* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Effect of Ischemia on Calcium-Dependent Fluorescence
Cardiac contractility modulation wikipedia , lookup
Coronary artery disease wikipedia , lookup
Heart failure wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Electrocardiography wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
1047
Effect of Ischemia on
Calcium-Dependent Fluorescence Transients
in Rabbit Hearts Containing Indo 1
Correlation with
Monophasic Action Potentials and Contraction
Hon-Chi Lee, MD, PhD, Rajendra Mohabir, PhD, Nellis Smith, MD,
Michael R. Franz, MD, and William T. Clusin, MD, PhD
Downloaded from http://circ.ahajournals.org/ by guest on June 12, 2017
The effects of acute global ischemia on cytosolic calcium transients were studied in perfused
rabbit hearts loaded with the fluorescent calcium indicator indo 1. Indo 1-loaded hearts were
illuminated at 360 nm, and fluorescence was recorded simultaneously at 400 and 550 nm from
the epicardial surface of the left ventricle. The F4m/F550 ratio was calculated by an analog circuit,
which allowed cancellation of optical motion artifact. Resulting calcium transients demonstrated a rapid upstroke and slow decay similar to those recorded in isolated ventricular
myocytes. Global ischemia rapidly suppressed contraction, but it produced a concurrent
increase in the systolic and diastolic levels of the calcium transients, together with an increase
in the duration of the peak. The effects of ischemia were reversed by reperfusion, inhibited by
verapamil, and mimicked by perfusion of nonischemic hearts with acidified (C02-rich) solution.
In addition to elevation of the calcium transients, ischemia caused a pattern of intracellular
calcium alternans that was discernible after 2-3 minutes. The pattern of alternans was stable
at a given epicardial site, but it could be out of phase at different sites. Similar nonuniformities
were observed in contraction strength and in the duration of monophasic action potentials
recorded immediately adjacent to the fiber-optic probe. Abnormalities in intracellular calcium
may be a causal factor in the loss of electrical and mechanical synchrony in the acutely ischemic
heart. (Circulation 1988;78:1047-1059)
C essation of blood flow causes rapid changes
in the electrical and mechanical activity of
the heart. The resting potential of ischemic
cells declines promptly, which inactivates sodium
channels and slows conduction.' The duration of
the action potential is modified to varying degrees
so that recovery of excitability no longer occurs in
the normal, orderly sequence. The combination of
slowed conduction and nonuniform excitability leads
to vulnerability of the ischemic heart to ventricular
From the Division of Cardiology, Stanford University School
of Medicine, Stanford, California 94305.
Supported by Grant HL-32093 from the National Institutes of
Health and by a Grant-in-Aid from the American Heart Association, California Affiliate. N.S., H-C.L., and R.M. were recipients of individual post-doctoral fellowships from the National
Institutes of Health, the American Heart Association, California
Affiliate, and the Canadian Heart Foundation. W.T.C. is an
Established Investigator of the American Heart Association.
Address for correspondence: Hon-Chi Lee, MD, PhD, Division of Cardiology, Stanford University School of Medicine,
Stanford, CA 94305.
Received October 14, 1987; revision accepted May 26, 1988.
fibrillation.2 Changes in electrical activity are accompanied by profound impairment of mechanical performance. Ischemia causes a marked decrease in
contraction strength, along with alternation of contraction strength from beat to beat. The mechanism
of ",mechanical alternans" during ischemia has not
been established, but it presumably involves fluctuation in the level of cytosolic calcium ([Ca2`ji) that
is transiently achieved during the action potential.
Changes in membrane potential during ischemia
may also result from abnormalities in [Ca2+1L.3
"Calcium overload" mimicks the effects of ischemia by reducing the resting potential and by changing the configuration of the action potential in a
characteristic way. These effects are mediated either
by "calcium-activated" cation channels4'5 or by
electrogenic sodium-calcium exchange.6-10 Because
both of these processes are practically instantaneous, variations in the [Ca2+]i transient from beat
to beat would cause concomitant changes in the
action potential plateau.
1048
Circulation Vol 78, No 4, October 1988
Downloaded from http://circ.ahajournals.org/ by guest on June 12, 2017
To clarify the role of [Ca2"j1 in ischemia, we have
devised a method of recording [Ca2]i-dependent
fluorescence transients from rabbit hearts loaded
with the fluorescent calcium indicator indo 1. This
method involves arterial perfusion of the hearts with
the cell-permeant form of the indicator, indo 1-AM,"'
which has been used previously in isolated cardiac
myocytes. 12-14 The present experiments are designed
to study changes in the calcium transients during
ischemia as well as the mechanism by which the
transients are altered. We find that ischemia causes
rapid elevation of the calcium transients, which is
simulated by elevation of CO2 and is prevented by
pretreatment with verapamil. Ischemia also causes
spatial and temporal variations in the amplitude of the
transients, which correspond to inhomogeneities in
contraction strength and action potential duration.
These observations suggest that cytosolic calcium
abnormalities contribute to the loss of synchronized
excitation in the acutely ischemic heart.
