* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Core Curriculum Slides - Austin Community College
Survey
Document related concepts
Transcript
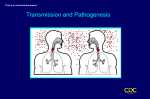
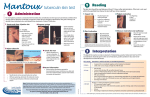
Tuberculosis Causative Organism Mycobacterium Tuberculosis Gram-positive, acid-fast bacillus (AFB) Etiology and Pathophysiology Brief exposure rarely causes infection Transmission requires close, frequent, or prolonged exposure Inhaled bacilli pass down and lodge in the alveoli Replicates slowly and spreads via the lymphatic system Body immune system responds by initiating the inflammatory response. Transmission of Tuberculosis How is Tuberculosis transmitted? Transmission of Disease Spread via airborne droplets when infected person Coughs Speaks Sneezes Sings Ask Yourself? Can the disease be spread by: Hands Books Glasses Dishes Clothing Bedding Individuals at Risk Poor, underserved Homeless persons Residents of inner-city neighborhoods Foreign-born person Older adults Those in institutions (long-term care facilities, prisons) Injection drug users Immunosuppressed Asian, native Hawaiian have highest reported cases Classification System for TB Class Type Description 0 No TB exposure Not infected No history of exposure Negative reaction to tuberculin skin test 1 TB exposure No evidence of infection History of exposure Negative reaction to tuberculin skin test 2 TB infection No disease Positive reaction to tuberculin skin test Negative bacteriologic studies (if done) No clinical, bacteriological, or radiographic evidence of active TB 3 TB, clinically active M. tuberculosis cultured (if done) Clinical, bacteriological, or radiographic evidence of current disease 4 TB Not clinically active History of episode(s) of TB or Abnormal but stable radiographic findings Positive reaction to the tuberculin skin test Negative bacteriologic studies (if done) and No clinical or radiographic evidence of current disease 5 TB suspected Diagnosis pending What can trigger reactivation of latent TB infection (LTBI) Answer: Host’s defenses become impaired Which of the following are Signs and Symptoms? Select all that apply a. Fatigue b. Non-productive cough c. Weight loss d. Sudden onset of high fever >1020 e. Night sweats f. Anorexia g. Decreased movement of chest wall Signs and Symptoms Cough becomes frequent Produces white, frothy sputum Hemoptysis is not common and is usually associated with advanced disease Complications Pleural effusion and empyema Caused by bacteria in pleural space Inflammatory reaction with plural exudates of protein-rich fluid TB pneumonia Large amounts of bacilli discharging from granulomas into lung or lymph nodes TB Skin Test (Mantoux) Uses purified protein derivative (PPD) intradermal Administering the Tuberculin Skin Test • Inject intradermally • Produce wheal 6 mm to 10 mm in diameter • Do not recap, bend, or break needles, or remove needles from syringes • Follow universal precautions for infection control Reading the Tuberculin Skin Test Read reaction 48-72 hours after injection Measure only induration Record reaction in millimeters Positive reaction => 5 mm induration – high risk persons => 10 mm induration – moderate risk persons => 15 mm induration – low risk persons Means that the person has been exposed to Tb and developed antibodies, does not differentiate between active and dormant Tb infection. Factors that May Affect the Skin Test Reaction Type of Reaction Possible Cause False-positive Nontuberculous mycobacteria BCG vaccination Anergy False-negative Recent TB infection Very young age (< 6 months old) Live-virus vaccination Overwhelming TB disease If a person has other symptoms and has a negative skin test, then the HCP would likely order a __________ ________? Chest X-Ray • Does this chest x-ray confirm the diagnosis of Tb? • Abnormalities often seen in apical or posterior segments of upper lobe or superior segments of lower lobe Arrow points to cavity in patient's right upper lobe. Bacteriologic Studies Sputum for AFB AFB (shown in red) are tubercle bacilli QuantiFERON-TB Blood is obtained from patient and placed in container with mycobacterial antigens. If the patient is infected with TB, the lympocytes in the blood will recognize these antigens and secrete interferon, a cytokine produced by lymphocytes. Test results are available in a few hours. Sputum Cultures • Use to CONFIRM diagnosis of TB • Culture all specimens, even if smear negative • Results in 4 to 14 days when liquid medium systems used Colonies of M. tuberculosis growing on media Goals of Nursing Care Goals: Comply with therapeutic regimen Have no recurrence of disease Have normal pulmonary function Take appropriate measures to prevent spread of disease Four Drug Regimen isoniazid [INH] rifampin [Rifadin] pyrazinamide [PZA] ethambutol Drug Therapy Active disease Patients should be taught about side effects and when to seek medical attention Liver function should be monitored Drug