* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download L 1 Characters_Mechanisms_Pituitary Final
Hormonal contraception wikipedia , lookup
Mammary gland wikipedia , lookup
Triclocarban wikipedia , lookup
Endocrine disruptor wikipedia , lookup
Menstrual cycle wikipedia , lookup
Xenoestrogen wikipedia , lookup
Breast development wikipedia , lookup
Neuroendocrine tumor wikipedia , lookup
Hyperandrogenism wikipedia , lookup
Hormone replacement therapy (menopause) wikipedia , lookup
Adrenal gland wikipedia , lookup
Hormone replacement therapy (male-to-female) wikipedia , lookup
Bioidentical hormone replacement therapy wikipedia , lookup
Graves' disease wikipedia , lookup
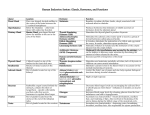
Endocrine System Lecture 1 Characters and mechanisms of actions of hormones Pituitary hormones Asso. Professor Dr Than Kyaw 17 September 2012 What is endocrinology? Endocrinology Study of: - Intercellular Chemical Communication - about communication systems & information transfer. Hormones Definition (classical) - Chemical substances produced by specialized ductless glands - Released into the blood - Carried to other parts of the body - Produce specific regulatory effects. Is that definition true? PGF2α - produced by most of the body cells, transmitted by diffusion in interstitial fluid rather than by circulation in the blood. Pheromones – transmission through olfaction (smell) -- outside the body Modes of transmission Hormone transmission restricted only to blood – incorrect 1. Epicrine transmission - Hormones pass through gap junctions of adjacent cells without entering extracellular fluid. 2. Neurocrine transmission - Hormones diffuse through synaptic clefts between neurons. Neural – through neurons (neurotransmitters) Gap junctions - Pores connecting adjacent cells. Small molecules and electrical signals in one cell can pass through the gap junctions to adjacent cells. Synaptic cleft - Between a neuron and a muscle fiber or - Between 2 neurons - Acetylcholine Mode of transmission 3. Paracrine transmission - Hormones diffuse through interstitial fluid - PGF2α 4. Endocrine transmission - Hormones are transported through blood circulation. - Typical of most hormones 5. Exocrine transmission - Hormones are secreted to the exterior of the body. E.g - Somatostatin secreted into the lumen of GI tract (and inhibit intestinal motility and absorption) - Pheromones Endocrine Functions • • • • • Maintain Internal Homeostasis Support Cell Growth Coordinate Development Coordinate Reproduction Facilitate Responses to External Stimuli Elements of an endocrine system • • • • • • • • Sender = Sending Cell (where hormone is produced) Signal = Hormone Nondestructive Medium = Serum & Hormone Binders Selective Receiver = Receptor Protein (Target cells) Transducer = Transducer Proteins & 2º Messengers Amplifier = Transducer/Effector Enzymes Effector = Effector Proteins Response = Cellular Response What are transducers? Transducers - proteins that convert the information in hormonal signals into chemical signals understood by cellular machinery. - They change their shape & activity when they interact directly with protein-hormone complexes. - Usually enzymes or nucleotide binding proteins, they produce 2nd messengers, or change the activity of other proteins by covalently modifying them (adding or removing phosphate, lipid groups, acetate, or methyl groups), or they interact with other proteins that do these things. - They begin amplifying the energy content of the original hormone signals. Classes of hormone 1. Amine hormones - thyroid hormones, catecholamines - all derived from single amino acids - thyroid hormones - from tyrosine - catecholamines - from tyrosine - melatonin - from tryptophan Classes of hormone 2. Peptide hormones - Peptides, polypeptides and proteins - Hydrophilic/Lipophobic - short half life - hormones of hypothalmus (releasing and inhibiting) - pituitary hormones - Insulin, glucagon Classes of hormone 3. Steroid hormones - adrenocortical and reproductive hormones - derived from cholesterol - Hydrophobic/lipophilic - long half