Materials and Methods
Preparation of Isolated Hearts
Albino male New Zealand rabbits weighing
between 1.8 and 2.2 kg were killed by cervical
fracture. The heart was rapidly excised and perfused
with saline solution at a constant flow rate of 20-30
ml/min. The perfusate contained NaCI 115 mM, KCl
4.7 mM, CaCI2 2.0 mM, MgC12 0.7 mM, NaHCO3 28
mM, NaH2PO4 0.5 mM, glucose 20 mM, insulin 10
units/l, and fetal calf serum 0.1%; the perfusate was
adjusted to pH 7.4, equilibrated with 95% 02-5%
C02, and heated to maintain the heart at 30 ± 10 C.
Left ventricular pressure was recorded with an isovolumic intracavitary latex balloon that contained a
fiber-optic pressure transducer (Camino Laboratories, San Diego, California). Simultaneous recordings of local contractile activity were obtained with a
piezoelectric epicardial strain gauge, the transducing
pins of which were 4 mm apart. In some experiments, the ventricular action potential was recorded
from the surface of the heart with a "contact"
monophasic action potential electrode, which is
known to respond linearly to changes in membrane
potential.15,16 Most recordings were obtained during
rapid pacing of the right ventricle (180 beats/min) by
an epicardial plunge electrode.
Fluorescence Recordings
Recordings were obtained from the anterior surface of the left ventricle except where otherwise
stated. Illumination from a 100 W mercury vapor
lamp was filtered at 360 ± 5 nm and directed through
a silica fiber-optic cable onto the surface of the
heart. The fiber-optic cable terminated in a plastic
receptacle, which was attached to the heart by a
plastic sleeve and rubber girdle that were designed
to minimize relative motion. The plastic sleeve was
opaque, and it confined the illumination beam to a
circular region of the ventricular surface 1 cm in
diameter. Fluorescence emissions were collected
by a ring of smaller fiber optics and were directed
through a beam splitter into two photomultipliers
fitted with optical band-pass filters centered at 400
and 550 nm. The output of the photomultipliers was
passed into an electronic ratio circuit so that the
fluorescence ratio (F400/F550) could be obtained. Fluorescence at individual wavelengths, the F400/F550
ratio, and other physiological signals were displayed on a Gould-Brush strip chart recorder (Cleveland, Ohio). Indo 1-AM was solubilized in dimethyl
sulfoxide containing pluronic F-127 (25% w/v) and
infused into the heart at a final concentration of 2.5
,gM, in the presence of 5% fetal calf serum. Perfusion with indo 1-AM continued for 30 minutes,
followed by a 30-minute washout. This procedure
caused the fluorescence of the heart to increase by
a factor of 5-12 compared with the fluorescence
obtained before loading (autofluorescence).
Differential Centrifugation, Manganese
Quenching, and Electron Microscopy
To confirm that infused indo 1-AM is converted
to the calcium-sensitive free acid, manganese
quenching studies were performed. Low concentrations of manganese are known to quench completely the fluorescence of indo 1 free acid, while
having no effect on the calcium-insensitive fluorescence of indo 1-AM.17 In three hearts loaded with
indo 1, 20 mM MnC12 was infused in the presence of
the ionophore ionomycin (1.5 ,M), which transports Mn' ions into the cell interior. Manganese
promptly quenched more than two thirds of the
fluorescence in all three hearts, which indicates that
most of the fluorescence arose from indo 1 free
acid. Postmanganese fluorescence was, however,
significantly higher than the autofluorescence level
(172 ± 5% of autofluorescence at 400 nm and
161 +±5% of autofluorescence at 550 nm), which
indicates that there was retention of incompletely
hydrolyzed indo 1-AM. The presence of incompletely hydrolyzed indo 1-AM complicates conversion of the fluorescence ratios to [Ca2 ]i.17
To define further the localization and fate of indo 1
in the intact heart, tissue homogenates were fractionated by differential centrifugation. 18 One gram of
myocardium was excised from the anterior left ventricular wall of an indo 1-loaded heart at the same
site where [Ca2']i-dependent fluorescence transients
had previously been recorded. The specimen was
minced and suspended in 5 ml of a buffer containing
0.25 M sucrose, 115 mM KCI, 20 mM NaCI, 1.115
mM MgCl2, 1.115 mM ethyleneglycol-bis-(Qaminoethyl ether)-N,N,N',N'-tetraacetic acid
(EGTA), and 10 mM N-(2-hydroxyethyl)piperazineN'-2-ethanesulfonic acid (HEPES), which was
adjusted to pH 7.05 at 40 C. The specimen was then
homogenized with a Polytron instrument (Brinkman
Instruments, Westbury, New York) operated twice
at full speed for 30 seconds. The crude homogenate
was spun at 40g in a Damon/IEC HN-SII centrifuge
(Needham Heights, Massachusetts) for 10 minutes to
Lee et al Ischemia and Calcium-Dependent Fluorescence Transients
Downloaded from http://circ.ahajournals.org/ by guest on June 12, 2017
remove intact cells. Ultracentrifugations were then
performed with a TY 65 rotor in a Beckman L5-65
ultracentrifuge (Irvine, California). The supernatant
from the crude homogenate was spun at 1 ,OOOg for 20
