* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Complement activation in patients with rheumatoid arthritis mediated
Behçet's disease wikipedia , lookup
Autoimmune encephalitis wikipedia , lookup
Signs and symptoms of Graves' disease wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Ankylosing spondylitis wikipedia , lookup
Neuromyelitis optica wikipedia , lookup
Management of multiple sclerosis wikipedia , lookup
Multiple sclerosis research wikipedia , lookup
Pathophysiology of multiple sclerosis wikipedia , lookup
Multiple sclerosis signs and symptoms wikipedia , lookup
Complement component 4 wikipedia , lookup
Rheumatoid arthritis wikipedia , lookup
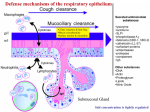
Seediscussions,stats,andauthorprofilesforthispublicationat:https://www.researchgate.net/publication/11985945 Complementactivationinpatientswith rheumatoidarthritismediatedinpartbyC‐ reactiveprotein ArticleinArthritis&Rheumatology·May2001 ImpactFactor:7.76·DOI:10.1002/1529-0131(200105)44:5<997::AID-ANR178>3.0.CO;2-C·Source:PubMed CITATIONS READS 55 34 6authors,including: EsmeraldaTHMolenaar Gerardvanmierlo GroeneHartZiekenhuis SanquinBloodSupplyFoundation 27PUBLICATIONS730CITATIONS 35PUBLICATIONS968CITATIONS SEEPROFILE Allin-textreferencesunderlinedinbluearelinkedtopublicationsonResearchGate, lettingyouaccessandreadthemimmediately. SEEPROFILE Availablefrom:Gerardvanmierlo Retrievedon:12May2016 ARTHRITIS & RHEUMATISM Vol. 44, No. 5, May 2001, pp 997–1002 © 2001, American College of Rheumatology Published by Wiley-Liss, Inc. Complement Activation in Patients With Rheumatoid Arthritis Mediated in Part by C-Reactive Protein Esmeralda T. H. Molenaar,1 Alexandre E. Voskuyl,1 Atoosa Familian,2 Gerard J. van Mierlo,2 Ben A. C. Dijkmans,3 and C. Erik Hack4 Objective. Complement activation in patients with rheumatoid arthritis (RA) is considered to be triggered by immune complexes. Recently, it was shown that C-reactive protein (CRP) can activate the complement system in vivo. We therefore hypothesized that part of the complement activation in RA is due to CRP. The aim of this study was to investigate CRP-mediated complement activation in RA, and to assess its correlation with disease activity. Methods. Complexes between CRP and the activated complement components C3d (C3d–CRP) and C4d (C4d–CRP), which reflect CRP-mediated complement activation, as well as the overall levels of activated C3 and C4 were measured in the plasma of 107 patients with active RA and 177 patients with inactive RA. Inactive RA was defined according to the American College of Rheumatology criteria for clinical remission. Disease activity was assessed by the modified Disease Activity Score (DAS28). Results. Plasma levels of C3d–CRP and C4d–CRP were increased in the majority of the patients, and were significantly higher in patients with active disease versus those with inactive RA (P < 0.001). In patients with active RA, the plasma concentrations of C3d–CRP and C4d–CRP correlated significantly with the DAS28 (Spearman’s rho 0.61 and 0.55, respectively; P < 0.001), whereas these correlations were less pronounced in patients with inactive RA (Spearman’s rho 0.28 [P < 0.001] and 0.25 [P ⴝ 0.001], respectively). Levels of activated C3 and C4 were also increased in the majority of the patients, particularly in patients with active RA. Conclusion. Part of the activation of complement in RA is mediated by CRP and is correlated with disease activity. We suggest that this activation is involved in the pathogenesis of RA. Rheumatoid arthritis (RA) is a chronic disease of unknown cause, characterized by inflammation of the joints. The pathogenesis of RA is incompletely understood, although there is compelling evidence that cytokines such as tumor necrosis factor ␣ and interleukin-1 are involved (1). Furthermore, there is substantial evidence that the complement system is also involved in the pathogenesis of RA (2–6). Increased levels of complement products and immune complexes have been found in the serum and synovial fluid of RA patients (4,5) and correlate with disease activity (6). Moreover, studies in animals have demonstrated that the complement system contributes to the inflammatory damage in arthritis; inhibition of the complement cascade ameliorates experimental arthritis (7,8). Complement is traditionally considered to be mainly activated by bacteria or immune complexes. Indeed, the latter have been implicated as the trigger for complement activation in RA (9). However, circulating immune complexes from patients with RA appear to have very little effect on activation of the complement system (10). Since there is no conclusive evidence that immune complexes are the main trigger for complement activation in RA, other potential triggers for complement activation in RA should be considered. One of these triggers may be C-reactive protein (CRP), since this acute-phase protein can activate complement both in vitro (11) and in vivo (12–14). 