* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Lecture 16: The Nephron
Countercurrent exchange wikipedia , lookup
Intracranial pressure wikipedia , lookup
Circulatory system wikipedia , lookup
Cardiac output wikipedia , lookup
Haemodynamic response wikipedia , lookup
Biofluid dynamics wikipedia , lookup
Hemodynamics wikipedia , lookup
Reuse of excreta wikipedia , lookup
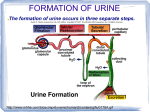
Renal function wikipedia , lookup
Lecture 16: The Nephron Reading: OpenStax A&P Text Chapter 25 Primary functions of the kidneys 1. Regulating osmolarity (blood concentration!) A. Regulating blood pressure B. Maintaining ion balance C. Regulating blood pH 2. Excretion of waste products (either ingested or produced through metabolic reactions) Nephron anatomy 1. Nephron- functional unit of the kidney A. Up to 1 million nephrons/kidney (med pg 310) B. After age 40, number of nephrons decreases 1%/year…but the body compensates, so it isn’t usually a problem… 2. The nephron is a TUBE that is tightly associated with its own blood supply. A. Glomerular capsule B. Proximal convoluted tubule C. Descending loop of Henle D. Ascending loop of Henle E. Distal convoluted tubule F. Collecting duct Blood vessels Each individual nephron has its own blood supply. 1. Big picture—renal artery flows IN, renal vein flows OUT 2. Little picture? Afferent arteriole → glomerulus (capillary bed) → efferent arteriole → peritubular capillaries (sometimes specialize as vasa recta) → veins… 3. The afferent arteriole has a larger diameter than the efferent arteriole. Mechanisms of kidney function 1. Filtration: removing fluid and solutes, en masse, from the blood, and collecting the “stuff” in the nephron tubules. A. This produces FILTRATE in the nephron tubule…but if the substance should be kept in the body, it must be reabsorbed! 2. Reabsorption: taking substances from the filtrate and returning them to the blood 3. Secretion: Selectively removing molecules from the blood and adding them to the filtrate. (Note: This is much different from filtration which is non-specific) 4. Excretion: Removal of substances from the body Biol 7: Human Physiology Spring 16 106 CC-BY Wendy Riggs The renal corpuscle The renal corpuscle is a term to describe two structures: Bowman’s capusle (part of the nephron) and the glomerulus (part of the blood supply). Its structure enables its function: to filter fluild OUT of the blood and INTO the nephron. 1. Glomerular capsule: A. This nephron structure has two layers. The visceral layer of the glomerular capsule tightly covers the glomerular capillaries. It is made of cells, called podocytes, that have interlacing pedicels with filtration slits between them. B. Podocytes COVER the glomerular capillaries, but the filtration slits leave space between each pedicel. C. The parietal layer of the glomerular capsule is connected to the visceral layer, but consists of simple squamous ET and connects to the PCT. 2. Glomerular capillaries A. These are fenestrated capillaries. B. Fenestrations are slits that allow fluid through, but are generally too small for plasma proteins to pass. This creates very LEAKY capillaries in the glomerulus. Filtration 1. 180L fluid filtered OUT of the blood EVERY SINGLE DAY! Or entire plasma volume is filtered out 60x per day! Whaaaat?! 2. Occurs in the glomerulus/Bowman’s capsule 3. Filtration is powered by hydrostatic pressure in the blood (180L net filtration) A. First, review blood pressure in other capillaries…3 L net filtration… i. Hydrostatic pressure: 32 mmHg → 15 mmHg OUT (over the length of the capillary) ii. Osmotic pressure: 25 mmHg IN (constant over cap length, b/c # prot doesn’t change) iii. Net filtration OUT (3 L) B. Blood pressure in the glomerulus is HIGH! i. 55 mmHg OUT… a. Blood pressure (32 mmHg) b. Where does the extra “pressure” come from? Big afferent, small efferent vessels… ii. 45 mmHg IN a. (Osmotic pressure pushing IN due to proteins…30 mm Hg) b. (Hydrostatic pressure in the bowman’s capsule pushing IN: 15) iii. 10 mmHg push stuff OUT. a. This total pressure influences GFR b. Increase this pressure (HOW???) and you increase GFR c. Decrease this pressure and you decrease GFR… 4. You now have filtrate in Bowman’s capsule (180L/day) that is similar in composition to plasma (but no plasma proteins). Myogenic control of GFR At any given moment, only 20% of the plasma is filtered OUT…(why not more?) 1. Rate of filtration is quantified by the Glomerular Filtration Rate (GFR), which is influenced by changes in resistance (diameter) in afferent or efferent arterioles 2. GFR is actively monitored by cells in the kidney. A. Myogenic response i. This is a stretch reflex in the afferent arteriole that has no integrator. ii. Stimulus: increased blood pressure (which causes smooth muscle in the arteriole wall to STRETCH) iii. Response: Vasoconstriction iv. Mechanism: Stretch-sensitive ion channels OPEN when BP increases, and the smooth muscle depolarizes and contracts. Biol 7: Human Physiology Spring 16 107 CC-BY Wendy Riggs v. Vasoconstriction reduces blood flow INTO the glomerulus, which reduces GFR. Tubuloglomerular control of GFR Characteristics of the filtrate in the nephron stimulate blood pressure regulation. 