* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Biology 231
Embryonic stem cell wikipedia , lookup
Cell culture wikipedia , lookup
Chimera (genetics) wikipedia , lookup
Microbial cooperation wikipedia , lookup
State switching wikipedia , lookup
Hematopoietic stem cell wikipedia , lookup
List of types of proteins wikipedia , lookup
Nerve guidance conduit wikipedia , lookup
Neuronal lineage marker wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Organ-on-a-chip wikipedia , lookup
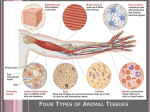
VT 105 Comparative Anatomy and Physiology Tissues TISSUES – group of similar cells with a common function Histology – study of tissues Pathologist – doctor who examines tissues for changes in structure indicating disease processes Biopsy – removal of tissue for pathological examination techniques – needle biopsy, surgical biopsy 3 primary germ layers – first tissues of embryo ectoderm – dorsal layer mesoderm – middle layer endoderm – ventral layer 4 Basic Tissue Types: nervous tissue – from ectoderm muscle tissue – from mesoderm connective tissue – from mesoderm epithelial tissue – from all 3 layers depending on location Cell Junctions – contact points between cells that bind them together into a functional unit, form seals between cells, anchor cells in place, provide channels for communication between cells Tight junctions – web of membrane proteins on adjacent cells fuse together forming a watertight seal (eg. cells lining digestive tract) Desmosomes – plaque (dense area of proteins) on membrane with cell adhesion molecules desmosones of adjacent cells attach to each other like velcro intermediate filaments link desmosomes to cytoskeleton of cell contributes strength and stability to tissues Hemidesmosomes – similar to desmosomes, but attach epithelial cells to a basement membrane Gap junctions – membrane proteins of adjacent cells bind together forming channels between cells certain particles can diffuse from one cell to the other, allowing intercellular communication 1 Neural Tissue – detects changes in internal and external environment and responds by transmitting signals to other tissues to maintain homeostasis or cause a response 2 cell types: neurons – detect stimuli, create nerve impulses; composed of a cell body, with fibrous processes neuroglia – support neurons Muscle Tissue – use ATP to contract; cause body movements 3 muscle types: Skeletal muscle – usually attaches to bone striated (striped) appearance under microscope very long, multinucleate cells contractions are voluntary Cardiac muscle – heart muscle branched, striated cells with 1 nucleus intercalated discs – junctions between cells with gap junctions contractions are involuntary Smooth muscle – walls of hollow organs and vessels spindle-shaped with 1 central nucleus and no striations contractions are involuntary EPITHELIAL TISSUE sheets of epithelial cells held together by cell junctions; anchored to a basement membrane basement membrane – fibrous layer which anchors epithelium to underlying connective tissue composed of protein fibers and adhesion proteins secreted by epithelium and underlying connective tissue Functions of Epithelial Tissues cover and line surfaces protect surfaces and deeper tissues sites of excretion, absorption, or gas exchange some modified to detect sensations form glands produce secretions 2 Polarity of Epithelial Cells – they have directionality basal surface – cell surface which adheres to basement membrane via hemidesmosomes (basal layer = deepest layer) apical surface – cell surface opposite basal surface; faces body surface, body cavity, or lumen of organ or duct (apical layer = most superficial layer) lateral surfaces – face adjacent cells and are attached by various cell junctions epithelium is avascular (no blood vessels) so nutrients and wastes diffuse to and from epithelium from blood vessels in connective tissue beneath CLASSIFICATION OF EPITHELIUM by number of cell layers: simple epithelium – single layer of cells stratified epithelium – 2 or more layers of cells pseudostratified epithelium – 1 layer that appears multilayered classification by cell shapes: squamous – flat; nucleus in center cuboidal – cubes or hexagons; nucleus in center columnar – height greater than width; nucleus at base transitional – shape varies due to tissue stretching (flat to cuboidal) by cell modifications: cilia – hair-like microtubule structures on apical surface function in sweeping mucus and other materials on surface (eg. upper respiratory tract, uterine tubes) microvilli – finger-like