-eliciting situation (action, object, place, etc.) while preventing the associated compulsions and/or avoidance Homework Change cannot occur exclusively through CBT sessions; strategies must be practiced at home 6 3/10/2015 Childhood OCD: Tips & Tricks Childhood and adult OCD are more similar than not. However, some differences exist : Obsessions develop later that compulsions Poor insight is more common in children Children tend to under-estimate the impact of their OCD Children are more likely to present with comorbid OCD and tics Similarities vs. Differences 8 statements on the next 2 slides Comparing & Contrasting RBs Similarities vs. Differences (1) Behaviour done in response to a sensation (2) Comorbidities are common & frequent Decide whether statement is a similarity (applicable across the RBs discussed – OCD, TTM, TS) or whether it is a difference (applicable to 0,1 or 2 but NOT all RBs discussed) (3) Competing responses are part of treatment (4) Onset usually before age 10 Similarities vs. Differences (5) Symptoms wax and wane (6) Personal distress required for treatment How did you do? (7) More common in males (8) Medications could be useful 7 3/10/2015 Similarities vs. Differences Comprehensive Comparison Differences Similarities (2) Comorbidities = common + frequent (5) Symptoms wax & wane (8) Medications could be useful (1) Behaviour done in response to a sensation (3) Competing responses are part of treatment (4) Onset usually before age 10 (6) Personal distress required for treatment (7) More common in males Developmental Issues “I’m not sure if I’m ready to change” Unconcerned Lack by RB of insight into RB An Analogy for Understanding RBs Brake Shop Model Welcome to the Leaky Brake Club Leaky brakes over attention +/or impulsivity (ADHD) Leaky brakes over thoughts (OCD) Leaky brakes over movements and/or sounds (TICS) Parent involvement Leaky brakes over behaviour (ODD, CD, rage) Leaky brakes over senses (Sensory integration disorder) Take Home Messages Patient & Family Resources Leaky Brakes = Help child understand RB Society: “Just Stop” vs. Patient: “I would if I could” Awareness of behaviour & reinforcement patterns RBs = a spectrum Function of behaviour important differential More research needed! 8 3/10/2015 Clinician Manuals/Resources Woods & Miltenberger (2001). Tic disorders, trichotillomania, and other RB disorders: Behavioural Approaches to Analysis and Treatment. USA: Kluewer Academic Publishers OCD OCD in Children and Adolescents: A Cognitive-Behavioral Treatment Manual by John March and Karen Mulle Tics Woods et al., (2008). Managing TS: A behavioural intervention for children & Adults. Therapist Guide. USA: Oxford University Press. Thank You Questions, Comments, Thoughts Contact Information: [email protected] [email protected] [email protected] TTM Golomb & Vavrichek ( 2000) The hair pulling habit and you: How to solve the TTM puzzle. Maryland: Writers’ Cooperative of Greater Washington. 9