life - travel with a protein carrier - bind to cytoplasmic/nuclear receptor Classes of hormone 4. Eicosanoids (Lipid hormones) - produced from 20 carbon fatty acids (arachidonic acid) - produced in all cells except RBCs - prostaglandin, leukotrienes (smooth m/s contraction in trachea), thromboxanes Hormone Interactions Responsivenss of a target cell to a hormone depends on: - The hormone concentration - The abundance of the target cell’s hormone receptors - influences exerted by other hormones 1. Permissive effect: when the action of a hormone on target cells requires a simultaneous or recent exposure to a second hormone. - e.g: Epinephrine – alone, weakly stimulates lipolysis but presence of a small amounts of thyroid hormones - the same amount of epinephrine stimulates lipolysis much more powerfully. Hormone Interactions 2. Synergistic effects when the effect of two hormones acting together is greater or more extensive than the sum of each hormone acting alone 3. Antagonistic effects when one hormone opposes the activation of another hormone. E.g, Insulin promotes glycogen synthesis by the liver cells and glucagon stimulates glycogen breakdown Enzyme amplification - One hormone molecule does not trigger - the synthesis of just one enzyme molecule - It activates thousands of enzyme molecules through a cascade of called enzyme amplification - This enables a very small stimulus to produce a very large effect - Hormones are therefore needed in very small quantities - circulating concentration very low compared to other blood substances: on order of nanograms per deciliter of blood - Because of amplification target cells do not need a great number of hormone receptors Hormone clearance - Hormone signals, like nervous signals, must be turned off when they have served their purpose - Most hormones are taken up and degraded by the liver and kidneys and then excreted in bile or urine - Some are degraded by the target cells - Rate of hormone removal (metabolic clearance rate – MCR) - Halflife – the length of time required to clear 50% of the hormone from the blood - the faster the MCR – the shorter half life Metabolic Clearance Rate or Half-life of some hormones Hormone Half-life Amines 2-3 min Thyroid hormones: T4 T3 6.7 days 0.75 days Polypeptides 4-40 min Proteins 15-170 min Steroids 4-120 min Modulation of target cell sensitivity - Hormones affect only target cells - cells that carry specific receptors that bind the recognized hormone - Down regulation: when receptor quantity decrease when hormone is in excess - Decreases responsiveness to hormone for example, in response to obesity when cells become less sensitive to insulin. - Up regulation: when receptor quantity increases when hormone is deficient - Make target cell more sensitive to hormone for example, in response to regular exercise when cells become more sensitive to insulin. Hormone receptors (Cell surface receptor, membrane receptors, transmembrane receptors) - Cellular proteins that bind with high affinity to hormones & are altered in shape & function by binding. - exist in limited numbers. - Binding to hormone is noncovalent & reversible. - Hormone binding will alter binding to other cellular proteins & may activate any receptor protein enzyme actions. Hormone & Receptor in General Hormone receptors - Specialized integral membrane proteins - Communication between the cell and the outside world. - Extracellular signalling molecules (usually hormones, neurotransmitters, cytokines, growth factors or cell recognition molecules) - Attach to the receptor, trigger changes in the function of the cell. - This process is called signal transduction: The binding initiates a chemical change on the intracellular side of the membrane. In this way the receptors play a unique and important role in cellular communications and signal transduction. G Protein Any of a class of cell membrane proteins that function as intermediaries between hormone receptors and effector enzymes and enable the cell to regulate its metabolism in response to hormonal changes. 