extensions of cell membrane on apical surface increase surface area for absorption or secretion (eg. small intestine, kidney tubules) TYPES OF EPITHELIUM simple squamous – smooth, single, flat layer mesothelium – lines body cavities and viscera endothelium – lines inside of blood vessels gas exchange surfaces of lungs stratified squamous – many layers, apical layer is flat lines surfaces exposed to damaging environment (especially abrasion) skin, mouth and esophagus, vagina, anus simple cuboidal – single cuboidal layer sites of secretion and absorption many glands, kidney tubules may have cilia or microvilli 3 stratified cuboidal – 2 or more cuboidal layers lining large ducts of glands simple columnar – single columnar layer thickness provides some protection capable of secretion and absorption lining digestive tract, uterine tubes may have cilia or microvilli stratified columnar – multiple layers, apical layer is columnar protective and secretory rare pseudostratified ciliated columnar lines most of respiratory airways has goblet cells which produce mucus traps and sweeps debris out of airways transitional – found in urinary bladder and ureters variable number of layers and shape of apical layer depending on fullness of organ full – stretches out; appears squamous with fewer layers empty – not stretched; appears cuboidal to round with more layers GLANDS – epithelia that produce secretions; most invaginate to form clusters of cells beneath the covering layers of epithelium exocrine glands – secrete into ducts that empty onto covering or lining epithelium (eg. mucus, sweat, saliva) endocrine glands – ductless glands which secrete (hormones) into interstitial fluid, from which it diffuses into bloodstream Structural classification of glands: multicellular glands – multiple cells simple, branched, compound tubular – tube-shaped acinar – sac-like unicellular glands – 1 cell goblet cells – modified columnar epithelial cells secrete mucus for lubrication and protection (eg. upper respiratory tract, digestive tract) Functional classification of glands – how secretion is released merocrine glands – most common type; secretory vesicles containing product empty via exocytosis (eg. salivary glands) holocrine glands – product accumulates in cytoplasm and is released as cell ruptures (eg. sebaceous glands) apocrine glands – product accumulates in apical region of cell and cell pinches of apex to release (mammary glands) 4 CONNECTIVE TISSUE connects, supports, and protects body and organs; store energy, provide immunity, allow transport of materials between tissues most have a rich vascular supply 2 Basic Components of Connective Tissue 1) Specialized Cells – all derived from embryonic mesoderm variety of cells types depending on specific tissue fixed cells – remain in a specific connective tissue wandering cells – come and go in many types of tissues leukocytes – white blood cells mast cells – inflammatory cells macrophages – tissue phagocytes 2) Matrix – extracellular material (outside of cells) protein fibers and ground substance secreted between cells by –blast cells matrix determines a tissue’s physical characteristics Protein Fibers – fibrous proteins; strengthen and support matrix collagen fibers – thick, strong white fibers resistant to stretch, but flexible made of collagen protein (25% of body protein) (plentiful in bone, cartilage and tendons) reticular fibers – collagen proteins form thin, branching networks forming a framework to support soft organs such as liver and spleen elastic fibers – contain the protein elastin strong but elastic (can be stretched but returns to original shape) (found in lungs, skin, blood vessels) Ground substance – amorphous materials secreted between cells and fibers; supports and binds cells and fibers determines consistency of tissue (liquid, gel, solid) water – major component in all ground substance 5 glycosaminogycans (GAGs) - trap water molecules to form a gel hyaluronic acid – viscous, slippery substance chondroitin sulfate – thick gel mineral salts – form solid matrix mostly calcium and phosphates TYPES OF CONNECTIVE TISSUES Embryonic Connective Tissue mesenchyme – relatively undifferentiated mesoderm gives rise to all adult connective tissues mesenchymal cells; soft gel ground substance, delicate reticular fibers ADULT CONNECTIVE TISSUES Connective Tissue Proper Loose Connective Tissue – many cells with loosely arranged matrix areolar connective tissue – most common; least specialized “packing material”; cushions and supports organs main fixed cells – fibroblasts – large, branched cells that secrete the matrix many wandering cells fibers – collagen, elastic, and reticular ground – soft gel (found in subcutaneous (subQ) layer beneath skin) adipose connective tissue – fatty tissue stores energy, insulates, and cushions organs main fixed cells – adipocytes – round cells filled with large fat droplets white fat – main type in adults brown fat – newborn and hibernating animals rich blood supply and mitochondria; generates heat reticular connective tissue – reticular fibers and fibroblast cells forms stroma (network) which supports soft organs (liver, spleen, lymph nodes) 6 Dense Connective Tissue – many thick fibers and fewer cells and matrix connect body structures and resist stress dense regular connective tissue – bundles of parallel collagen fibers, all running in the same direction fibroblasts between bundles very resistant to stretch in 1 direction, (eg. tendons) dense irregular connective tissue – many, irregularly woven collagen fibers, with fibroblasts resists pulling forces in multiple directions (eg. joint capsules, skin) elastic connective tissue – branching elastic fibers with fibroblasts between allows stretching but returns to original shape (eg. lungs, arteries, vocal cords) Specialized Connective Tissues Cartilage – rigid, yet flexible matrix – dense fiber network in thick gel ground fixed cells chondroblasts – immature cells that secrete matrix chondrocytes – mature cells trapped in matrix lacunae – spaces within matrix where cells live perichondrium – dense irregular c.t. membrane covering surface of most cartilage hyaline cartilage – most common (eg. joint surfaces, nose, trachea, fetal skeleton) fine collagen fibers in a firm gel ground numerous chondrocytes provides support with some flexibility, reduces friction, absorbs shock fibrocartilage – dense bundles of collagen in thick gel ground few chondrocytes; no perichondrium very tough to absorb shock (eg. intervertebral discs, menisci [pads] of stifle) elastic cartilage – thread-like network of elastic fibers in gel ground with chondrocytes strong but flexible (eg. ear, epiglottis) 7 Growth and Repair of Cartilage no vascular supply (blood vessels); growth and repair are very slow in adults Bone (Osseous) Tissue – supports of skeleton stores calcium and phosphorus matrix – numerous collagen fibers in mineral salt ground main fixed cells – osteocytes within lacunae periosteum – dense irregular c.t. membrane covering bone surface Blood – fluid connective tissue blood plasma – fluid matrix composed of water with solutes red blood cells (erythrocytes) – carry oxygen to cells and carbon dioxide away white blood cells (leukocytes) – involved in phagocytosis, immunity, and inflammation platelets (thrombocytes) – involved in blood clotting Lymph – mainly fluid; variable cell and solute content MEMBRANES – flat, pliable sheets of tissue; cover or line a body part Epithelial Membranes – composed of epithelium and underlying connective tissue Mucous membranes (mucosa) – line body cavities open to the exterior (eg. digestive, respiratory, reproductive tracts) protective barrier against pathogens, chemicals, and physical injury secrete mucus - stops desiccation, lubricates, traps foreign material may function in absorption or secretion of other products may have cilia, microvilli, and goblet cells lamina propria – areolar connective tissue layer Serous membranes (serosa) – line body cavities not open to the exterior and cover organs within cavities areolar connective tissue covered by mesothelium (simple squamous epithelium) 2 layers – parietal layer covers wall & visceral layer covers organs (eg. pleura, peritoneum, pericardium) serous transudate (watery fluid) lubricates surfaces reduces friction and prevents adhesions Cutaneous membrane – skin (next lecture) 8 Connective Tissue Membranes – composed of connective tissues, no epithelium Synovial membranes – line joint spaces, bursae and tendon sheaths areolar connective tissue with connective tissue cells secrete synovial fluid – thick, viscous fluid which lubricates articular cartilage Meninges – cover and protect brain and spinal cord TISSUE REPAIR Regeneration – reconstruction of injured tissue by parenchymal cells (functioning part of tissue or organ) – fully functional repair stem cells – undifferentiated cells in parenchyma that divide and differentiate to replace cells some tissues don’t regenerate well (eg. muscle, nervous tissue) Fibrosis – repair of injured tissue by fibroblasts (scarring) replace parenchyma with connective tissue (not functional) 9