minutes to remove large organelles and subcellular
debris (nuclear fraction). The supernatant was then
spun at 10,000g for 20 minutes to isolate mitochondria (mitochondrial fraction). A third ultracentrifugation was then performed at 105,000g for 120 minutes
to obtain the microsomal fraction, with the final
supernatant being the cytosol fraction. The three
ultracentrifugation pellets were resuspended in 5-ml
aliquots of buffer, and 1 ml of each fraction was
placed in a quartz cuvette for measurement of fluorescence. Fluorescence was recorded at an excitation wavelength of 360 nm and an emission wavelength of 400 nm. For each cuvette, calcium-specific
fluorescence was determined as the difference between F. and FMj2 +, where Fm., was obtained by
addition of 25 ,ul 100 mM CaCl2 to the cuvette and
FM2 + was obtained by addition of 50 ,l 100 mM
MnCl2. The total calcium-specific fluorescence of the
homogenate was then calculated as the sum of
calcium-specific fluorescence for each of the three
ultracentrifugation pellets plus the calcium-specific
fluorescence of the final supernatant. The percentage
of total calcium-specific fluorescence in each fraction
was then determined with the following results:
cytosol fraction = 72.2%, mitochondrial fraction =
3.6%, microsomal fraction= 3.4%, and nuclear
fraction = 20.8%. These results indicate that most of
the calcium-specific fluorescence, which arises from
indo 1 free acid, was located in the soluble cytosolic
fraction. Very little indo 1 free acid was contained in
the mitochondria. Although it is possible that some
of the mitochondria were disrupted during homogenization of the tissue, a conclusion similar to ours
has been reached by Steinberg and others,19 who
used a nondisruptive technique (rhodamine dual fluorescence microscopy) to study the subcellular fate
of indo 1-AM.
F400
1.9
to
LLto
0
IL
1.5
L
V-At
F550
0
1.0
sec
1049
The distribution of incompletely hydrolyzed indo
1-AM in the tissue homogenate could be deduced
from the amount of fluorescence not quenched by
manganese (FMj2 + .,,F; expressed in a percentage). For the cytosolic fraction, only 2.1% of the
Fmaxfluorescence was resistant to quenching, which
implies that practically all of the cytosolic indo 1 is
composed of the free acid. In contrast, a greater
portion of the fluorescence was resistant to quenching in the other fractions (36.6%, 31.5%, and 17.7%
for the mitochondrial, microsomal, and nuclear
fractions, respectively). These observations suggest
that retained indo 1-AM is largely associated with
organelles.
To further confirm the distribution of indo 1
described above, a sample of the four fractions was
submitted for electron microscopy. The microscopist was blinded as to the identity of the fractions.
Electron microscopy showed that mitochondria were
abundantly present in the mitochondrial fraction
and were not present in other fractions. The microsomal fraction contained clear membrane-bound
vesicles that were presumably of sarcoplasmic reticular origin, whereas the cytosol fraction contained
no electron dense material.
In Vitro pH Sensitivity of Indo 1
For indo 1 to be accepted as an indicator of [Ca2+]i
during ischemia, it was necessary to determine
whether the fluorescence or calcium sensitivity of
the indicator is altered by moderate acidification.
These determinations were made by illuminating
vials containing indo 1 free acid at varying pH with
the same fiber-optic apparatus that was used for
intact hearts. Three titration curves (pH vs. the
F400/F550 ratio) were constructed, one for an indo 1
solution that was saturated with calcium, one for an
indo 1 solution in the calcium-free form, and one for
a solution in which indo 1 was partially saturated so
that the fluorescence ratio was similar to that obtained
in the intact heart. All three solutions contained
FIGURE 1. Recordings of [Ca+i-Jdependent fluorescence transients from the surface of a rabbit heart
containing indo 1. Three transients are shown in which
fluorescence increases at 400 nm (top trace) and
decreases at 550 nm (bottom trace). Middle trace
shows the fluorescence ratio, F40olF55o, which is a
monotonic function of [Ca2+]j.11 Calcium transients
are similar to those obtained in isolated cardiac
myocytes containing indo 1,12-14 or the related indicatorfura-2.29,30 The calcium transient represents a 5%
variation in the totalfluorescence at 400 nm and a 7%
variation in fluorescence at 550 nm. The autofluorescence signal, measured before loading with indo 1,
represents 9% of the total fluorescence at 400 nm and
12% of the total fluorescence at 550 nm. Absolute
signal strengths were approximately 106 photonslsec
after loading.
1050
Circulation Vol 78, No 4, October 1988
(mM) KCl 115, NaCI 20, MgCl2 1.115, and HEPES
10, and they were adjusted to an initial pH of 7.4.
The calcium-free solution contained EGTA 1.115 mM
and indo 1 1 ,uM. The calcium-saturated solution
contained CaCI2 5 mM and indo 1 1 ,uM. The partially
saturated solution contained indo 1 21 ,M and CaCl2
10 ,M. Each solution was acidified by stepwise
addition of small aliquots (10-50 ,ul) of IN HCI.
