* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download GIANT TRUE CYST OF THE MITRAL VALVE WITH OBSTRUCTION
Heart failure wikipedia , lookup
Electrocardiography wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Myocardial infarction wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Jatene procedure wikipedia , lookup
Cardiac surgery wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
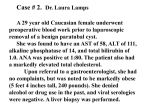
GIANT TRUE CYST OF THE MITRAL VALVE WITH OBSTRUCTION OF THE LEFT VENTRICULAR OUTFLOW TRACT. RADIOLOGICAL DIAGNOSIS AND SURGICAL TREATMENT V.V. Sokolov, A.I. Kovalyov, N.M. Bikbova, N.I. Kharitonova, N.V. Kurlykina, V.Y. Sinitsyn, E.A. Mershina, G.A. Nefyodova N.V. Sklifosovsky Research Institute of Emergency Medicine of the Moscow Healthcare Department, Moscow, Russian Federation ABSTRACT Intracardiac cyst is an extremely rare disease in adults. The article describes the clinical observation of the true cyst of the mitral valve, which led to obstruction of the left ventricular outflow tract. A young woman underwent transthoracic echocardiography due to complaints for shortness of breath, which revealed a floating rounded formation with the echo negative content on the anterior flap of the mitral valve. Transesophageal echocardiography and magnetic resonance imaging confirmed the presence of intracardiac formation. The patient was successfully operated on. The histological test verified the true (congenital) cyst of the mitral valve. true intracardiac cyst, disease of the mitral valve, echocardiography. Keywords: EchoCG — echocardiography ECG — electrocardiography LV — left ventricle MRI — magnetic resonance tomography MV — mitral valve INTRODUCTION An intracardiac true cyst is a rare disease. Cysts are mainly revealed during the autopsy of the fetus or child under the age of 6 months [1-3]. The world literature describes approximately 35 clinical cases of a true cyst in adults. The most common cysts are located in the area of valves [4] and are usually asymptomatic or accompanied by a poor clinical picture. In some cases, the disease manifests with embolic complications, dysfunction or valves or obstruction of left ventricular outflow tract (LV) [5, 6]. Clinical case review A 28-year-old female patient S. was admitted to the Department of Emergency Cardiac Surgery, Circulatory Support and Cardiac Tansplantation of the N.V. Sklifosovsky Research Institute for Emergency Medicine with preliminary diagnosis of a neoplasm (myxoma?) in the left ventricular cavity. Complaint of shortness of breath upon admission. The general condition of moderate severity. Auscultation of the heart in all points gave the systolic murmur. No other pathological changes. Electrocardiography (ECG) and chest x-ray revealed no abnormalities. Magnetic resonance imaging (MRI) of the heart in the left ventricular cavity showed multinodular (3 nodes) soft tissue formation, connected with chords of the mitral valve (MV). The largest of the nodes (28x18 mm) was movable and prolapsed into the LV outflow tract during the systole, leading to its partial obstruction. The diameter of the other nodes did not exceed 12 mm, their mobility was restricted. According to MRI findings we suggested the presence of a multinodular myxoma, attached to the MV chords and leading to obstruction of left ventricular outflow tract (Fig. 1). Transthoracic echocardiography (echocardiography) identified three thin-wall ovoid floating structures with echonegative content fixed to the ventricular surface of the anterior cusp of MV: one formation of 19x19 mm and two of 8x8 mm (Fig. 2). During the systole, larger formation prolapsed into the LV outflow tract, creating an obstruction of blood flow with maximum intraventricular pressure gradient at rest of 144 mm Hg (Fig. 3). Chambers of the heart were not enlarged. There was a moderate left ventricular hypertrophy (thickness of the left ventricular posterior wall and interventricular septum 1.1 cm, myocardial mass index – 120 g/m2) . LV diastolic dysfunction type 1. LV systolic function was not impaired (ejection fraction – 59%). Transesophageal echocardiography confirmed the presence of formations and refined their location. A B Fig. 1. Magnetic resonance imaging of the heart: A – multinodular ventricular cavity formation having connected with chords of MV (arrow), B – formation prolapsing into left ventricular outflow tract during the systole Fig. 2. Transthoracic echocardiography (parasternal position, the long axis), ovoid thin-wall formations on the MV anterior cusp A B Fig. 3. Transthoracic echocardiography (apical five-chamber position): A – a cyst prolapsing into the outflow