1 Esmeralda T. H. Molenaar, MD, Alexandre E. Voskuyl, MD, PhD: Vrije Universiteit Medical Center, Amsterdam, The Netherlands; 2Atoosa Familian, MD, Gerard J. van Mierlo: Central Laboratory of the Netherlands Red Cross Blood Transfusion Service, Amsterdam, The Netherlands; 3Ben A. C. Dijkmans, MD, PhD: Academic Hospital Vrije Universiteit and Jan van Breemen Instituut, Amsterdam, The Netherlands; 4C. Erik Hack, MD, PhD: Academic Hospital Vrije Universiteit and Central Laboratory of the Netherlands Red Cross Blood Transfusion Service, Amsterdam, The Netherlands. Address correspondence and reprint requests to Alexandre E. Voskuyl, MD, PhD, Department of Rheumatology, Vrije Universiteit Medical Center, P.O. Box 7057, 1007 MB Amsterdam, The Netherlands. Submitted for publication July 25, 2000; accepted in revised form February 6, 2001. 997 998 MOLENAAR ET AL CRP–complement complexes (12) serve as one parameter of CRP-mediated complement activation. These complexes have been detected in the circulation of renal allograft recipients (12) and in patients with sepsis (13). Notably, circulating levels of CRP are associated with the disease activity of RA (15). CRP has been found to be localized in inflamed joints in a rabbit model of arthritis (16), suggesting a possible role in local inflammatory reactions. Yet the association between CRP and the activity of RA is generally considered to be indirect in that the levels of CRP reflect the production of inflammatory cytokines, and the association has never been considered to result from a direct pathogenic effect of CRP. The present study was performed on the assumption that CRP is involved in the activation of complement in RA. Therefore, plasma levels of complexes between CRP and complement, as well as complement activation products (C3b/c [denotes C3b, C3bi, and/or C3c] and C4b/c) were determined in patients with active and inactive RA. In addition, we assessed the association of these parameters with disease activity. PATIENTS AND METHODS Patients. Clinical data and blood samples were collected from 284 RA patients who were recruited from an outpatient clinic. Of those patients, 177 were classified as having inactive RA and 107 were classified as having active RA. Inactive RA was defined by the American College of Rheumatology (ACR) criteria for clinical remission (17). Accordingly, clinical remission is present when 5 of the following 6 criteria are fulfilled: 1) duration of morning stiffness not exceeding 15 minutes; 2) no fatigue; 3) no joint pain; 4) no joint tenderness or pain on motion; 5) no soft tissue swelling in joints or tendon sheets; and 6) erythrocyte sedimentation rate (ESR) ⬍30 mm/hour for a female patient or ⬍20 mm/hour for a male patient. For this study, these criteria were modified by omitting the “no fatigue” criterion so that a patient was classified as having inactive RA when fulfilling 4 of the 5 remaining criteria. The criteria for joint pain and joint tenderness on motion were modified by allowing the consideration of mild arthralgia if local synovitis was absent and anatomic changes in the joint could be demonstrated radiologically, as previously described (18). Patients with active RA included 55 patients with a disease duration of ⬎1 year. In addition, 52 consecutive patients with early RA with a disease duration of ⬍1 year were also included. Patients were classified with active disease when not fulfilling the criteria for clinical remission (17). In order to assess disease activity, the modified Disease Activity Score (DAS28) was calculated. This composite index consists of the swollen and tender joint counts (each from a possible total of 28 joints), the ESR, and a visual analog scale for general health (19). All RA patients fulfilled the 1987 ACR (formerly, the American Rheumatism Association) criteria for RA (20). The protocol was approved by the local institutional ethics review committee. Collection of blood samples. Blood samples from patients were collected in vacutainer tubes containing EDTA. Plasma was obtained