Resulting pH changes were measured with an Instrumentation Laboratory (Lexington, Massachusetts)
Model 282 Co-oximeter. Measurements ofthe F4m/F550
ratio were obtained at four to eight different pH values
for each solution, which ranged between 5.8 and 7.4.
Results
[Ca2+]i-Dependent Fluorescence Transients
Under Baseline Conditions
Downloaded from http://circ.ahajournals.org/ by guest on June 12, 2017
Hearts loaded with indo 1 exhibit [Ca2+lidependent fluorescence transients (Figure 1), which
are not present before loading. Calcium transients
rise more steeply than the contraction (Figure 2) and
have the same shape as those observed in cardiac
myocytes containing indo 1.12-14Transients are clearest in the F400/F550 ratio (Figure 1, middle trace),
which reflects reciprocal changes at the two emission
wavelengths. Transients are also clear in the individual fluorescence signals, where the systolic increase in
[Ca2+]i produces a phasic increase in fluorescence at
Transients
During Ischemia
A primary reason for recording calcium tran-
sients in intact hearts is to determine the effects of
1.7
U-
0
0
LL
[Ca2"]i-Dependent Fluorescence
j.y111,-.
1.4
1.7 -
ANTERIOR
1.41.7
APEX
INDO-1
CONTROL
0
L0
10
400 nm (top trace) and a phasic decrease in fluorescence at 550 nm (bottom trace). The calcium transients represent, a 5% and 7% variation in the total
fluorescence at 400 and 550 nm, respectively. Corresponding autofluorescence levels are 9% and 12%.
Onset of the fluorescence transients coincides
with, or slightly precedes, the onset of ventricular
contraction (Figure 2, right panel). The contractions
of indo 1-loaded hearts are not reduced in amplitude or increased in duration compared with
unloaded hearts, which indicates that there is no
significant buffering of [Ca2 ji by the indicator.
Fluorescence transients are uniform from one heart
to the next and can be recorded from any portion of
the left ventricular surface or from the right ventricle. Figure 3 shows calcium transients recorded
from three nonoverlapping regions of the left ventricle of a single heart. All 15 transients are similar
in time course and have similar ratio values.
to
1"1.
1
LL
0
Q
[ j
v~
jJ
h
A
11
1/ \ 1/ \
I
,1 X~
1K
E
E
0
0.5
sec
0
0.5
1.0
sec
1. .
\
1
1.4
1.7 -
LATERAL
1
.
1.5
FIGURE 2. Simultaneous recordings of calcium tran-
sients (top right) and ventricular pressure (bottom right)
in a heart loaded with indo 1. Isovolumic left ventricular
pressure is measured with an intracavitary latex balloon
containing a fiber-optic pressure transducer. Peak systolic pressure is 100 mm Hg. The left-hand recording
shows intraventricular pressure in the same heart before
loading with indo 1. Loading of the heart with indo 1 does
not reduce systolic pressure and does not slow the time
course of relaxation compared with the control recording
(bottom left). These observations indicate that there is no
significant buffering of [Ca2 li by the indicator. F40JF550
ratio was not recorded in this heart before loading with
indo 1, but results of such a recording are shown in
Figure 4B. Possible effects of dimethyl sulfoxide and
Pluronic F-127 alone were tested in one heart, and no
change in ventricular pressure was found.
1.4r
,
A,
1.4
0
1
2
sec
FIGURE 3. Recordings of calcium transients from three
different portions of the surface of the left ventricle of a
rabbit heart containing indo 1. Each recording is from a
i-cm circular region whose boundary is defined by the
edge of the plastic sleeve that contains the fiber-optic
cables. The recordings have been obtained by manually
positioning the fiber-optic assembly on the anterior surface (top trace), the apical surface (middle trace), and the
lateral surface (bottom trace) of the left ventricle. The
recordings are nonsimultaneous but are aligned in the
figure to facilitate comparison among the calcium transients. Allfifteen transients have approximately the same
time course and the same fluorescence ratio values.
Different results are obtained when the heart has been
ischemic for several minutes (see text).
Lee et al Ischemia and Calcium-Dependent Fluorescence Transients
1051
A
REPERFUSE
1 ISCHEMIA
v
1.9
LO
F~~~~~~~~~~~~~~.
1.wim
'to
LL
"OM"
0'
UC)
1Ll..l.id.A
&
L
I 11.1..I
I.
d
1.
1.
1
1U-
1.4
-r
100 [1
cm
E
E
nTl
lr I, ` IT,
',
ihdu.
1
Tip
lipr_
ii - j_---A
MM
1m""T.M
"V"l
r''1
-
---------------
I
m
OL
0
90
60
30
120
150
sec
B
Downloaded from http://circ.ahajournals.org/ by guest on June 12, 2017
0
to
U')
REPERFUSE
1.5[ ISCHEMIA
LL
to
0
LL
2
n 7
U. I -
N~~~~~~~~~~~~------
100
90
30
sec
FIGURE 4. Recordings of effects of ischemia on calcium transients (Panel A, top) and left ventricularpressure (Panel A,
bottom) in a heart containing indo 1. Ischemia is produced by cessation of coronary perfusion for 60 seconds while the
heart is paced at 180 beatslmin by an epicardial plunge electrode. Baseline systolic pressure is above 100 mm Hg.