tract of the left ventricle during systole, and B – growth of the blood flow in the left ventricular outflow tract up to 6 m/s Given the presence of intracardiac formation, creating significant obstruction of the LV outflow tract and threatening with embolic complications, the patient underwent the removal of the fomation and the MV replacement. Intraoperative: on the ventricular side of the A2 segment of the MV at the junction of the marginal chord with the anterior mitral cusp, liquid mass lesion (cyst) of irregular shape, consisting of several chambers was visualized: one chamber of 20x30 mm and two ones of 10x10 mm. All chambers were in a single cavity filled with hemorrhagic fluid (Fig. 4). After excision of the cyst, the large defect of the anterior cusp appeared, which required the MV replacement with the bileaflet mechanical prosthesis On-X 27/29. Fig. 4. Macropreparations of the removed cyst. Arrows indicate the cyst chamber The postoperative period was uneventful. Histological examination revealed that the cyst wall was represented by fibrous tissue; the inner lining was somewhere undetermined, and somewhere represented by a single-row flattened epithelial layer. Such changes are characteristic of true (congenital) cyst (Fig. 5). A B Fig. 5. The results of histological examination. The wall of the cyst is presented by fibrous tissue, parallel connective tissue fibers () and lined with a single row flattened endothelium (). A – Van Gieson's stain, x40; B – Van Gieson's stain, x100 According to the test echocardiography after the operation, the function of the prosthetic MV was satisfactory, LV systolic function was not impaired. The patient was discharged in satisfactory condition 8 days after the surgery. The test echocardiography 3 months later showed satisfactory functioning of the prosthetic MV, there were no additional formations in the cavities of the heart, there was a regression of LV hypertrophy (myocardial mass index – 89 g/m2 compared with the original – a decrease by 25.8%). DISCUSSION Intracardiac blood cysts are extremely rare in adult patients. As already mentioned, it is usually found during the autopsy of the fetus or child under the age of 6 months [1-3]. For the first time, the blood cyst was described in 1844 by Elsasser [1, 7], and presented by the echocardiography by Hauser in 1983 [8]. There are several theories of the development of these cysts [5, 9, 10]. According to the first theory, the blood enters the tissue folds and isolates in it during the valve formation [2]. This hypothesis explains the presence of cysts in newborns, but does not explain its occurrence in adults who had prior echoCG showing normal morphology of the MV [5]. Another theory suggests that the cyst is the result of hematomas formation in subvalvular region due to occlusion of the small branches of arteries associated with inflammation, vagal activity, anoxia or hemorrhage [11]. The other theories relate to the abnormal migration of primary pericardium into the myocardium during the formation of fibrous structures, ectasia or dilation of valvular blood vessels [6]. Thus, intracardiac cyst is a formation, often congenital, emerging from the endothelium, mostly along the lines of cusps co-optation [12] and is a soft cardiovascular neoplasm of a rounded shape with thin smooth walls and liquid hemorrhagic content. Sizes vary from 1 mm to several centimeters in diameter. The ehocardiographic study show that the cyst as a thin-walled rounded formation, often multi-chamber, with echo negative content. The differential diagnosis should be made with hemangioma, myxoma, vegetations, thrombi, echinococcus cyst, malignant neoplasms. Most cysts are found in atrioventricular valves [2, 5, 9, 10, 13, 14], least – in semilunar valves [6, 15], as well as the walls of the cavities of the heart [16-19]. The literature describes cases of cysts after chest trauma [20] or surgery for the heart valves [21]. Typically, these cysts are small and asymptomatic. They can disappear spontaneously in childhood [1], and become large in adulthood and depending on the location, be accompanied by symptoms of valve dysfunction and/or left ventricular outflow tract obstruction, [7, 13, 14]. We should note serious complications such as embolism and sudden death [4-6]. Since an intracardiac cyst is a very rare disease, there is currently no consensus on the choice of the optimal method for treatment of patients. Perhaps, it is reasonable to perform the conservative therapy in asymptomatic patients with small cysts before symptoms appear. At the same time, it is impossible to predict blood cyst development scenario. Therefore, in order to