by centrifugation of blood and stored in aliquots at ⫺70°C until tested. Measurement of activated complement, CRP, and CRP–complement complexes. Activation of C3 and C4 was assessed with an enzyme-linked immunosorbent assay (ELISA), as described elsewhere in detail (21). In brief, monoclonal antibodies recognizing neoepitopes on C4b/c and C3b/c were used as catching antibodies. Biotinylated polyclonal rabbit anti-human C4 and C3c antibodies were used as detecting antibodies. Levels of C3b/c and C4b/c above the upper limits of the normal values in healthy controls, i.e., 57 nmoles/liter and 5 nmoles/liter, respectively, were considered to be increased. CRP was measured with a sandwich-type ELISA as described by Wolbink et al (12). Levels of CRP above the upper limit of normal (i.e., 5 mg/liter) were considered to be increased. Complexes between CRP and the degradation products of the activated complement components C3d (C3d– CRP) and C4d (C4d–CRP) were measured by ELISAs, as previously described (12). Levels of C3d–CRP and C4d–CRP above the detectable level in healthy controls (i.e., 4 pmoles/ liter) were considered to be increased. Statistical methods. Comparisons between patients with active RA and patients with inactive RA were made using the Mann-Whitney U test or the chi-square test. Correlations between the CRP–complement complexes and parameters of disease activity in active and inactive RA patients were analyzed using Spearman’s rank correlation coefficients. Twosided P values less than 0.05 were considered statistically significant. RESULTS Demographic and clinical characteristics. The characteristics of the 2 patient groups (active and inactive RA) are presented in Table 1. The disease duration and the presence of radiologic erosions were significantly lower in the patients with active RA when compared with those with inactive RA. Furthermore, parameters of disease activity and the frequency of treatment with disease-modifying antirheumatic drugs were, as expected, significantly higher in the patients with active RA when compared with those with inactive RA. Plasma levels of activated complement, CRP, and CRP–complement complexes. Increased C3b/c levels were found in 99% of the 107 active RA patients and in 98% of the 177 inactive RA patients. The median level of C3b/c in active RA patients was significantly higher compared with that in inactive RA patients (Table 2). Increased C4b/c levels were found in 98% of the active RA patients and in 98% of the inactive RA patients. The COMPLEMENT ACTIVATION BY CRP 999 Table 1. Demographic and clinical characteristics of patients with active and inactive rheumatoid arthritis (RA)* Age, years Female, no. (%) Disease duration, years RF positive, no. (%) Erosions on radiographs, no. (%) Currently taking DMARDs, no. (%) 28–swollen joint count 28–tender joint count ESR, mm/hour DAS28 CRP, mg/liter Active RA (n ⫽ 107) Inactive RA (n ⫽ 177) 59 (18–91) 83 (78) 1 (0–50) 70 (65) 61 (57) 59 (24–86) 114 (64) 7 (1–47) 121 (68) 135 (76) 0.98 0.02 ⬍0.001 0.50 0.001 96 (90) 124 (70) ⬍0.001 7 (0–25) 4 (0–28) 29 (1–113) 4.7 (1.0–8.1) 12 (1–112) 0 (0–9) 0 (0–6) 10 (1–40) 1.9 (0.1–3.5) 3 (0.07–47) ⬍0.001 ⬍0.001 ⬍0.001 ⬍0.001 ⬍0.001 P * Except where otherwise indicated, values are the median (range). RF ⫽ rheumatoid factor; DMARDs ⫽ disease-modifying antirheumatic drugs; ESR ⫽ erythrocyte sedimentation rate; DAS28 ⫽ modified Disease Activity Score (19); CRP ⫽ C-reactive protein. median level of C4b/c in active RA patients was not significantly different from that in the inactive RA patients (Table 2). The proportion of patients with an increased CRP level was significantly higher among those with active RA (72%) compared with those with inactive RA (33%). Also, the median level of CRP was significantly higher in patients with active RA when compared with that in patients with inactive RA (Table 1 and Figure 1A). The proportion of patients with an increased plasma level of C3d–CRP tended to be higher among active RA patients (91%) when compared with that among inactive RA patients (66%). Moreover, the median level of C3d–CRP was significantly elevated in patients with active RA when compared with that in patients with inactive RA (Table 2 and Figure 1B). Increased plasma levels of C4d–CRP were found in the same percentage of patients (93%) from both Table 2. Plasma levels of activated C3 and C4 and C3d–CRP and C4d–CRP complexes in patients with active and inactive RA* C3b/c, nmoles/liter C4b/c, nmoles/liter