Ischemia produces a prompt decline in pressure, along with progressive elevation of the calcium transients, which begins
S seconds later. Reperfusion causes return of both signals to their original levels but with a temporary impairment of
relaxation that may be due to elevation of diastolic [Ca2+]. Panel B is a recording of the F400 Fs50 autofluorescence ratio
during ischemia and reperfusion in a heart not yet loaded with indo 1. Beat-to-beat calcium transients are notably absent,
and there is no effect of ischemia (which begins at time 0) on thefluorescence ratio. Subsequent loading ofthis heart with
indo 1 produced very prominent calcium transients (shown in Figures 1 and5), whose net amplitude wasfurther increased
by ischemia (Figure 5). Loading of the heart with indo 1 produced an 8.3-fold increase in the absolute fluorescence
intensity at 550 nm and an 11.1-fold increase at 400 nm. The heart was paced at 180 beatslmin throughout the recording.
0
10
20
ischemia, which can only occur in perfused tissue.
Figure 4A shows the effect of a 60-second episode
of global ischemia, during which the heart is paced
at 180 beats/min. Ischemia produces a prompt
increase in the peak amplitude of the calcium transients, along with an upward shift of the baseline, so
that the F4m/F55o ratio at end diastole approaches the
normal systolic value. In most cases, the systolic
fluorescence ratio increases more rapidly than the
diastolic ratio so that the net amplitude of the
calcium transients becomes larger (Figures 5 and 6).
Net amplitude reaches a maximum value between
45 and 60 seconds, after which both ratios increase
more slowly. The shape of the calcium transients
also changes during ischemia so that the peak
becomes broader and the terminal decay more
abrupt (Figure 7). All of these effects can be discerned in recordings obtained at single wavelengths
(Figure 5) as well as in the F40o/F550 ratio. The effects
of ischemia are reversed by reperfusion for 60-90
seconds (Figure 4A), are reproducible during a
series of three to six ischemic trials, and are consistent in a series of hearts for which the mean
change in F4m/F550 ratio is shown in Figure 6.
Elevation of the calcium transients during ischemia
is accompanied by an equally prompt decrease in
contraction strength (Figure 4A), which is presumably due to a decrease in the calcium sensitivity of
the myofilaments.20,21 The contractile response
recovers during reperfusion, and there is a temporary impairment of relaxation, which may be due to
persisting elevation of [Ca2+]i.
Effects of Ischemia Are Not Due to
Changes in Autofluorescence
The effects of ischemia on the calcium transients
are not due to changes in epicardial temperature,
changes in pH (see below), or changes in autofluorescence. There are three reasons why autofluorescence changes cannot explain the effects of ischemia on the F400/F550 ratio:
1) In contrast to the behavior of indo 1 fluorescence, changes in autofluorescence during ischemia
are parallel at 400 and 550 nm; both signals show a
moderate increase. These changes cancel in the
F4m/F550 ratio so that the ratio remains constant
(Figure 4B). When recordings from the same heart
are compared before and after loading with indo 1,
1052
Circulation Vol 78, No 4, October 1988
CONTROL
ISCHEMIA
REPERFUSE
0
0
rr.It~
.........................
Lli
z
LlJ
c)
1F
\
11
1-1
0
0
L11
D
\,-.
Ul
U-
z
IU
z
C)
sec
F550
.........................
L
L
Downloaded from http://circ.ahajournals.org/ by guest on June 12, 2017
0.4
0
sec
0
0.4
sec
FIGURE 5. Recordings of effects of ischemia on calcium
transients at individual wavelengths. Fluorescence transients at 400 nm (top trace) and 550 nm (bottom trace) are
shown together with the F40JF550 ratio (middle trace).
Right panels obtained at 50 seconds of ischemia, and left
panels obtained immediately before ischemia. Ischemia
increases the net amplitude of the calcium transient in all
three recordings. End-diastolicfluorescence increases at
400 nm and decreases at 550 nm, which leads to a
comparable increase in the end-diastolic fluorescence
ratio. As in Figure 4A, the effects are reversed by
reperfusion (not shown). Recordings are obtained from
the same heart as Figure 1, but the heart is now paced at
180 beatslmin. Dotted lines in right panels show initial
end-diastolic signal levels.
the effect of ischemia at 550 nm is converted from a
fluorescence increase to a fluorescence decrease
(Figure 5, bottom traces). This fluorescence decrease
is indicative of a rise in [Ca2']j.
2) Changes in autofluorescence could not, in principle, explain the increased net amplitude of the
fluorescence transients. Changes in autofluorescence
should have no effect on the amplitude of fluorescence transients at single wavelengths. Furthermore,
an increase in autofluorescence at both wavelengths
should diminish the transients observed in the ratio.
3) Changes in indo 1 fluorescence during ischemia
are larger than the changes in autofluorescence. This
point is particularly important for the 400 nm signal,
where the effect of a [Ca2 ]i increase can be mimicked
by an increase in autofluorescence. For the experiment in Figure 5, the increase in 400 nm end-diastolic
fluorescence during 90 seconds of ischemia is 2.7
times greater than the increase in autofluorescence
during an ischemic trial that preceded infusion of
indo 1-AM. Although the increase in autofluorescence
causes some overestimation of indo 1 fluorescence at
400 nm (Figure 5, top), this effect is balanced by
FIGURE 6. Plot of relative change in the calcium transient produced by ischemia and reperfusion in 11 hearts.
