* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Document
Saturated fat and cardiovascular disease wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Aortic stenosis wikipedia , lookup
Heart failure wikipedia , lookup
Cardiac surgery wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Electrocardiography wikipedia , lookup
Coronary artery disease wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
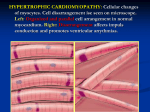
Hypertrophic cardiomyopathy Dipin.s Junior resident Internal medicine • Autosomal dominant disease of the heart muscle, characterized by a small left ventricular cavity and marked hypertrophy of the myocardium with myofibril disarray. • Overall prevalence is 1:500 to 1:1000 • Disease of the myofilaments, with alteration in structure and function • Most common cause of sudden cardiac death in young people. • Asymmetric septal hypertrophy (ASH) • Idiopathic hypertrophic subaortic stenosis (IHSS) • Muscle subaortic stenosis • Hypertrophic obstructive cardiomyopathy (HOCM). Etiology • Most common genetic cardiovascular disease • Mutation in genes encoding proteins of the cardiac sarcomere myofilaments • Beta-myosin heavy chain, myosin-binding protein C, cardiac troponin T and I,alpha -tropomyosin, actin, titin, and myosin light chains • Other genes outside of the sarcomere myofilaments have also been recently implicated • Deletions, insertions, missense, and splice site mutations. • Hypothesis is that sarcomeric dysfunction leads to compensatory hypertrophy. pathology • Asymmetrical hypertrophy with a small LV cavity • Mural endocardium thickened by fibrous tissue • Elongation of chordae and ant. displacement of the hypertrophied papillary muscles • LA is usually dilated Histology • Short runs of severely hypertrophied fibers interrupted by connective tissue • Large and bizarre nuclei and fibrosis , with degenerating muscle fibers. • Whorling of muscle fibers is characteristic of HCM Pathophysiology Diastolic dysfunction • Impaired ventricular relaxation and chamber stiffness • Compensatory increase in late diastolic filling by atrial systole. • During exercise or any other type of catecholamine stimulation, diastolic filling period decreases as well as myocardial ischemia occurs • Leads to severe diastolic dysfunction- dyspnoea LVOT obstruction • Multifactorial • During systolic contraction the hypertrophied basal septum encroaches to the outflow tract • Mitral leaflets are pulled in by the venturi force • In midcavitary region hypertrophied pappillary muscles pressing against septum may cause obstruction • LVOT obstruction is dynamic • Increased myocardial contractility, decreased ventricular volume, or decreased afterload ----increases Myocardial ischaemia • Supply-demand mismatch • compromised coronary blood flow to the LV myocardium -- abnormally small and partially obliterated intramural coronary arteries Autonomic dysfunction • Either a failure of systolic blood pressure to rise >20 mmHg or a fall in systolic blood pressure during excercise. • Speculated that there is high degree of abnormal autonomic tone in HCM • Assoc. with poor prognosis Mitral regurgitation • Secondary phenomenon due to systolic anterior motion of leaflets due to LVOT obstruction • During mid and late systole- jet directed post. and laterally Clinical presentation • Most are asymptomatic • Dyspnoea-diastolic dysfunction and elevated LV filling pressures • Angina – epicardial coronary disease may be absent • Syncope or presyncope- LV baroreceptors causes reflex vasodilatation • Atrial fibrillation occurs more in elderly Physical examination • Carotid pulse- spike and dome pattern rapid rise (percussion wave) midsystolic drop secondary wave (tidal wave) • Jugular venous pressue- usually normal; sometimes prominent a wave (hypertrophy and lack of compliant RV and powerful Rt atrial contraction) • Apical impulse- forceful, sustained, diffuse double or triple apical impulse (outward thrust of ventricular contraction, a presystolic accentuated atrial contraction, and expansion of early diastolic filling) • Cardiac sounds- usually split sometimes paradoxically split S4 if severe hypertrophy • Murmurs =crescendo–decrescendo murmur located primarily at the left sternal border. (usually ends before S2) • May radiate to the base or apex, but seldom radiation to the carotid arteries. • Any