C3d–CRP, pmoles/liter C4d–CRP, pmoles/liter C3d–CRP:C3b/c C4d–CRP:C4b/c Active RA (n ⫽ 107) Inactive RA (n ⫽ 177) P 135 (46–374) 32 (5.7–212) 89 (9–1,214) 290 (1–3,000) 0.16 (0.03–3.12) 1.5 (0.04–22.1) 112 (23–279) 27 (6.1–300) 18 (7–384) 46 (1–1,502) 0.6 (0.04–11.4) 8.5 (0.01–150) 0.002 0.93 ⬍0.001 ⬍0.001 ⬍0.001 ⬍0.001 * Except where otherwise indicated, values are the median (range). See Table 1 for definitions. Figure 1. Plasma levels of C-reactive protein (CRP) (A), C3d–CRP (B), and C4d–CRP (C) in patients with inactive and active rheumatoid arthritis (RA). Bold lines indicate the median value. Dotted lines indicate the upper limit of normal. patient groups. The median level of C4d–CRP was significantly elevated in active RA patients when compared with that in inactive RA patients (Table 2 and Figure 1C). 1000 MOLENAAR ET AL Table 3. Correlation between activated C3 and C4, CRP, CRP– complement complexes, and parameters of disease activity in patients with active and inactive RA* Active RA DAS28 CRP C3b/c C4b/c Inactive RA DAS28 CRP C3b/c C4b/c CRP C3d–CRP C4d–CRP C3b/c C4b/c 0.68† – 0.13 0.12 0.62† 0.89† 0.18 0.18 0.56† 0.83† 0.26§ 0.26‡ 0.14 0.13 – 0.11 0.22‡ 0.12 0.11 – 0.22§ – 0.05 0.09 0.28† 0.92† 0.14 0.10 0.25§ 0.79† ⫺0.04 0.28§ 0.26§ 0.05 – 0.05 0.22§ 0.09 0.05 – * Values are the Spearman’s rank correlation coefficients. See Table 1 for definitions. † P ⬍ 0.001. ‡ P ⬍ 0.05. § P ⬍ 0.01. Because of the skewed distribution of activated complement components, we also assessed differences in the C3d–CRP and C4d–CRP levels in the total group of patients (n ⫽ 284). Patients were classified in subgroups based on whether the plasma concentration of C3b/c was below or above the median value in the total group of patients. Levels of C3d–CRP were significantly higher in the group of patients with a C3b/c concentration above the median when compared with the levels in patients with a C3b/c concentration below the median (P ⫽ 0.004). Conversely, levels of C4d–CRP were not significantly different between patients with C3b/c concentrations above or below the median. When patients were classified in subgroups based on the plasma concentration of C4b/c, the group of patients with a C4b/c concentration below the median value was found to have significantly lower levels of the C4d–CRP complex compared with the levels in patients with a C4b/c concentration above the median (P ⫽ 0.005). In contrast, levels of C3d–CRP were not significantly different between patients with a C4b/c concentration above or below the median. Correlations of activated complement and CRP– complement complexes with parameters of disease activity. In patients with active and inactive RA, significant correlations were found between the levels of CRP– complement complexes, levels of CRP, and the DAS28. The strength of these correlations was less pronounced in patients with inactive RA (Table 3). No significant correlations were found between the levels of activated complement components and the CRP levels. The levels of both C3b/c and C4b/c correlated significantly with the DAS28 (except in patients with active RA) and with the levels of C4d–CRP, but not with the levels of C3d–CRP (Table 3). Because of the skewed distribution of activated complement components, correlation coefficients were also calculated in all patients (n ⫽ 284). Patients were classified in 2 subgroups based on whether the plasma concentration of the activated complement components was above or below the median value. In the subgroup of patients with levels of C3b/c above the median, the C3b/c levels correlated significantly (P ⬍ 0.01) with the levels of C3d–CRP (r ⫽ 0.30), C4d–CRP (r ⫽ 0.26), and CRP (r ⫽ 0.28). In patients with levels of C3b/c below the median, no such correlations were found. In patients with levels of C4b/c above the median, a weak, but not significant, correlation between the C4b/c and C4d–CRP complex levels was found, whereas in patients with C4b/c levels below the median, no correlations were found. DISCUSSION The main conclusion from this study is that the plasma levels of activated complement and CRP– complement complexes are increased in the majority of patients with RA and that these levels are correlated with parameters of disease activity. The observation of increased levels of CRP–complement complexes in this study points to the involvement of CRP in complement activation and a possible role of CRP-mediated complement activation in the pathogenesis of RA. The presence of increased