Fluorescence ratios from each heart have been converted
to a percentage of the end-diastolic value at the onset of
ischemia. Ischemia causes a progressive increase in peak
systolic and end diastolic fluorescence ratio, which is
reversed by reperfusion. Net amplitude of the calcium
transient (peak systolic ratio minus end-diastolic ratio)
increases during ischemia and tends to be largest at 4560 seconds. Bars indicate SEM.
partial masking of the [Ca2+]i-dependent fluorescence
decrease at 550 nm. Net effects have been determined
by deconvolution of the F4m/F550 ratio, and these
calculations show that autofluorescence changes have
no significant effect on the ratio and do not contribute
to the increase in the ratio during ischemia.
Alternans Behavior of Calcium Transients
Consecutive calcium transients remain uniform
throughout the 1st minute of ischemia. However, in
the 2nd or 3rd minute, a characteristic nonuniformity develops in which every other transient is diminished in amplitude and arises from a higher enddiastolic level (Figure 7A). This pattern of alternation
is stable at any given site on the ventricular surface.
However, when the fiber-optic probe is moved to a
different site during a continuous recording, the
pattern of alternation may reverse so that if odd
numbered transients were larger at the first site,
they are smaller at the second site. This observation
indicates that the alternans behavior of calcium
transients within a 1-cm circular region is independent of the behavior in other regions.
Nonuniformity of the calcium transients is associated with similar variations in contraction strength.
Contractions in Figure 7B, for example, exhibit
alternations in amplitude during ischemia that are
similar to the alternations of the calcium transient
described above. Alternations are seen in both the
intraventricular pressure recording (top trace) and
in the contractions recorded by a strain gauge
transducer, which has an inter-pin distance of 4 mm
(bottom trace). However, as shown by the arrows,
the pattern of alternation is out of phase in the two
recordings so that weak contractions recorded by
Lee et al Ischemia and Calcium-Dependent Fluorescence Transients
CONTROL
A
0
1053
ISCHEMIA
1.9
:°L.
20
1<
2)
1
0
..........................
3
2
0
1.8
sec
LL
U-
1.4
B
,,
0.5
0
sec
If
20
I
E
E
OL
Downloaded from http://circ.ahajournals.org/ by guest on June 12, 2017
11
0
11
-1
11
2
1
3
sec
FIGURE 7. Recordings of alternation of contraction
strength and calcium transients after 3 minutes of ischemia. Panel A shows alternation of the F4o IF55o fluorescence ratio. Even numbered beats have smaller calcium
transients that arise from a higher end-diastolic level and
are followed by more complete decay. Despite the alternans pattern, all of the calcium transients have higher
peak systolic and end-diastolic values than those recorded
before ischemia (not shown). Panel B shows alternation
of contractions recorded by an intracavitary balloon (top
trace) and by an epicardial strain gauge transducer (bottom
trace). Alternans pattern is similar in the two recordings,
but it is out ofphase so that strong contractions recorded
by the balloon (top arrow) coincide with weak contractions
recorded by the strain gauge (bottom arrow). This result
implies that alternans develops independently in different
regions of the ventricle and that the pattern recorded by
the intracavitary balloon represents a net imbalance in the
summated activity of different regions.
the strain gauge correspond to strong contractions
recorded from the entire ventricle. This result implies
that variations in contraction strength occur independently in localized regions of the heart. This
interpretation has been confirmed by simultaneous
recordings with two strain gauge transducers. Ischemia causes alternations in the strength of contraction recorded by each transducer, but these alternations do not develop simultaneously, and they are
often out of phase.
Correlation of Calcium Transients With
Monophasic Action Potentials During Ischemia
Changes in the calcium transient during ischemia
are accompanied by changes in membrane potential. Ischemia causes reduction of the resting poten-
0
0.5
0
0.5
sec
FiGURE 8. Recordings of effects of ischemia on the
calcium transient (bottom trace) and monophasic action
potential (top trace) in the same heart. A 90-second
episode of ischemia (right) causes reduction of the resting
potential, broadening of the action potential, and slowing
of conduction, which is indicated by an increase in the
time from stimulus to action potential onset. Ischemia also
increases both the peak systolic and end-diastolic level of
the calcium transient and causes broadening of the peak.
Dotted line indicates the original monophasic action potential resting potential before ischemia.
tial, which occurs within the 1st minute of rapidly
paced occlusions and is reversed by reperfusion.
