* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Chapter 11 The Endocrine System
Hormonal contraception wikipedia , lookup
Mammary gland wikipedia , lookup
Neuroendocrine tumor wikipedia , lookup
Menstrual cycle wikipedia , lookup
Xenoestrogen wikipedia , lookup
History of catecholamine research wikipedia , lookup
Endocrine disruptor wikipedia , lookup
Triclocarban wikipedia , lookup
Hormone replacement therapy (menopause) wikipedia , lookup
Breast development wikipedia , lookup
Hormone replacement therapy (male-to-female) wikipedia , lookup
Hyperthyroidism wikipedia , lookup
Bioidentical hormone replacement therapy wikipedia , lookup
Congenital adrenal hyperplasia due to 21-hydroxylase deficiency wikipedia , lookup
Hypothalamus wikipedia , lookup
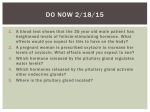
Chapter 11 Lecture Outline* The Endocrine System Eric P. Widmaier Boston University Hershel Raff Medical College of Wisconsin Kevin T. Strang University of Wisconsin - Madison *See PowerPoint Image Slides for all figures and tables pre-inserted into PowerPoint without notes. Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. 1 Fig. 11-1 2 Hormones Structures and Synthesis • Three major chemical classes of hormones – Amines – Peptides and proteins – Steroids 3 Amine Hormones Fig. 11-2 4 Peptide and Protein Hormones Fig. 11-3 5 Steroid Hormones Fig. 11-4 6 Steroid Hormone Synthesis Fig. 11-5 7 Adrenal Gland Hormones Fig. 11-6 8 Synthesis of Sex Hormones Fig. 11-7 9 Hormone Transport in the Blood 10 Hormone Metabolism and Excretion Fig. 11-8 11 Permissive Actions of Hormones Fig. 11-9 12 Hormone Receptors • The ability of a cell to respond to a hormone depends upon the presence of receptors for that hormone on or in the target cell. • An increase in the number of receptors for a hormone is called up-regulation. • A decrease in the number of receptors for a hormone is called down-regulation. 13 Events Elicited by HormoneReceptor Binding 14 Pharmacological Effects of Hormones • Administration of large quantities of a hormone for medical purposes may have effects in an individual that are not usually seen in a healthy person. 15 Inputs that Control Hormone Secretion Fig. 11-10 16 Control by Plasma Concentrations of Mineral Ions or Organic Nutrients Fig. 11-11 17 Control by Neurons Fig. 11-12 18 Control by Other Hormones • A hormone that controls the secretion of another hormone is called a tropic hormone. 19 Types of Endocrine Disorders • Hyposecretion: the secretion of too little hormone. • Hypersecretion: the secretion of too much hormone. • Hyporesponsiveness and Hyperresponsiveness occurs when the target cells do not respond properly to a hormone. 20 The Hypothalamus and Pituitary Gland Fig. 11-13 21 Control Systems Involving the Hypothalamus and Pituitary Fig. 11-14 22 Posterior Pituitary Hormones • The posterior pituitary does not synthesize any hormones; it only secretes them. • Oxytocin is involved in the milk ejection reflex of nursing mothers and emotional bonding. • Antidiuretic hormone (Vasopressin) is involved in regulation of water balance and osmolarity. 23 Fig. 11-15 24 Anterior Pituitary Hormones and the Hypothalamus Fig. 11-17 25 Fig. 11-19 26 Feedback Loops Fig. 11-20 27 The Thyroid Gland Fig. 11-21 28 Synthesis of Thyroid Hormones Fig. 11-22 29 Control of Thyroid Function Fig. 11-23 30 Actions of Thyroid Hormones • Metabolic Actions • Permissive Actions • Growth and Development 31 The Endocrine Response to Stress • The endocrine system responds to stresses on the body such as trauma, infection, pain, sleep deprivation, fright, and other emotional stresses by increasing the release of cortisol from the adrenal cortex and epinephrine from the adrenal medulla. 32 Physiological Functions of Cortisol • Permits action of epinephrine and norepinephrine on muscles and blood vessels. • Maintains cellular concentrations of metabolic enzymes required to produce glucose between meals. • Decreases events associated with the inflammatory response such as capillary permeability and production of prostaglandins. • Important for fetal development. 