* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Causes - EDExam
Management of acute coronary syndrome wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Myocardial infarction wikipedia , lookup
Jatene procedure wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Cardiac arrest wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
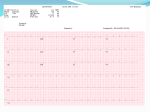
Cardiac Arrhythmias Mx of patient experiencing an arrhythmia: Obtain Rhythm strip Assess: Conscious state Vital signs Chest pain/other syx Reassure Pt Apply O2 If no cardiac output/pt unconscious – start CPR If witnessed, monitored collapse, & Pt in VT or VF – praecordial thump If not hypotensive/dyspnoeic – sitting position ECG Take bloods for FBE, U&E Ca/Mg/PO4, Cardiac enzymes – Urgent K+ Check medication – most anti-arrhythmics are pro-arrhythmic and negatively inotropic NB Digoxin may be toxic at therapeutic levels with LOW K+ Ventricular Tachycardia – VT Irritable ectopic focus in ventricles, may have re-entry circuit Rate: 100-250 bpm No P waves In about 50% AV dissociation present – map P-P intervals, look for hidden P waves In other 50% - P waves discernible – due to retrograde conduction – hard to see at higher rates “Sustained” = longer than 30 secs “Non-Sustained” = less than 30 secs 4 ventricular ectopics in a row = VT ECG Characteristics: Rate atrial: variable, may be independent of ventricles, or retrograde ventricular: 100-250bpm Regularity: Ventric response regular, or very slightly irregular P-R Interval: indeterminable QRS duration: wide >0.12 secs Morphology: P waves – variable if present QRS – wide complex, bizarre looking, may have narrower fusion beats (superimposed SA node & ventric beats) ST – often obscured T – opposite polarity to QRS Causes IHD/AMI Hypoxia K/Mg/pH (acidosis) Digoxin toxicity Indwelling cardiac lines/pacemaker Reperfusion arrhythmias post thrombolysis Treatment Determined by haemodynamic/conscious state of patient Conscious Patient: Symptoms include: Asymptomatic Palpitations Dizziness/Syncope Angina In this setting VT is dangerous as may cardiac output may deteriorate and rhythm can deteriorate into VF. Mx: Apply O2, Check obs 12-lead ECG – may help differentiate VT from SVT with aberrancy Check reversible causes & treat Lignocaine bolus 1mg/kg If it corrects – infusion of lignocaine VT versus SVT with aberrancy VT QRS often > 0.14s Extreme axis deviation (-90 to –180 degrees) Fusion/capture beats (narrow complexes amongst wide ones) Concordance (all +ve or all –ve in V1-V6) Deflection: If +ve in V1 and monophasic r wave OR biphasic & left > right peak of R wave If –ve in V1, r wave >0.03s in V1/V2 slurred S in V1/V2 any Q in V6 r to low point of s >0.06s Unconscious Patient/No pulse: CPR/BLS Defibrillate ASAP Witnessed Monitored Collapse Pt witnessed to go unconscious & into VT (on monitor) – PRAECORDIAL THUMP Only other type of unmonitored collapse that should be thumped is ELECTROCUTION Ventricular Fibrillation: VF Classic ‘cardiac arrest’ Multiple ectopic foci discharging simultaneously in ventricles Disordered chaotic rhythm Cardiac output = zero! Always unconscious, will die without correction! ECG Features: Rate: atrial/ventricular = indeterminable Regularity: irregular P-R interval: indeterminable QRS duration: indeterminable Morphology: Pwaves – absent QRS – chaotic, no uniformity ST – indeterminable Twaves – indeterminable Causes IHD/AMI Electrocution Drug intoxication Trauma Hypothermia <30oC Other – as per VT Treatment CPR/BLS Defibrillate ASAP Early difibrillation provides the best chance of survival: Time in VF pre-defibrillation % Discharged from hospital < 1 min 99% 2 mins 50% > 5 mins 35% Asystole No contraction – “flatline” (misnomer as line is not perfectly flat!) As per VF: Cardiac output = zero! Always unconscious, will die without correction! ECG Features Rate: none or extremely slow QRS – none or wide, bizarre looking Causes End stage of advanced cardiac disease Severe myocardial depression due to hypoxia/drug overdose Management VERIFY ASYSTOLE – to ensure it’s not Isoelectric or “Fine” VF On monitor – cycle through leads I, II & III If monitoring through paddles – swap paddles to 90o Check all connections Check that monitoring through correct input (paddles/monitor) on defibrillator Then: Increase the gain/amplitude on monitor Check for CPR artefact If “flat” or straight line consider Monitor not connected Lead not selected Malfunction CPR Ventilation – ETT 100% O2 Adrenaline 1mg IV, 20ml flush Continue CPR for 3 minutes If still in asystole – Atropine 1mg IV Can repeat Adr/Atropine Consider temporary pacing (early in asystole, especially if there’s a remnant of electrical activity) EMD / PEA Coordinated electrical activity with no cardiac output Causes AMI/IHD Acidosis 4 H’s & 4 T’s 4 H’s Hypoxia Hypovolaemia Hypothermia Hypo/Hyperkalaemia & other metabolic disorders 4 T’s Tamponade Tension Pneumothorax Toxins, poisons, drugs Thromboembolism (massive PE, vena caval obstruction) Non-reversible causes include Massive PE Ruptured Mitral Valve Ruptured ventricle Management CPR/BLS Identify & treat reversible causes ETT, 100% O2 Adrenaline 1mg IV CPR for 3 minutes Atropine 1mg IV Continue CPR & Adrenaline every 3 minutes Idioventricular Rhythm Automaticity of ventricles, “escape rhythm” Rate of about 30-40/min (40-100bpm = “accelerated idioventrcular rhythm”) Each beat has appearance of a ventricular contraction May degenerate to Asystole ECG Features Rate: atrial: nil ventricular: 30-40 Regularity: Regular QRS Duration: widened Morphology: Pwaves – absent QRS Complexes: wide, bizarre looking ST: often obscured T waves: opposite in polarity to QRS Causes Indicates severe disruption to conduction system May be first stable rhythm post conversion of VT/VF/Asystole AMI/IHD Digoxin toxicity Reperfusion (post thrombolysis) Treatment Isoprenaline infusion Temporary pacemaker Ventricular Ectopics Commonest ventricular arrhythmia, many names, can occur in any rhythm Ectopic focus in Purkinje fibres or ventric muscle Wider complex, larger voltage contraction, as usual conduction paths not followed NOT a stronger contraction! Actually CO T wave in opposite direction to QRS Features: Earlier than next expected beat No P wave Wide bizarre QRS (often > 0.14sec) ST segment often obscured T wave – opposite polarity to QRS Next beat: OR When expected After compensatory pause If all ectopics have same morphology – “unifocal” If they have different morphology – “multi-focal” May occur in bigeminal, trigeminal or quadrigeminal arrangements Or in couplets or pairs, or runs of 3 (“Salvos”) 4 or more in a row = VT Causes Most cases = incidental finding IHD/AMI K/pH Digoxin toxicity Indwelling cardiac lines Bradycardia may allow an ectopic focus to emit an ectopic beat Treatment Controversial: Rough Guide: Only treat if VE’s are ing in number or patient compromised Some suggest treatment if combination of: patient compromised more than 5/minute multifocal runs or Salvos R on T phenomenon Any of these in the first 24hrs post MI Remember to exclude/treat causes In early AMI, Lignocaine is drug of choice BUT: AT HR, treatment is to HR first with Atropine Lignocaine may rate/put them into asystole