Reversible depolarization during ischemia can be
monitored with "floating" microelectrodes, or with
monophasic action potential electrodes. 15,16 Recordings of the latter type are illustrated in the top trace
of Figure 8. Reduction of the resting potential is
accompanied by an upward shift in the calcium
transient recorded from an adjacent site. The
increase in the diastolic fluorescence ratio in Figure
8 would be consistent with the possibility that
increased [Ca2"]i causes changes in membrane permeability that reduce the resting potential of the
isc(hemic cells.22
Ischemia also causes initial broadening of the
action potential (Figure 8, top right), which has
been demonstrated previously by microelectrode
impalement in the dog heart,23 and by suction
monophasic action potential recordings in the pig
heart.24 Broadening of the action potential is accompanied by elevation and broadening of the calcium
transient (Figure 8, bottom right), which is reversed
by reperfusion. Elevation of the calcium transient in
Figure 8 could be a consequence of action potential
broadening or could cause this broadening by inducing calcium-activated inward currents across the
membrane of the myocardial cell.6-'0 The latter
interpretation is suggested by the marked shortening of the action potential that occurs when the
calcium transients of rabbit myocardium are deliberately abolished by the drug ryanodine, which
inhibits calcium release from the sarcoplasmic
reticulum.25
1054
Circulation Vol 78, No 4, October 1988
A
20-
<1 I
O
-~~~1
0
0
IC)
1.9
U-)to
0
LL 1
iV>{V\>
/1>.
g; -_ -\j
11,1
.;
0
1.0
0.5
sec
B
20-
mV
Downloaded from http://circ.ahajournals.org/ by guest on June 12, 2017
0-
0
0.2
0.4
sec
FIGURE 9. Recordings of simultaneous calcium transients and action potentials after 2 minutes of ischemia
(Panel A). Duration of the action potential alternates
from beat to beat, as does the peak amplitude of the
calcium transient. End-diastolic level of the calcium
transient also exhibits fluctuations so that the lower
amplitude transients (second and fourth) arise from a
higher starting point. Panel B shows photographic superimposition of long- and short-duration action potentials
from Panel A. Action potentials are nearly identical
during the first 80 msec and do not diverge until after the
calcium transient has reached its peak. This observation
indicates that variations in the amplitude of the calcium
transient are not a direct consequence of variations in
membrane potential. Fluctuations of the calcium transient
in Panel A are not an artifact of motion, as can be shown
by comparison of the F400/F550 ratio with recordings at
single wavelengths. Calcium transients in Panel A all
reach a peak systolic value that exceeds the preischemic
value of 1.6.
Consecutive action potentials are uniform during
the 1st minute of ischemia. However, in the 2nd or
3rd minute, a pattern of nonuniformity often develops in which action potential duration alternates
from beat to beat (Figure 9A, top trace; and Figure
9B). When action potentials and calcium transients
are recorded from adjacent sites, the broader action
potentials coincide with the larger calcium transients (Figure 9A, bottom trace). Changes in the
action potential are most prominent during repolarization and are minimal during the upstroke (Figure
9B). There is substantial variation in the upstroke of
the calcium transients (first 80 msec), even though
the corresponding action potentials are superimposible during this time (Figure 9B). This observation
shows that the changing amplitude of the calcium
transients is not due to fluctuations in excitability or
conduction. Alternation of the transients is more
likely to result from variations in intracellular calcium release, which is the primary source of the
calcium that gives rise to the transients.26
A further implication of Figure 9 is that alternation of action potential duration can occur independently in discrete regions of the ischemic heart so
that the pattern of alternation in a particular region
can either be in phase or out of phase with some
other region. We have confirmed this inference
directly in two ischemic hearts where simultaneous
monophasic action potential recordings were
obtained at two different sites. Localization of monophasic action potential alternans to specific regions
of the myocardium has also been reported in the
ischemic pig heart24 and is consistent with the
behavior we observed for the calcium transient and
contraction (Figure 7B).
Verapamil Blocks Effects of
Ischemia on Calcium Transients
The role of [Ca2"]i in the physiology of ischemia
could be tested further if it were possible to block
the ischemia-induced [Ca2"]i increase. Electrophysiological manifestations of ischemia are prevented
by drugs that reduce calcium influx, and it has been
postulated that reduction of [Ca2+]i is the basis for
this action.3 Figure lOA shows the effect of a
5-minute infusion of verapamil (0.25 ,M) on the
ischemia-induced increase in the F4m/F550 ratio. The
top two plots (circles) show the fluorescence ratio
during an ischemic trial before verapamil, whereas
the bottom two plots (triangles) depict a second trial
performed after verapamil infusion. Verapamil
reduces the net amplitude of the calcium transient
before ischemia (leftmost triangles) and reduces the
end-diastolic level from which the transients arise
(open triangle at left). Elevation of the calcium
transients during ischemia is nearly abolished by
verapamil so that the effect of verapamil on the
F400/F550 ratio is larger during ischemia than in the
preischemic period. Comparable results have been
obtained in six ischemic hearts, for which mean
values are listed in Table 1. The increase in the
fluorescence ratio during ischemia is significantly
reduced by verapamil (Table 1, first and second
rows from top) as is the net amplitude of the
calcium transients (Table 1, third and fourth rows
from top). The bottom row of Table 1 gives the
ischemia-induced increase in the calcium transient,
which is calculated by subtracting the net amplitude
of the transient before ischemia from the net amplitude at 1 minute of ischemia. The increase in the
transient is threefold smaller after verapamil infusion. The above effects were partly reversible in
four hearts where a third ischemic trial was performed after washout of verapamil for 15 minutes.
