* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download ANTI-ANXIETY DRUGS
Drug interaction wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Serotonin syndrome wikipedia , lookup
Theralizumab wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Dextropropoxyphene wikipedia , lookup
Neuropharmacology wikipedia , lookup
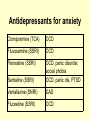
Anxiolytics & Hypnotics by Sue Henderson Therapeutic actions 1. 2. 3. 4. 5. Hypnotic Anxiolytic Anticonvulsant Amnestic Myorelaxant • In what medical circumstances might the amnestic properties of benzodiazepines be useful? Indications • Why are benzodiazepines useful in the treatment of alcohol detoxification? • Can they be used in the long term to prevent further alcohol abuse? Anti-Anxiety & Hypnotics Anti-Anxiety Hypnotics: Sedatives • Benzodiazepine e.g. Diazepam • Benzodiazepine e.g. Temazepam • Non Benzodiazepine e.g. Buspirone • Non Benzodiazepine e.g. Zopiclone Differentiate • What is the difference between an anti-anxiety medication and a hypnotic? Antidepressants for anxiety Clomipramine (TCA) OCD Fluvoxamine (SSRI) OCD Paroxetine (SSRI) Sertraline (SSRI) OCD, panic disorder, social phobia OCD, panic dis, PTSD Venlafaxine (SNRI) GAD Fluoxetine (SSRI) OCD Benzodiazepines • Used mostly in primary care rather than psychiatry. • Often prescribed for problems that are more effectively managed with non-drug therapies. • Temazepam in 10 most frequently prescribed up until 2001. Benzodiazepines • Should not be 1st line therapy in mental health & sleep management. • Limit use to less than 2 weeks. • Only benefit of continued use is avoiding withdrawal effects (NPS, 1999). • All equally effective but differ in metabolism, speed of onset & half life 2004-05 National Health Survey • 5% of Australians had used a benzodiazepine for anxiety management in the 2 weeks prior to the survey. • Benzodiazepine use was higher in women and in older age groups (mostly due to sleeping tablets). • Overall use has fallen since 80’s but total use remains high (ABS, 2006). Anxiolytic/hypnotic (% of pop all age groups) 12 10 8 6 4 2 0 Temazepam Diazepam Other benzodiazepines Oxazepam MCQ Benzodiazepines can safely be prescribed during pregnancy. • A. True • B. False Indications Anxiolytic Drug Diazepam, Alprazolam, Bromazepam, Lorazepam, Oxazepam, Buspirone* Muscle relaxant Diazepam Pre-med Diazepam, Lorazepam Alcohol withdrawal Diazepam, Oxazepam, Panic disorder Alprazolam, Clonazepam. Anti-convulsant Clobazam, Clonazepam, Diazepam, Lorazepam Hypnotic Flunitrazepam, Nitrazepam Temazepam, Zolpidem, Zopiclone* Dose Equivalents Drug Daily range mg Equiv 5mg diazepam. Duration (½ life) alprazolam 1–4 0.5 - 1 Short/Intermediate bromazepam 6–9 3–6 Short/Intermediate clobazam 30 – 80 10 Intermediate clonazepam 4–8 0.5 Intermediate diazepam 5 – 20 5 Long flunitrazepam 0.5 – 2 1–2 Intermediate lorazepam 2–4 1 Short/Intermediate nitrazepam 5 – 20 5 – 10 Intermediate oxazepam 45 – 90 15 – 30 Short temazepam 10 – 30 10 - 20 Short triazolam 0.125 - 0.25 0.25 Short buspirone* 15 – 30 - Short zopiclone* 3.75 - 7.5 - Short Short Acting: 3 - 8 hrs • Oxazepam • Temazepam • Triazolam • Buspirone* • Zopiclone* Intermediate Acting: 10 - 20 hours • • • • • • • Alprazolam Bromazepam Clobazam Clonazepam Flunitrazepam Lorazepam Nitrazepam Hypnotics • Explain the benefit of using Temazepam over Nitrazepam for assisting with sleep. • Why should hypnotics be used for a limited time to assist with sleep? Long Acting 1- 3 days: Diazepam X X X Addiction • Why are short acting benzodiazepines more of a problem with addiction than the long acting ones? Dependency cycle of benzodiazepines Use of benzodiazepine Even more anxious Reduced anxiety Effect wears off Green, 1996, p. 88 Benzodiazepines: Action • CNS depressant • Enhance the effect of GABA. • GABA is a neurotransmitter that inhibits neuronal activity i.e. reduces the firing rate of neurones. Agonist = Facilitate • Benzodiazepines bind to a site near the GABA binding site thus facilitating the action of GABA Death Coma General Anaesthesia Sleep Sedation Disinhibition Relief from anxiety No effect Increasing dose of drug •(Julien, 2001) Combination CNS depressants Contra-indications • Myasthenia gravis. • Severe respiratory impairment e.g sleep apnoea, COAD. Avoid (if possible) • Pregnancy • Lactation Adverse Effects • Physical dependence occurs in about 1 in 3 patients. • History substance abuse > risk dependence • Increased accident risk. • Tolerance & rebound insomnia. • Alcohol & CNS depressants potentiate adverse effects. Adverse effects • 60y+ > vulnerability