prevent serious complications in the majority of cases the cyst is removed. In the present observation the cyst was congenital, and eventually led to the obstruction of the left ventricular outflow tract. As LV myocardial hypertrophy had already been formed and the patient did not suffer hypertension, we may assume that the obstruction had existed for a long time. Given the size of the cyst and its associated complications, the tactics was obvious. CONCLUSION Transthoracic echocardiography is a simple and reliable method for the detection of intracardiac structures and evaluation of myocardial and heart valve functions. Transesophageal echocardiography and MRI are methods of choice for more accurate localization of intracardiac structures and formations, as well as the exclusion of related abnormalities. In the absence of specific recommendations for the treatment of patients with intracardiac blood cyst, each patient should be treated individually, assessing the potential risk of complications. REFERENCES 1. Zimmerman K.G., Paplanus S. H., Dong S., Nagle R.B. Congenital blood cysts of the heart valves. Hum Pathol. 1983; 14 (8): 699–703. 2. Boyd T. Blood cyst on the heart valves of infants. Am J Pathol. 1949; 25 (4): 757–758. 3. Gallucci V., Stritoni P., Fasoli G., Thiene G. Giant blood cyst of tricuspid valve. Successful excision in an infant. Br. Heart J. 1976; 38 (9): 990–992. 4. Basso C., Valente M., Poletti A., et al. Surgical pathology of primary cardiac and pericardial tumors. Eur J Cardiothorac Surg. 1997; 12 (5): 730–737. 5. Dencker M., Jexmark T., Hansen F., et al. Bileaflet blood cysts on the mitral valve in an adult. J Am Soc Echocardiogr. 2009; 22 (9): 1085.e5–1085.e8. 6. Minato H., Manabe T., Masaki H., Kawahara Y. Blood cyst of the pulmonary valve in an adult: report of a case and review of the literature. Hum Pathol. 1997; 28 (2): 252–255. 7. Elsässer C. Bericht über die ereignisse in der gebäranstalt des Catherinen-Hospital in Jahre 1844. Med Correspondenzblatt. 1844; 14: 297. 8. Hauser A. M., Rathod K., McGill J., et al. Blood cyst of the papillary muscle. Clinical, echocardiographic and anatomic observations. Am J Cardiol. 1983; 51 (3): 612–613. 9. Xie S. W., Lu O. L., Picard M. H. Blood cyst of the mitral valve: detection by transthoracic and transesophageal echocardiography. J Am Soc Echocardiogr. 1992; 5 (5): 547–550. 10. Kuvin J., Saha P., Rastegar H., et al. Blood cyst of the mitral valve apparatus in a woman with a history of orthotopic liver transplantation. J Am Soc Echocardiogr. 2004; 17 (5): 480–482. 11. Pelikan H.M.P, Tsang T.S.M, Seward J.B. Giant blood cyst of the mitral valve. J Am Soc Echocardiogr. 1999; 12 (11): 1005–1007. 12. Burke A., Virmani R. Tumors of the heart and great vessels. Atlas of tumor pathology. Third series, fascicle, 16. Washington: Armed Forces Institute of Pathology. 1996, 79. 13. Paşaoğlu I., Doğan R., Demircin M. Bozer A.Y. Blood cyst of the pulmonary valve causing pulmonic valve stenosis. Am J Cardiol. 1993; 72 (5): 493–494. 14. López-Pardo F., López-Haldón J., Granado-Sánchez C., et al. A heart inside the heart: blood cyst of mitral valve. Echocardiography. 2008; 25 (8): 928–930. 15. Degroff C., Silberbach M., Sahn D.J., Droukas P. Giant blood cyst of the aortic valve. J Am Soc Echocardiogr. 1995; 8 (4): 543–545. 16. Ohmoto Y., Tsuchihashi K., Tanaka S., et al. Giant endocardial blood cyst in left ventricle resected by transaortic valve approach. Chest. 1993; 103 (3): 965–966. 17. Mohanty S.R., Murthy K.S., Krishnanaik S. Cardiac blood-filled cyst at the atrialized portion of the right ventricle in a patient with ebstein anomaly: a case report. J Thorac Cardiovasc Surg. 2000; 120 (2): 422–423. 18. Boyd W.C., Hartman G.S., Reilly D.M., Kreiger K.H. An adult atrial blood cyst. J Cardiotorac Vasc Anest. 1999; 13 (5): 592–593. 19. Otsuka K., Terasaki A., Tonari S. et al. Right atrial blood cyst with total occlusion of the right coronary artery. Heart vessels. 2007; 22 (3): 208–210. 20. Rowe S.K., Porter C.B. Atrial septal hematoma: two-dimensional echocardiographic findings after blunt chest trauma. Am Heart J. 1987; 114 (3): 650–652. 21. Prasad A., Callahan M. J., Malouf J.R. Acquired right atrial blood cyst: a hitherto unrecognized complication of cardiac operation. J Am Soc Echocardiogr. 2003; 16 (4): 377–378. Article received on 18 June, 2015 For correspondence: Viktor Viktorovich Sokolov, Full Professor, Head of the to the Department of Emergency Cardiac Surgery, Circulatory Support and Cardiac Tansplantation, N.V. Sklifosovsky Research Institute for Emergency Medicine of the Moscow Healthcare Department, Russian Federation e-mail: [email protected]