levels of activated complement components in RA patients has been reported before (6) and is confirmed by the results of the present study. In general, these levels are much higher in synovial fluid than in plasma (4), suggesting that spillover from the joints contributes to the increased plasma levels. Such a spillover would explain the higher levels of circulating C3b/c and C4b/c in the patients with active disease, since these patients may have more intense activation of complement in their joints. Complement is a potent inflammatory system, and therefore activation of this system is likely to contribute to local inflammatory reactions in the inflamed joints. Indeed, complement has been shown to enhance tissue damage in animal models of arthritis (7,8). Although circulating levels of activated complement components were higher in patients with active disease, the overall correlation between complement activation and disease activity was weak. Several explanations may account for this. First, circulating levels of activation products may not adequately reflect local activation in the joints. Second, the clearance rate of the fragments measured may be too high to allow a precise appreciation of the extent of complement activation in a chronic disease. Although there are no data regarding COMPLEMENT ACTIVATION BY CRP the clearance of activated C3 or C4 in vivo, we have observed that the half-life of clearance of these products is within 1 hour, and presumably in the range of 10–30 minutes (22). Finally, although we took care that the blood specimens were handled and stored appropriately, some in vitro activation of samples may have blurred the results to some extent. Complement activation has been previously demonstrated in patients with RA, as has been reported here. Circulating immune complexes have been held responsible for the complement activation in RA patients. However, there is little evidence that immune complexes from RA patients are indeed a main trigger for this complement activation (10). CRP–complement complexes are specific markers for CRP-mediated activation of the complement system, since these complexes are only generated during CRP-induced activation of complement (12). Thus, our data point to a contribution of CRP to the activation of complement. The weak correlations between the levels of C4b/c and C3b/c, which reflect overall activation independent of the nature of the activator, and the levels of the CRP– complement complexes suggest that this contribution may be limited and that other activators, such as immune complexes, may be involved as well. This has been shown previously by others and is based on observations from experimental and human studies, particularly on Felty’s syndrome and rheumatoid vasculitis (23,24). In addition to the role of CRP, it is clear that rheumatoid factor also plays an important role as a trigger for complement activation through the formation of immune complexes (25,26) It is now generally accepted that cytokines play a dominant role in the pathogenesis of RA. These cytokines induce their detrimental effects by stimulating various effector mechanisms, such as the release of metalloproteinases and the infiltration of inflammatory cells. Studies in patients with cancer receiving high doses of interleukin-2 have shown that cytokines may induce complement activation (27). Therefore, another effector mechanism of cytokines in inflammatory conditions may be activation of complement. We have found increasing levels of complement–CRP complexes in patients receiving interleukin-2 (Wolbink GJ, Hack CE: unpublished observations), thus pointing to CRP as the link between complement activation and cytokines. Indeed, the synthesis of CRP by the liver during inflammatory conditions is stimulated by cytokines such as interleukin-6. The results of the study reported here support the concept that, in RA, CRP-mediated complement activation can be one of the effector mechanisms triggered by cytokines. 