2 Types -- Stimulatory (GS) -- Inhibitory (GI) Surface Hormone Receptors 4 types or 4 domains of Surface hormone receptors 1. Seven-transmembrane domain receptors - β adrenergic - Parathyroid hormones (PTH) - Luteinizing hormone (LH) - Thyroid-stimulating hormone (TSH) - Growth hormone-releasing hormone (GHRH) - Thyrotropin releasing hormone (TRH) - Adrenocorticotropic hormone (ACTH) - MSH (melanocyte-stimulating hormone) Surface Hormone Receptors 2. Single transmembrane receptors - Insulin - Insulin like growth factor I (IGF I) - Epidermal growth factor (EGF) - Platelet derived growth factor (PDGF) 3. Cytokine receptor super family - GH, Prolactin, - Erythropoietin - Interleukin - Leptin 4. Guanyl cyclase –linked receptor - Natriuretic peptide 1. A seven-transmembrane domain receptor 2. A single-ransmembrane domain receptor with kinase activity typical of many growth factors 3. Receptors with no intrinsic tyrosine kinase activity but activation by soluble transducer molecules. 4. Receptors dependent on guanylyl cyclase or adenylyl cyclase and synthesis of cGMP and cAMP. G protein-linked hormone mechanism Activation of receptor induced by binding of the hormone (1st messenger). Cytoplasmic tail of receptor activates G protein The activated G protein complex links to 2nd messenger which is responsible for the effect associated with hormone action Second messenger systems cyclic AMP - Hormone travels in blood plasma - Hormone binds to its receptor in the plasma membrane GPCR (G-protein coupled receptor) - Hormone-receptor binding activates a G protein (in plasma membrane) - Activated G protein in turn activates the enzyme adenyl cyclase - Adenyl cyclase causes ATP to lose two P, becoming cAMP (cyclic AMP [adenosine monophosphate]) - cAMP activates protein kinases (enzymes that activate other proteins/enzymes), producing the hormonal effect Hormones and their receptors by classifying water soluble and lipid soluble Hormone Class of hormone Location Amine (epinephrine) Water-soluble Cell surface Amine (thyroid hormone) Lipid soluble Intracellular Peptide/protein Water soluble Cell surface Steroids and Vitamin D Lipid Soluble Intracellular Endocrine glands of animals Hypothalamus and Pituitary gland (hypophysis cerebri) Hypothalamic releasing hormones Hypothalamic releasing hormone Effect on pituitary Corticotropin releasing hormone (CRH) Thyrotropin releasing hormone (TRH) Growth hormone releasing hormone (GHRH) Somatostatin Stimulates ACTH secretion Gonadotropin releasing hormone (GnRH) a.k.a LHRH Prolactin releasing hormone (PRH) Prolactin inhibiting hormone (dopamine) Stimulates TSH and Prolactin secretion Stimulates GH secretion Inhibits GH (and other hormone) secretion Stimulates LH and FSH secretion Stimulates PRL secretion Inhibits PRL secretion Putuitary gland = Master gland - Because pituitary gland produces many hormones –k/s master gland - Pituitary extracts – obtained from pituitary glands from slaughter houses - Laborious and low yields - 340 g/100 cattle; 30 g/100 pigs - Pituitary extracts are used for research or commercial purposes Pituitary gland (hypophysis cerebri) - Anterior lobe (adenohypophysis) - Posterior lobe (neurohypophysis) Location of the pituitary gland - Just below the hypothalmus - Provide direct delivery of releasing and inhibiting hormones from the hypothalmus to the anterior lobe - direct entry of secretory neurons from the hypothalmus to posterior lobe - Hypophysioportal circulation The venous blood drained from the hypothalmus is redistributed by another capillary system within the anterior lobe. Shortages of hormones in arterial blood are directed by specific cells within the hypothalmus, which are stimulated to secrete releasing hormones. The hormones produced are distributed by the second capillary bed to their appropriate cells in the anterior lobe. Anterior Pituitary Hormone A c r o n y m Hypop hysial Cell Type Hypothalamic Regulator(s) Hormonal Function(s) Corticotropin , Adrenocortic otropin A C T H Cortic otrope +Corticotropin Releasing Hormone, Corticoliberin (CRH); + Interleukin 1 ; Glucocortical Steroids (via CRH); + Vasopressin