* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download VF / Pulseless VT
Cardiac contractility modulation wikipedia , lookup
Coronary artery disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Myocardial infarction wikipedia , lookup
Electrocardiography wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
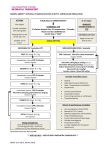
A. Jafari . MD Assistant Professor of emergency medicine Zanjan University of medical science • Four rhythms produce pulseless cardiac arrest: • Ventricular fibrillation (VF). • rapid ventricular tachycardia (VT). • Pulseless electrical activity (PEA). • Asystole. VF V.tach PEA Asystole Do not Forget ABCD • A: Insert an advanced airway. • B: PPV, Pulseoximetry. • C: Continuing chest compression, Obtaining certain IV root, Fluid & drug administration. • D: Differential diagnosis. • Endotracheal route: • What drugs? Lidocaine, Epinephrine, Atropine, Naloxone, and Vasopressin. • Results in lower blood concentrations than the same dose given intravascularly. • The optimal endotracheal dose of most drugs is unknown, but typically 2 to 2.5 times recommended IV dose. • should dilute recommended dose in 5 to 10 mL of water or normal saline. • VF / Pulseless VT: • immediate bystander CPR with minimal interruption in chest compressions and defibrillation as soon as possible. • witnessed arrest + defibrillator on-site: Deliver 2 rescue breath. Check pulse. If no pulse; Turn on the defibrillator, place paddles, and check the rhythm. If VF/pulseless VT is present ,deliver 1 shock & immediately resume CPR. • Unwitness arrest in out-of-hospital setting: • Give 5 cycles of CPR before attempting defibrillation.(??) Management of VF / pulseless VT: • Deliver 1 shock. biphasic: 120-200 j Monophasic: 360 j • Then resume CPR immediately and continue for 2 min then check rhythm. • When a rhythm check reveals VF/VT, rescuers should provide CPR while the defibrillator charges. • Recall H’s & T’s. • Hypovolemia. • Toxin. • Hypoxia. • Tamponade. • Hydrogen ion. • T.P • Hypo/Hyperkalemia. • Thrombosis (coronary or pulmonary). • Hypothermia. • If VF/VT persists after 1 or 2 shocks plus CPR, give Epinephrine 1mg q3-5 min. • When VF/pulseless VT persists after 2-3 shocks plus CPR and vasopressor, consider antiarrhythmic. • Rhythm checks should be brief, and pulse checks should generally be performed only if an organized rhythm is observed. • Continue shock-CPR(2 min) sequence + antiarrhythmic. • Amiodarone 300 mg IV/IO bolus. 150 mg after 10-15 min. Repeat amiodarone • Lidocaine 1-1.5 mg/kg first dose then 0.5- 0.75 mg/kg. maximum 3 doses or 3 mg/kg with 5-10 min interval. • Consider MgSO4 for torsades de pointes. Loading dose 1-2 gr in 10cc DW5% IV/IO. Fibrinolysis • Ongoing CPR is not an absolute contraindication to fibrinolysis. • Fibrinolytic therapy should not be routinely used in cardiac arrest. • It may be considered on a case-by-case basis when PTE (MI) is suspected. Pacing in Arrest • Several randomized controlled trials failed to show benefit from attempted pacing for asystole. • At this time use of pacing for Pts with asystolic cardiac arrest is not recommended. Precordial Thump • It can deteriorate in cardiac rhythm • It may be considered for • termination of – Witnessed – monitored – unstable ventricular tachyarrhythmias – when a defibrillator is not immediately ready for use. Sodium Bicarbonate • It’s routine use is not recommended • Can be beneficial: – Preexisting metabolic acidosis – Hyperkalemia – TCA overdose