33 34 Other Hormones Released During Stress • Aldosterone, vasopressin, growth hormone, glucagon, beta-endorphin. • Fight-or-flight response: epinephrine and norepinephrine. 35 Adrenal Insufficiency and Cushing’s Syndrome • The general term for any situation in which plasma levels of cortisol are chronically lower than normal is adrenal insufficiency. • Patients with adrenal insufficiency suffer from a diffuse array of symptoms, depending on the severity and cause of the disease, including: weakness, lethargy, and loss of appetite. • Examination may reveal low blood pressure (in part because cortisol is needed to permit the full extent of the cardiovascular actions of epinephrine) and low blood sugar, especially after fasting (because of the loss of the normal metabolic actions of cortisol). 36 Adrenal Insufficiency and Cushing’s Syndrome • Primary adrenal insufficiency is due to a loss of adrenal cortical function, as may occur, for example, when infectious diseases such as tuberculosis infiltrate the adrenal glands and destroy them. • The adrenals can also (rarely) be destroyed by invasive tumors. • Most commonly the syndrome is due to autoimmune attack causing the destruction of many of the cells of the adrenal glands. • Because of this, all of the zones of the adrenal cortex are affected. Thus, not only cortisol but also aldosterone levels are decreased below normal in primary adrenal insufficiency. 37 Adrenal Insufficiency and Cushing’s Syndrome • This decrease in aldosterone concentration creates the additional problem of an imbalance in Na+, K+, and water in the blood because aldosterone is a key regulator of those variables. • The loss of salt and water balance may lead to hypotension (low blood pressure). • Primary adrenal insufficiency from any of these causes is also known as Addison’s disease. 38 Adrenal Insufficiency and Cushing’s Syndrome • Adrenal insufficiency can also be due to a deficiency of ACTH—secondary adrenal insufficiency—which may arise from pituitary disease. • Its symptoms are often less dramatic than primary adrenal insufficiency, because aldosterone secretion, which does not rely on ACTH, is maintained by other mechanisms. • Adrenal insufficiency can be life-threatening if not treated aggressively. 39 Adrenal Insufficiency and Cushing’s Syndrome • In Cushing’s Syndrome, there is excess cortisol in the blood, even in the nonstressed individual. • The cause may be a primary defect (e.g., a cortisolsecreting tumor of the adrenal) or may be secondary (usually due to an ACTH-secreting tumor of the pituitary gland). • In Cushing’s disease (secondary) the increased blood levels of cortisol tend to promote uncontrolled catabolism of bone, muscle, skin, and other organs. 40 Adrenal Insufficiency and Cushing’s Syndrome • In Cushing’s Syndrome problems include: – Osteoporosis – Muscles weakness – Blood sugar increases to levels observed in diabetes mellitus – Immunosuppression – Redistribution of fat (buffalo hump and moon face) – Hypertension (high blood pressure) • Treatment of Cushing’s Syndrome depends on the cause. – Surgical removal of the pituitary tumor – Adrenalectomy 41 Endocrine Control of Growth • At least a dozen hormones directly or indirectly play important roles in controlling growth. 42 Bone Growth Fig. 11-27 Fig. 11-26 43 Environmental Factors Influencing Growth • Insufficient amounts of amino acids, fatty acids, vitamins, or minerals interferes with growth. 44 Hormonal Influences on Growth • Growth hormone and Insulin-like growth factors • Thyroid hormones • Insulin • Sex hormones (testosterone, estrogen) • Cortisol 45 Fig. 11-28 46 47 48 Parathyroid Hormone • Parathyroid hormone (PH) is secreted by the parathyroid glands (4 glands located in the neck on the thyroid gland). • PH is critically important to regulation of Calcium levels. 