Stimulates glucocorticoid production by adrenal fasiculata & reticularis Thyrotropin, Thyroid Stimulating Hormone T S H Thyrot rope -Thyroxine (T4); +Thyroid Releasing Hormone, Thyroliberin (TRH); -Somatostatin (SS) Stimulates thyroxine production by thyroid Prolactin, Mammotropi n, Luteotropin P R L -Dopamine; + TRH; - SS; + Estrogens; + Oxytocin Stimulates milk synthesis by secretory epithelium of breast; supports corpus luteum function Somatotropin , Growth Hormone G H Lactot rope; Mam motro pe Somat otrope + Growth Hormone Releasing Hormone, Somatoliberin (GHRH); - SS Stimulates somatic growth, supports intermediary metabolism Follitropin, Follicle Stimulating Hormone F S H Gona dotro pe + Gonadotropin Releasing Hormone, Luteinizing Hormone Releasing Hormone, Gonadoliberin (GnRH, LHRH); - Inhibin; - Sex steroids (via LHRH) Supports growth of ovarian follicles & estradiol production; Supports Sertoli cell function & spermatogenesis Lutropin, Luteinizing Hormone L H Gona dotro pe + GnRH (LHRH); - Sex steroids (via LHRH); + Estradiol in near midcycle Supports late follicular development, ovulation, & corpus luteum function (especially progesterone synthesis); Supports testosterone synthesis, Leydig cell Melanotropin, Melanocyte Stimulating Hormone M Melan S otrope H + CRH Supports dispersal & synthesis of pigment in melanocytes; may alter adrenal response to ACTH STIMULUS Hypothalamus Releasing Hormone (Release-Inhibiting Hormone) Pituitary Stimulating Hormone Gland Hormone Target Anterior Putuitary Hormones Regulated by: Releasing Hormones and Inhibiting hormones of hypothalmus Cells of anterior pituitary and hormones 5 cell type; 7 hormones 1. Somatotrope cells (Growth ormone) 2. Corticotrope cells (adrenocorticotropic hormone and beta-lipotropin hormone) 3. Mammotrope cells (prolactin) 4. Thyrotrope cells (thyroid stimulating hormone) 5. Gonadotrope cells (Follicle stimulating hormone and luteinizing hormone) Nature of anterior pituitary hormones - Polypeptides to large proteins - Different structures among species - Replacement therapy from one spp to another not uniformly successful Growth hormone (GH) - Somatotropic hormone (STH) Stimulatory effect of increase in body size Growth of all tissues of the body Both cell numbers and cell size Epiphyseal bone plates are more sensitive to GH Increases mitotic activity Stimulate the liver to form several small proteins, somatomedins (Insulin-like growth factors 1 and 2, IGF 1 and IGF2) - Somatomedins act on cartilage and bone growth. Therefore bone and cartilage are not stimulated directly by GH but indirectly by this intermediate compound. GH - Several specific metabolic effects - because of this, GH is necessary throughout life Metabolic effects - Increases - rate of protein synthesis in all body cells - mobilization of fatty acids from fat - use of fatty acids for energy - Decreased rate of glucose uptake throughout the body - Use of fats for energy conserves glucose and promotes glycogen storage – the heart can endure emergency contraction more effectively whereby glycogen stored in the heart is converted to glucose. GH Milk production - Increasing milk yield in lactating cows by growth hormone is not stimulation on mammary gland but by partitioning of available nutrients from body tissues towards milk synthesis Abnormal GH production Excessive production of GH Before puberty: – increase growth of long bones (prolonged proliferation of growth plate chondrocytes) After puberty – closure of epiphyseal plates - acromegaly - enlargement of extremities and facial bones Gigantism – frequently seen in human Failure to produce sufficient GH – stunted growth - dwarfism Adrenocorticotrophic hormone (ACTH) - Increase activity of the adrenal cortex - Glucocorticoids and mineralocorticoids (aldosterone ) secretion - Similar effects of somatotropic hormone (STH) - ↑protein synthesis - ↑fatty acid uptake - ↓ glucose uptake Thyroid stimulating hormone (TSH) - Stimulate - Synthesis of colloids by thyroid gland - Release of thyroid hormone - Associate functions - accumulation of iodine - organic binding