condition which increases the LVOT outflow gradient – more obstruction – murmur is louder longer and peak late in systole LVOT obstruction and systolic murmur increased by………. • A reduction in LV cavity volume and pressure ( less preload) • A decrease in systemic vascular resistance / arterial pressure ( less after load ) • An increase in LV contractility • Converse is also true Anterior Mitral Leaflet Myocardial Contractility Exercise Cathecolamines Digitalis Ventricular Volume Valsalva Standing Nitroglycerine Tachycardia Gradient / Murmur Per Arterial Pressure Methoxamine Sustained Handgrip Passive Leg Raise BV Expansion Gradient / Murmur ECG • • • • Abnormal in 90-95 % patients LVH LAE Deep and narrow q waves in inferolateral leads • Diminished R waves in lateral precordial leads • Large negative precordial T waves • Left axis deviation • No ECG finding is predictive of future events • Tall R and deep S waves weakly corelated with magnitude of LV hypertrophy • • • • SVT 46% PVCs 43% Non sustained VT 26% AF can occur in 25-30% of elderly Chest X-Ray • Mild to moderate enlargement of the cardiac silhouette. • The left ventricular contour is rounded consistent with concentric LVH. • Enlargement of the left atrium • Right-sided chambers are usually normal. Echocardiography • Gold standard for the diagnosis of HCM • Increased wall thickness in the absence of other etiology • Septum>=1.3 times LV post.free wall • Subaortic Gradient > 30mm Hg ( rest) >50(provocation) • Vigorous motion of post. Free wall with reduced septal excursion • Avg. LV wall thickness in HCM is 20- 22mm • ECG and echo has to be correlated. • Low voltages in ECG in the presence of increased wall thickness is seen in infiltrative disorder • Small LV cavity/ Septal immobility • Primary tool for defining the presence and severity of LVO tract obstruction • Systolic anterior motion of mitral valve • Presence and severity of MR (laterally and posteriorly directed jet in mid to late systole) Cardiac MRI • Subaortic gradient >30 is a determinant of heart failure but risk of sudden death • Elderly patients are not targeted for risk stratification(SCD is uncommon and survival to old age itself suggests low risk) • Beta myosin heavy chain and trop T mutations are assoc. with higher risk for premature death. Management Prevention of SCD • ICD implantation – as primary prevention following cardiac arrest -as secondary prevention if one or more high risk factors • Empirical pharmacological therapy with amiodarone is now obsolete Medical treatment Heart failure • Beta blockers (slows heart rate, reduce force of LV contraction, augments ventricular filling and relaxation, decreases myocardial O2 demand, blunts outflow gradient triggered by sympathetic activity) • Verapamil (improves LV relaxation and filling) • Disopyramide • End stage failure –ACE ,ARBs, ICD to prevent SCD • Atrial fibrillation- most common sustained arrhythmia in HCM • Paroxysmal AF occurs in 20% • Increases with age and is related to LA dilatation • Acute decompensation- cardioversion • Amiodarone prevents reccurences • Rate control with beta blockers or verapamil • Started on anticoagulation Diuretics…………….. • Can be use alone judiciously or with betablockers / verapamil to lessen pulmonary congestion Non medical treatment Surgery • Severe drug refractory heart failure symptoms • Severe functional disability (NYHA class III , IV) • Associated with LV outflow obstruction at rest or with physiological exercise (>50mm gradient) • Transaortic ventricular septal myectomy (morrow procedure)-small portion from basal septum Alcohol ablation • 96-98 % ethanol (1-3 ml)introduced into major septal perforator vessel • Necrosis and permanent MI in proximal septum is created • Thinning and reduced excursion of septum, Outflow tract enlarges- reduction of subaortic obstruction and MR • alternative treatment strategy for selected patients— (advanced age, significant comorbidity and increased operative risk, without access to expert surgical centers, or pt.against surgical intervention) Alcohol ablation • Dual chamber pacing – no definite evidence Infective endocarditis • Vegetations most commonly seen on anterior mitral leaflet or septal endocardium at the site of mitral valve–septum contact • standard antimicrobial prophylaxis is indicated prior to dental or surgical procedures Thank you