* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download International Standards for Tuberculosis Care, 2009
Dirofilaria immitis wikipedia , lookup
Trichinosis wikipedia , lookup
Sarcocystis wikipedia , lookup
Marburg virus disease wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Microbicides for sexually transmitted diseases wikipedia , lookup
Diagnosis of HIV/AIDS wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Schistosomiasis wikipedia , lookup
Leptospirosis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Mycobacterium tuberculosis wikipedia , lookup
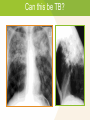
Module 5 – March 2010 Case Finding and Diagnosis Project Partners Funded by the Health Resources and Services Administration (HRSA) Module Overview Case Finding Steps in Diagnosing TB • Medical History • Bacteriologic Examination • Drug Susceptibility Testing • Radiographic Exam • Sputum smear-negative patient International Standards 1, 2, 3, 4, 5, and 18 Learning Objectives At the end of this presentation, participants will be able to: List the steps involved in diagnosing tuberculosis Describe the role of sputum smear microscopy in the diagnosis of tuberculosis Recognize the role of culture and drug sensitivity testing in the diagnosis and management of tuberculosis Case Finding Rapid, accurate diagnosis is essential for individual and public health Despite technical advances, clinical acumen with a high index of suspicion remains vital to the diagnosis of tuberculosis THINK TB Where can you conduct case finding activities? Opportunities for Case Finding TB Chest Clinics Drug Rehab Centres Hospitals (Public) HIV Care facilities Public Health Clinics Private medical clinics Voluntary Counselling Occupational Health and Testing (VCT) facilities clinics Long term care Prevention of Mother facilities and shelters to Child Transmission (PMTCT) clinics Correctional facilities (prisons, jails) Steps in Diagnosing TB Medical History Bacteriologic examination TB Culture and Drug Susceptibility Testing Radiographic exam Other examinations based on site(s)/location(s) involved Medical History Known exposure to a person with infectious pulmonary TB Symptoms of TB disease and onset Previous treatment for latent TB infection or active TB disease Risk factors for developing TB disease Other medical conditions that might affect treatment approach What are the signs and symptoms of tuberculosis? Standard 1: Prolonged Cough All persons with otherwise unexplained productive cough lasting two-three weeks or more should be evaluated for tuberculosis International Standards for Tuberculosis Care, 2009 Prolonged Cough Think TB: Prolonged Cough (2 - 3 weeks) Cough may not be specific for TB, however, long duration raises the likelihood of TB diagnosis This is common criterion for suspecting TB in most national and international guidelines The likelihood of AFB smear-positive sputum increases with increasing duration of cough Will not catch all TB cases; use best clinical judgment “Classic” TB Clinical Presentation Subtle onset and chronic course Chest symptoms • Cough (usually productive) • Hemoptysis • Chest pain (usually pleuritic) Nonspecific constitutional symptoms Extrapulmonary symptoms (if involved) Typical Systemic Symptoms Fever in 65-80% of cases Night sweats Fatigue/malaise Anorexia/weight loss 10-20% of TB cases have no symptoms at the time of diagnosis Clinical Presentation Physical Examination (PE): May be normal in mild–moderate disease Lungs: rales, rhonchi; absent breath sounds and dullness to percussion if pleural fluid is present Extrapulmonary (site specific): adenopathy, skin lesions, bone tenderness, neck stiffness, etc. The PE is most useful when assessing for non-pulmonary sites of TB Bacteriologic Examination Standard 2: Sputum Microscopy All patients suspected of having pulmonary TB who can produce sputum should have at least two sputum specimens obtained for microscopic examination in a quality-assured laboratory. When possible, at least one early morning specimen should be obtained. International Standards for Tuberculosis Care, 2009 Sputum Microscopy To confirm a diagnosis of TB, every effort must be made to identify the causative agent The AFB smear in high-prevalence areas is: • Highly specific for TB • Most rapid method for determining TB diagnosis • Identifies those at greatest risk of dying from TB • Identifies those most likely to transmit disease Performance of Sputum Microscopy Specimen Number Incremental Yield (of all smear positive) Incremental Sensitivity (of all culture positive) 1 85.8% 53.8% 2 11.9% 11.1% 3 2.4% 3.1% Total 100% 68.0% Average yield of single early morning specimen: 86.4% Average yield of single spot specimen: 73.9% Mase SR, Int J tuberc Lung Dis 2007;11(5): 485-95 Culture & Drug Susceptibility Testing Obtaining culture and drug susceptibility testing (DST) offers significant advantages in the diagnosis and management of TB: Increases case detection Earlier diagnosis Identification of drug resistance Culture: Advantages Higher sensitivity than smear microscopy (culture can make diagnosis despite fewer bacilli in specimen) If TB disease is suspected and sputum smears are negative, culture may provide diagnosis Allows for identification of mycobacterial species Allows for drug susceptibility testing Culture: Disadvantages Cost Technical complexity May take weeks to get results