* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Skin Anatomy
Survey
Document related concepts
Transcript
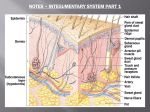
1 These are just some of the “every day” questions that are explained by skin anatomy. 2 The integument (skin, cutaneous membrane) includes two general layers of tissue. The more superficial layer, exposed to the outside environment, is the epidermis. Just deep to the epidermis is the dermis. In the micrograph above, the epidermis includes both the lavender-stained tissue (the keratinized stratum corneum) and the dark purple-stained tissue. The dermis is the pinkstained tissue underneath. Notice that the dermis has finger-like projections (called dermal papillae) that push deep into the epidermis. Normally, the epidermis and the dermis are tightly connected by a special kind of desmosome called a hemidesmosome, but when the skin is subjected to a lot of rubbing, the hemidesmosomes can break and the layesr can separate. When this happens, a “pocket” is formed and fills with interstitial fluid. This is how a blister forms. The skin is not just a flat sheet of cells that covers the body. It has lots of structures, called accessory organs, embedded in it. Some of the structures include hair follicles (with hairs), cutaneous exocrine glands (three types), nerve endings for pressure, temperature and pain, and nails. Since the skin is the boundary between our body and the outside world, the skin serves many functions that help us maintain homeostasis. The functions are summarized on the next slide. 3 The one thing I don’t like about this table is that it includes temperature regulation as a type of protection – that’s a confusing way to think about temperature regulation. It’s much better to consider temperature regulation as a separate function. Protection. The skin protects underlying tissues from damage in several ways: it protects against bumps and abrasions (mechanical damage), against chemical damage (such as acids, bases and oxidizers), against invasion by bacteria and other pathogens, against ultraviolet radiation and against water loss. The table above describes what specific features of the skin play a role in each of these types of protection. Temperature regulation. The skin helps protect us against both overheating and heat loss, as appropriate. When we become too warm, the sweat glands become active and secrete sweat (mostly water) onto the surface of our bodies. The evaporation of sweat absorbs heat energy from the body. When we’re too cold, two things happen: 1) arrector pili muscles contract, which causes our hair to “stand on end.” This traps a layer of warmed air close to our skin that helps insulate against the colder air around it. 2) Blood vessels in the skin constrict, reducing the flow of blood to the body’s surface. This helps keep the blood from getting close to the cold surface of the body and radiating its heat away. Excretion. Besides water, sweat includes some waste products that are excreted from the body. In particular, some salts as well as some byproducts of ammonia breakdown are excreted in small amounts in the sweat. Vitamin D production: When the skin is exposed to sunlight, energy is provided that catalyzes the conversion of certain precursors (made in the kidney) into vitamin D. If we get enough sunlight exposure, our skin can make all the vitamin D our bodies need! If not, though, we get vitamin D in foods we eat, too. 4 The superficial tissue of the skin is the epidermis. It consists of stratified squamous tissue and, like all epithelium, is avascular (it has no blood vessels). The deeper cells in the epidermis get oxygen and nutrients, though, because they lie close to the dermis, which does have a blood supply. All new epidermal cells are formed at the very deepest layer of the epidermis (called the stratum basale). As new cells are formed, they push the older cells up closer to the surface. As the cells are pushed towards the skin’s surface, they undergo a process called keratinization – a tough, waterproof protein called keratin is produced inside the cell and the cell fills up with keratin. By the time the skin cells (keratinocytes) reach the surface, they are completely filled with keratin and have died because they are so far from a blood supply. As the cells undergo keratinization, they are usually still attached to one another by desmosomes. Even when the cells die, they are still attached. Once the desmosomes break in the dead outer layers, though, the cells flake off, forming dandruff and dust. 5 Depending on the type, the epidermis has either 4 or 5 strata (layers): •The deepest layer (lying directly over the dermis) is the stratum basale. Since this stratum is so close to the dermis (and blood), these cells are living and can undergo cell division. In fact, the stratum basale is the only place where new skin cells are formed. As new cells are formed, they push the older cells up closer to the surface. •The stratum spinosum is several cells thick and includes cells that are still living, but undergoing keratinazation. The cells in this stratum appear more-orless round under a microscope. Stratum spinosum cells do not divide. •The stratum granulosum contains cells that are beginning to flatten as they are pushed up towards the dead cells of the most superficial layers. These cells continue to undergo keratinazation. •Finally, the stratum corneum consists of several layers of dead, fullykeratinized cells. Because these cells no longer have cytoplasm or organelles, they look very different under the microscope. In fact, they just look like a bunch of wavy fibers. The cells are still connected by desmosomes, though. •In addition, thick skin (found in the palmar and plantar regions) contains another layer. The stratum lucidum of thick skin is found between the stratum granulosum and the stratum corneum and looks like a thin layer of clear cells under the microscope. In addition to having a stratum lucidum, thick skin is noteworthy because it does not have any hair follicles. 6 Examine this micrograph carefully and note the visual differences between the epidermal strata. Identify the stratum basale, stratum spinosum, stratum granulosum and stratum corneum. 7 Identify the epidermal strata in this micrograph, too. 8 Cells in the stratum corneum are still attached by desmosomes, forming a thick, waterproof “sheet” over the skin. When these desmosomes break, though (because of movement, abrasion, etc.), the dead cells of the stratum corneum flake off. If the flakes consist of many cells and are large enough to see, we call them dandruff. Long-term rubbing of the epidermis can cause the stratum corneum to become thicker and harder to protect underlying tissues better. When this happens, a callus has formed. 9 Most of the cutaneous membrane is dermis, which directly underlies the epidermis. 10 The dermis contains most of the anatomical structures associated with the skin: cutaneous glands, hair follicles, nerve endings for pressure, temperature and pain, blood vessels, lymphatic vessels, smooth muscles. 11 The dermis has two distinct layers to it. The more superficial layer, which lies directly under the epidermis, is called the papillary layer. It’s called this because the dermis here has several “bumps” called dermal papillae that press into the epidermis. The dermal papillae contain blood vessels, nerve endings, or both. Since the epidermis doesn’t have any blood vessels, this is one way to get blood to as many epidermal cells as possible. Also, since the dermal papillae rise very near the surface of the skin, it makes a good place to put the sensory receptors for light touch (called Meissner’s corpuscles). On the fingertips and the bottoms of the feet, the dermal papillae are lined up and form “ridges” in the epidermis, which are easily visible from the outside. On the fingertips, these are our fingerprints, which give the fingers tread and help us grip things. On the bottoms of the feet, these help keep us from slipping when barefoot. The deeper layer of the dermis is the reticular layer. 12 When the skin stretches excessively, the reticular layer can become damaged. If the damage is repaired by granulation tissue, stretch marks (striae) may be visible from outside. Stretch marks often form in pregnant women because the skin in the abdominal region stretches faster than it can grow. Stretch marks fade over time, but they usually do not go completely away. The pictures on this slide show stretch marks in a pregnant woman (left) and in a bodybuilder who used steroids (right). 13 Identify the dermal papillae in this micrograph. What would you find in the dermal papillae? Identify the papillary layer and the reticular layer. Finally, identify each epidermal stratum. 14 These drawings show hair follicles (which are pockets where the epidermis is sort of “pushed in” to the dermis). In the left figure, identify the epidermis, dermis and hypodermis. In the right drawing, identify each of these and see if you can point out the stratum corneum. 15 The hypodermis is not a part of the skin. It sits under the skin and anchors it to underlying muscle, bone or cartilage. The hypodermis consists of a mix of areolar and adipose tissue. The adipose tissue makes up our body fat (the fat that people are always trying to lose). This accounts for about 50% of the adipose tissue in the body. Most of the rest is visceral fat, which surrounds and cushions most of the body’s internal organs. 16