of iodine - formation of thyroxine within the thyroid gland - No extrathyroid activity as for STH and ACTH. Gonadotropic hormones and prolactin - Follicle stimulating hormone (FSH) and luteinizing hormone (LH) have specific roles in male and female reproduction - FSH stimulates oogenesis and spermatogenesis - LH assists ovulation and development of functioning corpus luteum in female - LH stimulates secretion of testerone in male - Prolactin helps to initiate and maintain lactation after pregnancy - Maintenance of CL in ewe Beta-lipoprotein hormone (β-LPH) - Secreted by adrenocorticotropic cells - Exact physiologic role unknown - Assumed to be involved in the pain relief and response to stress. Posterior Pituitary Posterior pituitary and its hormones - An outgrowth of hypothalmus - Contains terminal axons from two pairs of nuclei - supraoptic nucleus and paraventricular nucleus - These nuclei synthesize - Antidiuretic hormone (ADH) - Oxytocin Neurosecretions - Transported to axon terminals in the posterior pituitary, stored in secretary granules - An action potential generated by the need for each of stored hormones causes the release of the hormone and subsequent absorption into the blood – distributed to the receptor cells - Both hormones – peptides (nona-peptides – nine amino acids) Antidiuretic hormone (Vasopressin) - Normally outloaded water of the body – excreted by diuresis (increased output of dilute urine) - Diuresis can be prevented by administration of ADH Dehydration (osmoconcentration) ↓ osmoreceptors ↓ Posterior putuitary Release of ADH ↓ ↓ Target cells (collecting tubules & Collecting ducts of kidney) Retention of water Oxytocin - Function related to the reproductive processes - Includes in parturition and laction - Neuroendocrine reflexes - Suckling by young or similar teat stimulation - Release of oxytocin - Milk letdown - Myometrial contraction at parturition - Transport of sperm in the oviduct at copulation Intermediate Lobe of Putuitary During development a transitional zone between the neurally derived posterior lobe & the epithelially derived anterior lobe forms. It is lost in adults of some species like humans but persists in others. It makes melanocortin (MSH). Negative Feedback Mechanism Simple example NEGATIVE FEEDBACK MECHANISM Decreased hormone concentration In the blood (e.g. Thyroxine) Pituitary gland Release of stimulating hormone (e.g. TSH) Stimulation of target organs to produce & (e.g. release hormone Thyroid gland release of Thyroxine) Return of the normal Concentration of hormone • Most hormonal regulatory systems work via negative feed back • Occasionally, a positive feed back system contributes of regulation - E.g. At parturition, where oxytocin stimulates contractions of the uterus and the uterus in turn stimulates more oxytocin release. Thyroid Gland and Thyroid Hormones Thyroid glands Located - on the trachea just caudal to the larynx 2 laterally placed, flattened lobes joined by isthmus No isthmus in dog and cat pig has a large medial lobe instead of isthmus Thyroid gland - composed of numerous follicles lined by simple cuboidal epithelial cells filled with fluids (colloids) Colloids - gel-like substances - consists of a protein–iodine complex, thyroglobulins - hormones T3 and T4 are stored in the colloids Bovine thyroid gland Thyroid hormones T3 = tri-iodothyronine; T4 = tetra-iodothyronine Regulation of secretion Thyrotropin-releasing hormone (TRH) from hypothalmus controls the secretion of thyroid stimulating hormone (TSH) from the anterior pituitary TSH stimulates the synthesis of thyroxine (T4) and triiodothyroxine (T3) T4 and T3 inhibit TRH by negative feedback There is no thyrotropin inhibiting hormone Regulation of secretion Thyroid hormones: Synthesis and release - Iodine containing compounds Belong to the amine classification of hormones derived from tyrosine Iodine trapping and iodination are unique features of the thyroid gland Synthesis of thyroglobulin Iodination of tyrosine Coupling of T1 and T2 to form T3 and T4 T3 and T4 are attached to the thyroglobulin in the colloids - Lysosomes - release proteolytic enzymes that separate T3 and T4 from the thyroglobulin Thyroid hormones: Synthesis and release - About 90% of thyroid hormones released is T4 - Released T3 and T4 immediately combined with plasma protein (mainly thyroxine binding globulin – TBG) for transport in the blood - TBG – greater affinity to T3 than T4 - Therefore, T3 is released more to the tissues - Once in the tissues, T3 is more potent than T4 but short duration of action Functions of thyroid hormones - Increase internal heat - increased rate of O2 consumption - Stimulate metabolic activities of most tissues of the body except brain, lungs, retina, testes and spleen - Increased metabolic activity and O2 consumption are through activation and stimulation of key enzymes - alpha glycerophosphate dehydrogenase - hexokinase - diphosphoglycerate mutase - cytochrome b and c - Thyroid hormones also markedly potentiate lipolytic effect of epinphrine - It is suggested that heat generated is secondary to protein synthesis stimulated by thyroid hormones Thyroid deficiency and antithyroid compounds Typical deficiency - Result from iodine deficiency and consequently inability of the thyroid gland to produce T3 and T4 - Lack of circulating hormones causes feedback mechanisms so that TSH is produced - This causes thyroglobulin accumulation without effective output of T3 and T4 - Thyroid gland enlarges because of colloid accumulation - a condition k/s goiter Thyroid enlargement (goiter) may be caused by - Hypothyroidism (iodine deficiency) or - Hyperthyroidism (increased thyroxine demands, tumour) - Goiter caused by iodine deficiency – rare in animals - Other causes of thyroid disfunction – relatively low in sheep, cattle and swine Hyperthyroidism – common in dogs and cats - Signs of hyperthyroidism - Fatigue - weight loss - Hunger - nervousness - sensitivity to heat - Signs of hypothyroidism - lack of activity (lethargy) - hair loss, dry and dull hair - cold sensitivity - anaemia Antithyroid compounds Goitrogens - Natural substances – inhibit thyroid function - Thyroxine is not produced in sufficient amounts and TSH continues to be secreted -- thyroglobulin accumulation Goitrin - Produced in the intestinal tract after ingestion of progoitrin containing plants (cabbage, turnip) Thiocyanate - Another goitrogen in some plants; it interferes with iodine trapping - This can be overcome by feeding excess iodine Antithyroid compounds are used in the treatment of hyperthyroidism - thiourea, thiouracil, sulphonamides, chlorpromazine - propylthiouracil or methimazole Hyperthyroidism in man Signs and symptoms - Increased heart rate - More forceful heartbeat or contractions - Increased blood pressure - Anxiety - Weight loss - Difficult sleeping - Tremors in the hands - Weakness - Bulging eyes (exophthalmos) Remember - Hyperthyroidism rare in animals except old cats and dogs Hypothyroidism in man Signs and symptoms - Weight gain Dry skin and puffy skin Constipation Cold intolerance Hair loss Fatigue and Menstrual irregularity in women. Cretinism - Congenital lack of thyroid hormone - Characterized by arrested physical and mental development Calcitonin - Produced by C cells (parafollicular cells) of thyroid gland - Peptide hormone - Lowers blood calcium level inhibiting the action of osteoclasts - Calcitonin release – Hypercalcemia (lesser degree by hypermagnesemia) – directly regulated by negative feedback of serum calcium concentration on C cells, NOT by TSH - physiological importance in overall regulation of calcium conc is minimal compared with the role of parathyroid hormones 1. Presentations 8 groups of students, each with 5 students Presentation on Week 13 1. 2. 3. 4. 5. 6. 7. 8. Hormone receptors and their regulations (G2) Hyperthyroidism and hypothyroidism (G3) Hyper- and hypo-secretion of Growth Hormone (G6) Parathyroid gland and calcium metabolism (G1) Factors that affect urine concentration (G8) Renal function tests (G7) Thyroid function test (G4) Hormonal influence on the various stages of estrous cycle (G5) 2. One Assignment Diabetes in animals before midterm break