Requires ongoing quality assurance Therefore, culture testing is more likely to be found in major referral centers. Avoid delaying appropriate TB treatment in suspicious cases while awaiting results. Case 1 A 32 year old man presents to the clinic with complaint of cough x 1 month. He is not severely ill and can be evaluated in an ambulatory setting. Questions: What other history do you ask him about? What other signs will you look for during your examination to aide in diagnosis? Case 1 (2) Patient gives further history of feeling poorly for several months now; reports weight loss (about 3-4kg) and cough has gotten progressively worse. Patient denies smoking. His brother was treated for tuberculosis last year. Patient was not evaluated for TB at that time. Question: What laboratory tests would do you order? Case 1 (3) Among the results you receive, one of two sputum smears is positive for acid fast bacilli (AFB) on direct microscopy. Question: What would you do next? Case 1 Summary If smear result is from a Lab with EQA: Obtain chest X-ray, order TB culture and initiate TB treatment Standard 3: Extrapulmonary Specimens For all patients suspected of having extrapulmonary TB, appropriate specimens from the suspected sites of involvement should be obtained for microscopy, culture, and histopathological examination. International Standards for Tuberculosis Care, 2009 Clinical Presentation: Extrapulmonary Incidence/site may vary TB can involve any organ More common in HIV/TB (co-infection) Both, 9% Lymphatic, 42% Pleural, 18% Extrapulmonary, 21% Other, 12% Pulmonary, 70% Bone/joint, 11% TB Cases by Form of Disease, United States, CDC, 2005 Peritoneal, 6% Genitourinary, 5% Meningeal, 6% Extrapulmonary Tuberculosis Radiographic Examination Standard 4: Evaluation of Abnormal CXR All persons with chest radiographic findings suggestive of tuberculosis should have sputum specimens submitted for microbiological examination. International Standards for Tuberculosis Care, 2009 Evaluation of Abnormal CXR Study from India: 2229 outpatients evaluated by CXR/culture Of 227 cases deemed TB by CXR alone • 36% had negative sputum cultures for TB Of 162 culture-positive cases of TB • 20% would have been missed based on CXR alone CXR alone is not enough! Nagpaul DR, Proceedings of the 9th Eastern Region Tuberculosis Conference and 29th National Conference on Tuberculosis and Chest Diseases. 1974 Delhi, as cited in Toman’s tuberculosis. Case detection, treatment and monitoring, 2nd Edition: World Health Organization, 2004 Chest Radiography Purpose: Provides additional evidence to aid in diagnosis of TB disease when only 1 sputum smear is positive in settings without an EQC laboratory Check for lung abnormalities in people who have symptoms of TB; especially in those with HIV co-infection Evaluate and rule out TB disease in persons with a newly positive tuberculin skin test (Mantoux) Chest X-ray alone cannot confirm TB disease Chest Radiography (2) Chest X-ray findings suggestive of active PTB disease include: Acute upper lobe pneumonia Unresolving pneumonia Cavitation, cavitary lesion Pleurisy, pleural effusion Lung infiltrate, especially in upper lung zones Intrathoracic adenopathy International Standards for Tuberculosis Care, 2009 Chest Radiography (3) Chest X-ray findings suggestive of previous or presumed inactive PTB include: Apical fibrosis Upper lobe fibronodular abnormality Pleural (fibro) calcification Upper lung zone bronchiectasis Thoracoplasty or partial pneumonectomy Healed primary lesion (Ghon focus/complex) Can this be TB? Can this be TB? Miliary TB Can this be TB? 54-year-old man with three months of focal low-back pain Can this be TB? Extrapulmonary 54-year-old man with three months of focal low-back pain “Pott’s disease” Signs and symptoms of extrapulmonary TB are site specific Sampling of extrapulmonary sites for smear, culture, and histopathology may confirm diagnosis Sputum Smear-Negative Patient Criteria for diagnosis: Have sputum that is smear-negative but culturepositive for M. tuberculosis OR Decision by a clinician to treat with a full course of anti-TB therapy; AND Chest X-ray consistent with TB; AND either: • Laboratory or strong clinical suspicion of HIV infection • Lack of response to broad-spectrum (nonfluoroquinolone) antibiotic (if HIV-negative or unknown) Standard 5: Smear-negative Diagnosis The diagnosis of sputum smear-negative PTB should be based on the following criteria: At least two negative sputum smears (including at least one early morning specimen) Chest radiographic findings consistent with TB Lack of response to a trial of broad-spectrum anti-microbial agents (avoid use of fluoroquinolones) For such patients sputum cultures should be obtained. International Standards for Tuberculosis Care, 2009 Standard 5: Smear-negative Diagnosis (2) In persons who are seriously ill or have known or suspected HIV infection, the diagnostic evaluation should be expedited and if clinical evidence strongly suggests TB, a course of antituberculosis treatment should be initiated International Standards for Tuberculosis Care, 2009 TB Diagnostic Algorithm: HIV-Negative or Low Prevalence Area All Pulmonary TB Suspects Sputum AFB Microscopy Assess for HIV Any smear + Rx: Non-anti TB antibiotics Improvement? > 2 smears - No Yes Repeat AFB smear Order TB culture > 1 smear +or TB culture + Yes TB* Yes TB* All smears CXR & medical officer’s judgment No TB TB Diagnostic Algorithm: HIV-Positive and High Prevalence Ambulatory HIV+ TB Suspect AFB smears/culture; DST AFB Positive* Treat for TB; CPT; HIV care if positive AFB Negative * TB likely Clinical evaluation; CXR; TST; may repeat AFB smears/culture TB not likely Reassess for TB No or poor response Treat for bacterial infection and/or PCP; HIV care if positive; CPT Reassess if symptoms recur CPT = cotrimoxazole prophylaxis Response Clinical Presentation and Diagnosis of TB Remember: Symptoms/severity can range from none to overwhelming Tempo of illness: ranges from indolent to fast TB can involve any organ or tissue Signs/symptoms may be both local and systemic Consider HIV testing in the diagnostic evaluation TB is capable of presenting in many ways Can this be TB? Can this be TB? Atypical pattern: Primary TB Distribution: Any lobe involved (slight lower lobe predominance) Air-space consolidation Cavitation is uncommon (< 10%) Adenopathy is common (especially in children and HIV) Miliary pattern ISTC Standard 18 All providers of care for patients with TB should ensure that persons who are in close contact with patients who have infectious TB are evaluated and managed in line with international recommendations. The determination of priorities for contact investigation is based on the likelihood that a contact: 1. Has undiagnosed TB 2. Is at high risk of developing TB if infected 3. Is at risk of having severe TB if the disease develops 4. Is at high risk of having been infected by the index case ISTC Standard 18 (2) The highest priority contacts for evaluation are: Persons with symptoms suggestive of tuberculosis Children aged <5 years Contacts with known or suspected immunocompromise, particularly HIV infection Contacts of patients with MDR/XDR tuberculosis Other close contacts are a lower priority group Contact Investigation There is a high likelihood that a person with smear-positive PTB will transmit tuberculosis. Therefore, prompt and thorough contact investigation is essential for the control of TB Contact investigations should start with the persons most likely to be infected (those who most frequently come in contact with the person who has infectious TB) Contact Investigation (2) Actively seeking out and evaluating contacts to persons with smearpositive PTB is an important TB control strategy for two reasons: • It identifies persons with previously undetected tuberculosis, allowing initiation of treatment and halting further transmission • It identifies persons with TB infection who would benefit from isoniazid preventive therapy (IPT) to prevent future TB reactivation Case Finding and Diagnosis of TB Summary: A prolonged duration of cough should raise TB suspicion and trigger a diagnostic evaluation TB risk factors and exposure increase level of suspicion AFB smear in high-prevalence areas is highly specific and most rapid tool for diagnosing TB Radiographic patterns may help in TB diagnosis if suspicion high and AFB smear is negative, but a radiograph alone is not enough to make diagnosis Summary: ISTC Standards Covered* Standard 1: Unexplained productive cough lasting 2-3 weeks or more should be evaluated for tuberculosis. Standard 2: All TB suspects should have at least 2 sputum specimens obtained for microscopic examination (at least one early morning specimen if possible). Standard 3: Specimens from suspected extrapulmonary TB sites should be obtained for microscopy, culture, and histopathological exam. * Abbreviated versions Summary: ISTC Standards Covered* (2) Standard 4: All persons with chest radiographic findings suggestive of TB should have sputum specimens submitted for microbiological examination. Standard 5: The diagnosis of smear-negative PTB should be based on the following: at least two negative sputum smears (including at least one early morning specimen); CXR finding consistent with TB; and lack of response to broad-spectrum antibiotics (avoid fluoroquinolones). Obtain cultures. Seriously ill or HIV + patients should have an expedited diagnostic evaluation and if there is strong clinical evidence, treatment should be initiated. * Abbreviated versions Summary: ISTC Standards Covered* (3) Standard 18: All providers of care for patients with TB should ensure that persons who are in close contact with patients who have infectious TB are evaluated and managed in line with international recommendations. The highest priority contacts for evaluation are: Persons with symptoms suggestive of tuberculosis Children aged <5 years Contacts with known or suspected immunocompromise, particularly HIV infection Contacts of patients with MDR/XDR tuberculosis Other close contacts are a lower priority group * Abbreviated versions Think TB Additional Cases Can this be TB? Can this be TB? Typical Pattern: Reactivation, Post-primary TB Distribution Apical / posterior segments of upper lobes Superior segments of lower lobes Isolated anterior segment involvement is unusual (think M. avium complex or other disease) Reactivation/Post-primary TB Patterns of disease Air-space consolidation Cavitation, cavitary nodule Endobronchial spread Miliary Bronchostenosis Tuberculoma Pleural effusions Can this be TB? Can this be TB? Findings suggestive of prior TB Ca+ granuloma – Ghon lesion Ca+ granuloma and hilar node calcification – Ranke complex Apical pleural thickening Fibrosis and volume loss