Isoniazid (INH) Side effects Noninfections hepatitis Peripheral neuropathy Hypersensitivity Nursing Implications Give B6 pyridoxine as prophylactic against peripheral neuropathy Assess for S&S of hepatitis (jaundice, yellow skin, dark urine, clay colored stools, pruritus) Take on empty stomach Avoid foods that contain tyramine and histamine (tuna, aged cheese, red wine, soy sauce, yeast extracts) Check liver enzymes, BUN, Creatinine levels monthly Rifampin (Rifadin) GI disturbances Orange discoloration of body fluids (sputum, urine, sweat, tears) Inform patient about orange discoloration of fluids/ urine Discolor contact lenses Metabolism of other meds and makes them ineffective such as cardiac meds and steroids. Drug Side effects Nursing Implications Ethambutol Retrobulbar neuritis (decreased red-green color discrimination) Get a baseline Snellen vision test and color discrimination and monthly when on high doses Pyrazinamide (PZA) Hepatoxicity, polyarthritis, Skin rash, hyperuricemia Assess for S&S of hepatitis (jaundice, yellow skin, dark urine, clay colored stools, pruritus) Monitor uric acid levels Have newer drugs with combinations of these Treatment Guidelines Initiation Phase of Treatment Multiple-medication regimen of all 4 meds Administered daily for 8 weeks Continuation Phase of Treatment d/c ethambutol and continue other 3 meds Administered for 4-7 months Patient begins to feel better in this phase Drug Therapy Latent TB infection Individual is infected with M. tuberculosis, but does not have the disease. Usually has been exposed to someone with tuberculosis. Usually treated with INH for 6 to 9 months Monitoring Response to Treatment Monitor patients bacteriologically monthly until cultures convert to negative After 3 months of therapy, if cultures are positive or symptoms do not resolve, reevaluate for Potential drug-resistant disease Nonadherence to drug regimen If cultures do not convert to negative despite 3 months of therapy, consider initiating DOT Monitoring Response to Treatment The patient asks how long before he can be considered non-contagious? What is the appropriate response? Answer this How would the nurse assess if the patient has been compliant with taking their medications? Direct Observation Therapy Used with those patients who are noncompliant and do not show signs of improvement after treatment. Noncompliance is major factor in multidrug resistance and treatment failures Provide drugs directly to the patient and watch patient swallow drugs Costly, but preferred to ensure adherence If refuses DOT then may have to put involuntarily in treatment facility to protect the community. Drug Therapy Vaccine Bacille Calmette-Guérin (BCG) vaccine to prevent TB is currently in use in many parts of the world - once person receives this vaccine, will have a false testing with the TST (TB Skin Test). For assessment, must have chest x-ray. Nursing Interventions What type of isolation is typically ordered? What PPE is worn? Who wears this equipment? What type of room are they in? Patient Teaching Cover nose and mouth with tissue when coughing, sneezing, or producing sputum Hand washing after handling sputum-soiled tissues Ambulatory and home care Fungal Infections - Who is at Risk Seriously ill patients being treated with Corticosteroids Antineoplastic drugs Immunosuppressive drugs Patients with AIDS Patients with Cystic Fibrosis Fungal Infections Histoplasmosis Pneumocystis pneumonia Cocciidiodomycosis Nocardiosis Blastomycosis Actinomycosis Cryptococcosis Aspreigillosis Candidiasis Diagnosis Skin Serology Biopsy Drug therapy Amphotericin B Intravenous Side effects Hypersensitivity reactions Fever and chills Malaise Nausea and vomiting Thrombophlebitis at injection site Pre-medicate with Benadryl to increase tolerance and decrease hypersensitivity Monitor renal function Ensure adequate hydration Drug Therapy Oral Antifungal agents ketoconazole (Nizoral) fluconazole (Sporanox; Difulcan) Flucytosine (Anobon) Monitor effectiveness with serology testing Side Effects N/V liver enzymes Bone marrow depression – monitor WBC, platelets Lung Abscess Pus-containing lesion of the lung Formed by necrosis of lung tissue Lung Abscess Causes Aspiration of material from GI tract into lungs Lung cancer Tuberculosis Signs and Symptoms Productive cough of purulent foul smelling and foul tasting sputum Fever and chills Pleuritic pain Dyspnea Weight loss Diagnosis Sputum cultures – obtained first so can confirm treatment modalities Chest x-ray Bronchoscopy Treatment and Nursing Care Drug Therapy- Antibiotics Penicillin Clindamycin **Large doses of IV are required because the antibiotic must penetrate the necrotic tissue and fluid in the abscess. **May need to make home health referral for IV to be given at home Antipyretics Chest physiotherapy and postural drainage Treatment and Nursing Care Drug Therapy Increase fluid intake Rest Good nutrition Nursing Care How do you know if the treatment is effective?