1. Low sodium is detected by macula densa cells in the end of the ALH (beginning of DCT)…this indicates low BP A. Macula densa: Specialized cells in the ALH/DCT that monitor filtrate composition i. (Note the actual orientation of the nephron…the ALH/DCT actually makes CONTACT with the afferent/efferent arterioles! This specialized location is the juxtaglomerular aparatus. a. Juxtaglomerular cells (aka granular ccells) line the afferent/efferent arterioles b. Macula densa cells line the ALH/DCT ii. The purpose of this? To allow MONITORING of filtrate composition and to stimulate APPROPRIATE MODIFICATION based on concentration of filtrate B. Possible mechanism: i. Lower BP leads to lower GFR (glomerular filtration rate) ii. Filtrate stays in nephron longer… iii. More sodium is absorbed from the filtrate iv. Macula densa detects lower Na in filtrate 2. Macula densa cells send a chemical message to afferent arteriole 3. Afferent arteriole releases renin (an enzyme) into the blood 4. Renin converts angiotensinogen in the blood to angiotensin I 5. Angiotensin I encounters “Angiotensin converting enzyme” (ACE), often in the lungs, and is turned into Angiotensin II 6. Angiotensin II has many powerful effects that INCREASE BP, including: A. Vasoconstriction (increases BP) B. Increased cardiac output C. Increased aldosterone production (in adrenal glands) i. Increased thirst (due to increased sodium reabsorption) a. Thirst is stimulated by osmoreceptors in the hypothalamus when plasma osomolarity gets HIGHER than 280mOsm b. Receptors in the oropharynx detect cold water and stop the firing of thirst receptors, regardless of osmolarity. D. Increased vasopressin secretion Biol 7: Human Physiology Spring 16 108 CC-BY Wendy Riggs Lab 16: The Pee Lab! Today we will evaluate the effects of different solutions on urine production. Each person in the lab will ingest a treatment solution and explore urine concentration, pH, specific gravity, and sodium concentration. Cheers! Materials: Urine collector Specific gravity strips Appropriate solution (based on your group) pH paperThermometerGraduated cylinder Potassium chromate Silver nitrate Small test tubes Procedure: 1. Divide into 5 GROUPS: A. Treatment 1: Drink 800 mL water. This imposes a heavy water load that dilutes the extracellular fluid and increases its total volume. B. Treatment 2: Drink 800 mL gatorade. The osmolarity of Gatorade approximately matches your total ECF osmolarity (it is isosmotic), so it should not alter your ECF osmolarity when absorbed by the gut. C. Treatment 3: Drink 80 mL water and take 3 salt tablet (= 3 g of sodium). This imposes a heavy salt load, but should not affect your total ECF volume. Note that most Americans ingest between 7-10 grams of NaCl daily. D. Treatment 4: Drink 300 mL 1% sodium bicarbonate solution. This treatment will produce a metabolic alkalosis. E. Treatment 5: Drink 300 ml of water and swallow a caffeine tablet. The amount of caffeine in each tablet (200 mg) is comparable to that found in 2 cups of freshly brewed coffee. Note: this treatment works best on individuals who do not drink coffee routinely. Treatment Group Baseline Data Start Time Time since last urination 2. The lab begins at TIME = 0. At this time, you will urinate into a cup. This is your BASELINE sample, taken at TIME = 0. 3. Drink your solution. 4. Empty your bladder every 30 minutes for 1.5 hours. 5. Record the following data for EACH urine sample (including your baseline sample!) A. Volume/rate of urine production i. Use a graduated cylinder to measure the volume of each urine sample. Calculate the flow rate in ml/min. Flow rate = urine volume collected (in ml) / 30 min (except for your FIRST calculation!) Time = 0 Volume of Urine (mL) 30 minutes 60 minutes 90 minutes Time = 0 Excretion Rate (mL/min) 30 minutes 60 minutes 90 minutes B. pH: Dip a strip of pH paper in your urine & compare the color of the paper to the scale on the pH paper container. Time = 0 pH of Urine 30 minutes 60 minutes 90 minutes C. Sodium chloride concentration i. Place 10 drops of urine in a test tube. ii. Add 1 drop