to confusion, memory impairment, over sedation (most common S/E) & falls. • Adverse mood effects: depression, emotional anaesthesia, aggression, increased suicide risk in elderly. Withdrawal from Benzodiazepines • Abrupt cessation: > seizures • Withdrawal symptoms may occur between doses during continuous use (inter-dose withdrawal). Patients may think these symptoms are due to the original problem. • Withdrawal symptoms: increased anxiety, sleep disorder, aching limbs, nervousness & nausea. Withdrawal from Benzodiazepines • Withdrawal experienced by 45% of patients discontinuing low dose benzodiazepines & 100% patients on high doses. • Short half life benzodiazepines are associated with more acute & intense withdrawal symptoms. • Long half life benzodiazepines - milder, more delayed withdrawal (NPS, 1999). Withdrawal from benzodiazepines • Benzodiazepines should not be ceased abruptly. • Dose reduced by 10-20% per week. • Patient allowed to stabilise between each reduction. • Admission for high dose users, history of seizures or psychosis, or for more rapid withdrawal. Withdrawal from benzodiazepines • Implement relaxation/cognitive techniques. • If necessary referral: • Drug & Alcohol Services • Self Help group TRANX www.tranx.org.au • Psychologist (for CBT) Overdose Benzodiazepines • Generally safe in overdose unless mixed with alcohol/CNS depressants. • Symptoms overdose: hypotension, respiratory depression & coma. • Treatment: Supportive • Flumazenil rarely indicated IV Flumazenil • Dangerous to use if mixed overdose (e.g benzodiazepine + tricyclics, amphetamines, other pro-convulsants) - Result in uncontrolled seizure • In dependent individuals severe withdrawal • Flumazenil has a shorter half life ( one hour) than all benzodiazepines Therefore, repeat doses of flumazenil may be required to prevent recurrent symptoms of overdosage once the initial dose of flumazenil wears off. Flumazenil is a benzodiazepine Antagonist = Blocker Flumazenil binds to GABA receptor displacing benzodizepine Non benzodiazepines Anxiolytic: Buspirone (Buspar) • Different action to bzd. • Not a CNS depressant. • Partial agonist (stimulant) of dopaminergic & serotoninergic receptors. • No sedation, anti-convulsant or muscle relaxant properties - just anxiolytic. • Delayed action (1-2 weeks) • Effect reduced if benzodiazepine used in last 3/12 Comparison of benzodiazepine & buspirone Benzodiazepine Rapid onset Can cause sedation May impair performance Additive effects with alcohol May cause dependence & withdrawal Pharmacokinetic change with age Associated with falls in elderly (Keltner & Folks, 2001) Buspirone Delayed onset (cannot be used PRN) Does not cause sedation Does not impair performance No additive effect with alcohol Non addictive No pharmacokinetic change with age Does not cause falls in elderly Expensive (Not on PBS) Presentation: Buspar • White scored • 5 mg & 10 mg tabs Buspirone: Agonist = Mimic • Buspirone attaches to serotonin receptor mimicking serotonin. Non benzo Hypnotic: Zopiclone (Imovane) • Similar action, side effects & contraindications to benzo’s. Benzodiazepines key points • Should not be used in patients with liver disease, history of substance abuse, severe respiratory distress, performing hazardous tasks • Avoid during pregnancy/lactation if possible • Assess for over sedation • Cease slowly • Monitor elderly (cognition, falls) • Be aware they raise seizure threshold, and • Potentiate CNS depressants (alcohol) Hypnotic key points • Advise re rebound insomnia when medications ceased • Should not be used in sleep apnoea • Avoid alcohol • Hangover effect (impairing performance) • Monitor in elderly (falls, double dosing) References • Australian Bureau of Statistics. (2006). National health survey 2004-05: Summary of results. Canberra: Australian Bureau of Statistics. • Fortinash, K. M., & Holoday-Worret, P. A. (2000). Psychiatric mental health nursing ( 2nd ed.). St. Louis: Mosby. • Galbraith, A., Bullock, S. & Manias, E. (2001). Fundamentals of pharmacology (3rd ed.). Melbourne: Prentice Hall. References • Julien, R. M. (2001). A primer of drug action: A concise, nontechnical guide to the actions, uses, and side effects of psychoactive drugs. New York: W. H. Freeman and Co. • Keltner, N. L., & Folks, D. G. (2001). Psychotropic drugs (3rd ed.). St. Louis: Mosby. • National Prescribing Service. (1999). Helping patients withdraw. National Prescribing Service Newsletter, No. 4 June. • National Prescribing Service. (1999). Benzodiazepines reviewing long term use: A suggested approach. Prescribing Practice Review, No. 4 July.