1001 A model explaining the mechanism of CRPmediated complement activation has been described previously (28). In this model, secretory phospholipase A2 (sPLA2) hydrolyzes cell membrane phospholipids to yield lysophospholipids and free fatty acids. In normal cells, there is an asymmetric distribution of phospholipids in the 2 leaflets of the lipid bilayer of the cell membrane. During apoptosis of the cell, phospholipids of both the inner and outer leaflet exchange (flip-flop phenomenon). The sPLA2 cannot hydrolyze the phospholipids in the cell membranes of normal cells, but it does hydrolyze those of flip-flopped cells (28). The presence of lysophospholipids together with that of the negatively charged phosphatidylserine in the outer leaflet of the cell membrane causes some disruption of the tight package of the phospholipids, making phosphorylcholine groups accessible for interaction with CRP. Cell-bound CRP is, in turn, able to activate the complement system. This activation may enhance inflammation and contribute to tissue damage. Notably, levels of sPLA2 are elevated in plasma, and in particular in the synovial fluid of RA patients (29,30). Increased levels of sPLA2 were also found in our patients (31), which supports previous observations and is consistent with the hypothesis on the role of sPLA2 in CRP-mediated complement activation. Currently, we are investigating the validity of this concept by analyzing the binding of CRP in cells and phospholipid microparticles obtained from RA joints. Circulating CRP–complement complexes have been previously demonstrated in patients with infections of varying severity and were significantly higher in patients with shock and in patients with a fatal outcome (13). Furthermore, depositions of CRP together with C3 and C4 activation fragments have been found in tissue specimens from patients who died after a myocardial infarction. These CRP and complement depositions were localized only in infarcted tissue, but not in normalappearing areas of the myocardium (14), suggesting an association between CRP, complement activation, and tissue damage. Such an association was demonstrated by Griselli et al, who showed that injection of human CRP in rats enhanced infarct size by 40% after ligation of the coronary artery, the effect of which was dependent on complement (32). One could thus speculate that, in RA, CRP may have a similar detrimental effect. Whether this explains the relationship between CRP levels and progressive radiologic evidence of joint damage (15,33) remains to be established. In conclusion, the results of this study demonstrate that CRP can activate complement in RA. There- 1002 MOLENAAR ET AL fore, this acute-phase protein should be considered an inflammatory mediator in this disease. REFERENCES 1. Fox DA. Cytokine blockade as a new strategy to treat rheumatoid arthritis: inhibition of tumor necrosis factor. Arch Intern Med 2000;160:437–44. 2. Brodeur JP, Ruddy S, Schwartz LB, Moxley G. Synovial fluid levels of complement SC5b–9 and fragment Bb are elevated in patients with rheumatoid arthritis. Arthritis Rheum 1991;34: 1531–7. 3. Abbink JJ, Kamp AM, Nuijens JH, Eerenberg AJM, Swaak AJG, Hack CE. Relative contribution of contact and complement activation to inflammatory reactions in arthritic joints. Ann Rheum Dis 1992;51:1122–8. 4. Swaak AJG, van Rooijen A, Planten O, Han H, Hattink O, Hack E. An analysis of the levels of complement components in the synovial fluid in rheumatic diseases. Clin Rheumatol 1987;22:350–7. 5. Shingu M, Watanabe Y, Tomooka K, Yoshioka K, Ohtsuka E, Nobunaga M. Complement degradation products in rheumatoid arthritis. Br J Rheumatol 1994;33:299–300. 6. Makinde VA, Senaldi G, Jaward AS, Berry H, Vergani D. Reflection of disease activity in rheumatoid arthritis by indices of activation of the classical complement pathway. Ann Rheum Dis 1989;48:302–6. 7. Goodfellow RM, Williams AS, Levin JL, Williams BD, Morgan BP. Local therapy with soluble complement receptor 1 (sCR1) suppresses inflammation in mono-articular arthritis. Clin Exp Immunol 1997;110:45–52. 8. Wang Y, Rollins SA, Madri JA, Matis LA. Anti-C5 monoclonal antibody therapy prevents collagen-induced arthritis and ameliorates established disease. Proc Natl Acad Sci U S A 1995;92: 8955–9. 9. Sato Y, Sato R, Watanabe H, Kogure A, Watanabe K, Nishimaki T, et al. Complement activating properties of monoreactive and polyreactive IgM rheumatoid factors. Ann Rheum Dis 1993;52: 795–800. 10. Hack CE, Eerenberg-Belmer AJM, Lim UG, Haverman J, Aalberse RC. Lack of activation of C1, despite circulating immune complexes detected by two C1q methods, in patients with rheumatoid arthritis. Arthritis Rheum 1984;27:40–8. 11. Volonakis JE. Complement activation by C-reactive protein complexes. Ann N Y Acad Sci 1982;389:235–49. 12. Wolbink GJ, Brouwer MC, Buysman S, ten Berge IJM, Hack CE. CRP-mediated activation of complement in vivo: assessment by measuring circulating complement-C-reactive protein complexes. J Immunol 1996;157:473–9. 