49 Fig. 11-31 50 Parathyroid Hormone Fig. 11-32 51 Endocrine Control of Ca2+ Homeostasis • Ca2+ homeostasis is so vital that the absence of the hormones for its control would be catastrophic. • This is a highly regulated and finely balanced system involving several hormones. 52 Effector Sites for Calcium Homeostasis • Calcium storage, absorption into the body and excretion from the body occur at 3 main sites: • Bone • Kidneys • Gastrointestinal Tract 53 Hormonal Controls • Two major hormones regulate plasma calcium concentration: – Parathyroid hormone – 1,25-dihydroxyvitamin D • Calcitonin plays a limited role. 54 1,25-Dihydroxyvitamin D Fig. 11-33 55 Calcitonin • Calcitonin, which is secreted by parafollicular cells of the thyroid gland, decreases plasma calcium concentration by inhibiting osteoclasts. • Its secretion is stimulated by high plasma calcium concentration, and it is only a factor when the concentration is very high. 56 Metabolic Bone Diseases • Rickets (in children) and osteomalacia (in adults) are conditions in which mineralization of bone matrix is deficient, causing the bones to be soft and easily fractured. A major cause of rickets and osteomalacia is deficiency of vitamin D. • Osteoporosis (an imbalance between bone resorption and bone formation) resulting in decreases in bone mass and strength leads to an increased incidence of fractures. • Osteoporosis can occur in people who are immobilized, in people who have an excessive plasma concentration of a hormone that favors bone resorption, and in people who have a deficient plasma concentration of a hormone that favors bone formation. 57 Metabolic Bone Diseases • Osteoporosis is most commonly seen with aging. • Everyone loses bone with age, but osteoporosis is more common in elderly women than in men for several reasons: – Women have a smaller bone mass to begin with – The loss that occurs with aging occurs more rapidly (menopause removes the bone-promoting influence of estrogen) – Pregnancy • Prevention is the focus of attention for osteoporosis. 58 Metabolic Bone Diseases • Treatment options for osteoporosis: – – – – Treatment of postmenopausal women with estrogen A regular weight-bearing exercise program Adequate dietary Ca2+ and vitamin D intake Drugs, called bisphosphonates, that interfere with the resorption of bone by osteoclasts – Other antiresorptive substances include calcitonin and selective estrogen receptor modulators (SERMs), which act by interacting with estrogen receptors, compensating for the low estrogen after menopause. 59 Hypercalcemia • Hypercalcemia is abnormally high levels of Ca2+ levels in the blood. • Cause of hypercalcemia: Primary hyperparathyroidism (caused by a benign tumor in one of the four parathyroid glands) – Certain types of cancer can lead to humoral hypercalcemia of malignancy. – Excessive ingestion of vitamin D can lead to hypercalcemia despite the fact that PTH levels will be very low. – • Hypercalcemia symptoms: – Tiredness – Lethargy with muscle weakness – Nausea and vomiting (due to effects on the GI tract) 60 Hypocalcemia • Hypocalcemia is abnormally low levels of Ca2+ levels in the blood. • Causes: – Primary hypoparathyroidism: loss of parathyroid gland function – Pseudohypoparathyroidism: resistance to the effects of PTH in target tissue, even though PTH levels in the blood tend to be elevated – Secondary hyperparathyroidism: failure to absorb vitamin D from the gastrointestinal tract, or decreased kidney 1,25-(OH)2D production, which can occur in kidney disease • The symptoms of hypocalcemia are: – Increases the excitability of nerves and muscles (seizures, muscle spasms (hypocalcemic tetany), and nerve excitability) • Treatment: – Calcium salts and 1,25-(OH)2D (calcitriol), supplemental dietary Ca2+ and high doses of dietary vitamin D, injections of vitamin D 61