of 20% potassium chromate. iii. Add 2.9% silver nitrate, drop by drop, and shake the test tube thoroughly between drops, until the solution turns from bright yellow to brown. The number of drops equals the concentration of NaCl in mg/mL. Biol 7: Human Physiology Spring 16 109 CC-BY Wendy Riggs Time = 0 NaCl (mg/mL) = # drops 30 minutes 60 minutes 90 minutes D. Specific gravity (measures concentration of urine) Time = 0 Specific Gravity of Urine 30 minutes 60 minutes 90 minutes E. Estimation of amount of urinary solids i. If the sample of urine were evaporated, the solids contained in the sample could be recovered, and would contain many organic and inorganic compounds. Urea is the principle organic solid; sodium and chloride compounds are the principal inorganic urinary solids. ii. The concentration of urinary solids in grams per liter (g/liter) can be computed by multiplying the last two digits of the specific gravity reading by 2.66, a value known as Long’s coefficient. For example, if the specific gravity is 1.025, the estimated concentration of urinary solids is calculated as follows: 25 x 2.66 = 66.5 g/liter. iii. How does this calculation compare to the NaCl concentration? Time = 0 Estimation of Urinary Solids 30 minutes 60 minutes 90 minutes Enter your data into the Excel worksheet at the front of the room so we can calculate average values for each group. Record the average values in your table. YOU WILL GRAPH THESE AVERAGE VALUES!!! LAB QUESTIONS 1. Discuss results of each GROUP in 5 graphs that display the AVERAGE values for EACH GROUP collected during the lab. 2. Clearly connect each group’s data to exactly what is happening in the kidney. Tie in as many aspects of kidney function as you can. Your answers should refer to the graphs as evidence. 3. Offer a physiological explanation for the differences in total urine excretion across the 5 treatments. 4. Offer a physiological explanation for the differences in total NaCl excretion across the 5 treatments. Determine the molarity of NaCl in the urine sample collected across the entire sampling period, separately for each treatment. (Note: use the treatment means to make this calculation.) 5. Based on your results, which treatment do you think elicited the greatest ADH production? The least production? Explain. 6. What was the relationship between specific gravity of a urine sample and the rate at which urine was excreted? 7. For each of the five treatments, what is the relationship between urine osmolality, specific gravity, and NaCl excretion? Explain. 8. Based on the results you obtained, attempt to explain how caffeine produces its diuretic effects. (Note: do not simply say that it increases GFR and reduces tubular uptake of sodium. Try to go further and explain why how these two effects increase urine flow.) 9. Create 5 graphs that display the AVERAGE values for EACH GROUP collected during the lab. 10. Clearly connect each group’s data to exactly what is happening in the kidney. Tie in as many aspects of kidney function as you can. Your answers should refer to the graphs as evidence. Helpful resources: http://library.med.utah.edu/WebPath/TUTORIAL/URINE/URINE.html#2 http://www.texascollaborative.org/spencer_urinalysis/ds_sub3.htm Biol 7: Human Physiology Spring 16 110 CC-BY Wendy Riggs External Brain 16: The Nephron Study Guide Questions 1. Distinguish between the following words: Filtration, Reabsorption, Secretion, Excretion 2. Be able to describe (or draw) the flow of filtrate through the nephron. 3. Know the function of the glomerulus, as well as all sections of the nephron tubule. 4. Be able to describe (or draw) the flow of blood associated with the nephron. 5. Understand how the structure of the glomerulus enables its unique function. 6. Explain the various pressures acting within the glomerulus that promote filtration. Compare these pressures to the pressures present in systemic capillaries where nutrient and waste exchange occurs. 7. What is the transport maximum (Tm)? 8. Describe the relationship between filtration rate, reabsorption rate, excretion rate and renal threshold. 9. Be able to describe (or draw) the flow of filtrate (the fluid filtered out at the glomerulus) through the nephron. 10. Describe the mechanism by which the kidney monitors blood pressure. 11. Be able to address metabolic changes and their effects on vessel resistance. (How will increased metabolic needs affect vessel resistance? Think about cellular respiration…) Biol 7: Human Physiology Spring 16 111 CC-BY Wendy Riggs










![Urinary System_student handout[1].](http://s1.studyres.com/store/data/008293858_1-b77b303d5bfb3ec35a6e80f57f440bef-150x150.png)