13. Wolbink GJ, Bossink AWJ, Groeneveld ABJ, de Groot MCM, Thijs LG, Hack CE. Complement activation in patients with sepsis is in part mediated by C-reactive protein. J Infect Dis 1998;177: 81–7. 14. Lagrand WK, Niessen HWM, Wolbink GJ, Jaspers LH, Visser CA, Verheugt FWA, et al. C-reactive protein co-localizes with complement in human hearts during acute myocardial infarction. Circulation 1997;95:97–103. 15. Van Leeuwen MA, van Rijswijk MH, van der Heijde DMFM, te Meerman GT, van Riel PLCM, Houtman PM, et al. The acute phase response in relation to radiographic progression in early rheumatoid arthritis: a prospective study during the first three years of the disease. Br J Rheumatol 1993;23:9–13. 16. Kushner I, Kaplan MH. Studies of acute phase protein. I. An immunohistochemical method for the localization of C-reactive protein in rabbits: association with necrosis in local inflammatory lesions. J Exp Med 1961;114:961–74. 17. Pinals RS, Masi AT, Larsen RA, and The Subcommittee for 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. Criteria of Remission in Rheumatoid Arthritis of the American Rheumatism Association Diagnostic and Therapeutic Criteria Committee. Preliminary criteria for clinical remission in rheumatoid arthritis. Arthritis Rheum 1981;24:1308–15. Ten Wolde S, Breedveld FC, Hermans J, Vandenbroucke JP, van der Laar MAFJ, Markusse HM, et al. Randomised placebo controlled study of stopping secondline drugs in rheumatoid arthritis. Lancet 1996;347:347–52. Prevoo MLL, van ’t Hof MA, Kuper HH, van Leeuwen MA, van de Putte LBA, van Riel PLCM. Modified disease activity scores that include twenty-eight–joint counts: development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum 1995;38:44–8. Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 1988;31:315–24. Wolbink GJ, Bollen J, Baars JW, ten Berge RJM, Swaak AJG, Paardekooper J, et al. Application of a monoclonal antibody against a neoepitope on activated C4 in an ELISA for the quantification of complement activation via the classical pathway. J Immunol Methods 1993;163:67–76. Buysmann S, Hack CE, van Diepen FN, Surachno J, ten Berge IJM. Administration of OKT3 as a two-hour infusion attenuates for dose side effects. Transplantation 1997;64:1620–3. Breedveld FC, Lafeber GJ, de Vries E, van Krieken JH, Cats A. Immune complexes and the pathogenesis of neutropenia in Felty’s syndrome. Ann Rheum Dis 1986;45:696–702. Westedt ML, Daha MR, de Vries E, Valentijn RM, Cats A. IgA containing immune complexes in rheumatoid arthritis and in active rheumatoid disease. J Rheumatol 1985;12:449–55. Pope RM, Yoshinoya S, McDuffy S. Detection of immune complexes and their relationship to rheumatoid factor in a variety of autoimmune disorders. Clin Exp Immunol 1981;46:256–67. Elson CJ, Scott DGI, Blake DR, Bacon PA, Holt PDJ. Complement-activating rheumatoid factor containing complexes in patients with rheumatoid vasculitis. Ann Rheum Dis 1983;42:147–50. Thijs LG, Hack CE, Strack van Schijndel RJM, Nuijens JH, Wolbink GJ, Eerenberg-Belmer AJM, et al. Complement activation and high dose of interleukin-2 [letter]. Lancet 1989;2:395. Hack CE, Wolbink GJ, Schalkwijk C, Seijer H, Hermens WT, van de Bosch H. A role for secretory phospholipase A2 and C-reactive protein in the removal of injured cells. Immunol Today 1997;187: 111–5. Koo Sin Lin M, Farewell V, Vadas P, Bookman AAM, Keystone EC, Pruzanski W. Secretory phospholipase A2 as an index of disease activity in rheumatoid arthritis: prospective double blind study of 212 patients. J Rheumatol 1996;23:1162–6. Loeser RF, Smith DM, Turner RA. Phospholipase activity in synovial fluid from patients with rheumatoid arthritis, osteoarthritis and crystal-associated arthritis. Clin Exp Rheumatol 1990;8: 379–86. Molenaar ETH, Voskuyl AE, Hack CE, Dijkmans BAC. Levels of secretory phospholipase A2 are elevated in patients with active rheumatoid arthritis when compared to patients with inactive rheumatoid arthritis [abstract]. Ann Rheum Dis 2000;59 Suppl 1:105. Griselli M, Herbert J, Hutchinson WL, Taylor KM, Sohail M, Krausz T, et al. C-reactive protein and complement are important mediators of tissue damage in acute myocardial infarction. J Exp Med 1999;190:1733–9. Van Leeuwen MA, van Rijswijk MH, Sluiter WJ, van Riel PLCM, Kuper IH, van de Putte LBA, et al. Individual relationship between progression of radiological damage and the acute phase response in early rheumatoid arthritis: towards development of a decision support system. J Rheumatol 1997;24:20–7.