Figure lOB shows the effect of a higher concentration of verapamil (3.0 ,uM) in five ischemic hearts.
This concentration abolishes the calcium transients
and contractions but does not abolish the monopha-
Lee et al Ischemia and Calcium-Dependent Fluorescence Transients
* ° CONTROL
A A VERAPAMIL
A
2.00
0
o
U)
Ut
LL
0
L1
1.75
0
A
z
1.50
W
0
cn
cc
0
19R
1LL 9zE
,
90
U-
0
30
60
,
120
150
sec
B
Downloaded from http://circ.ahajournals.org/ by guest on June 12, 2017
A VERAPAMIL
10
0
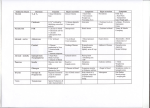
TABLE 1. Effects of Verapamil and Ischemia on [Ca2i]iDependent Fluorescence Transients in Six Hearts
Control trial Verapamil trial
0.04 0.02*
Ischemia-induced increase in 0.12±0.03
diastolic fluorescence ratio
0.05 ± 0.02t
Ischemia-induced increase in 0.15 ± 0.03
systolic fluorescence ratio
0.09±0.01t
0.12+0.01
Net amplitude of [Ca2+]i
transient before ischemia
0.10-0.0t
0.15 ±0.01§
Net amplitude of [Ca2+]i
transient at 1 minute of
ischemia
0.01±0.01*
Ischemia-induced increase in 0.03 ±0.01
[Ca2+]i transient
Values are mean ± SEM.
Values are calculated from normalized ratios for which the
end-diastolic ratio at the beginning of the control trial (before
ischemia) is defined as 1.00. 0.25 ,M verapamil was administered; ischemia lasted for 60 seconds.
*p<0.05, tp<0.005,
compared
value. with control trial;
preischemic
compared withtp<0.01
§p<0.005
i3.0 ,M verapamil compared with values from
^-~---~
0
30
60
90
120
150
sec
FIGURE 10. Plots of effect of verapamil on calcium
transients during ischemia. Panel A shows data from a
single heart in which two 90-second ischemic trials have
been performed, one before and one after infusion of 0.25
,uM verapamil. Peak systolic values of the F40ojF55o ratio
are plotted as solid symbols, whereas end-diastolic values are plotted as open symbols. The first ischemic trial
(circles) increases the net amplitude of the calcium transients and elevates the end-diastolic level from which
they arise. These effects are reversed by reperfusion.
Verapamil infusion begins 5 minutes later and continues
for an additional 5 minutes. Verapamil reduces the net
amplitude of the calcium transients (triangles), and
reduces the end-diastolic level as well. Ischemia has little
effect on the calcium transients after verapamil infusion,
but the effect of ischemia is partly restored in a third trial
performed after washout ofverapamilfor 15 minutes (not
shown). Panel B shows relative changes in the F4001F550
ratio in five ischemic hearts pretreated with 3 ,M verapamil. For each heart, the F4001F550 ratio is measured at
15-second intervals and is expressed as a percentage of
the end-diastolic value just before verapamil infusion. 3
,M verapamil causes profound inhibition of the calcium
transients so that the systolic peaks cannot be measured.
Verapamil reduces the diastolicfluorescence ratio below
the control value and inhibits the increase in the ratio
during ischemia (open triangles). Compared with untreated
hearts (Figure 6), verapamil reduces thefluorescence ratio
at every point in time. An overall significance of p<0.001
was obtained by analysis of variance for repeated measures. p values for each of the 1 1 time points were less than
0.05 by the method of Bonferroni. End-diastolic ratios in
Figure 6 were used for this analysis.
sic action potentials. The increase in the fluoresratio during ischemia is markedly reduced in
cence
1055
untreated hearts (Figure 6, p<0.001), but the reduction is not appreciably greater than that produced
by 0.25 ,uM verapamil. Although the monophasic
action potentials remain normal after 3.0 ,M verapamil, the effects of ischemia, such as reduction of
the resting potential, broadening of the action potential, and alternation of action potential duration are
prevented or greatly delayed.
Elevation of CO2 Simulates Effects of Ischemia on
Calcium Transients
The mechanism by which calcium transients are
elevated during ischemia is uncertain but probably
involves impairment of calcium sequestration. Calcium sequestration can be impaired by acid metabolites such as C02, which accumulates rapidly during ischemia27 and which is known to increase
[Ca2+]i in barnacle muscle fibers28 and in isolated
cardiac fibers.29,30 As shown in Figure 11, infusion
of hypercarbic saline increases the F4m/F550 ratio
during both systole and diastole and causes broadening of the calcium transients similar to that seen
in ischemia. This effect develops within 1 minute
(Figure 1iB) and recovers fully during reperfusion
with saline containing normal CO2. The effects
shown in Figure 11 have been observed in a total of
five hearts for which the pH values of the infused
saline ranged from 6.3 to 6.6. A similar result has
been obtained in three hearts in which lactic acid
(15-20 mM) was added to the saline solution, producing pH values of 6.3, 6.4, and 6.9. The effect of
lactic acid on [Ca2+]i-dependent fluorescence is not
ascribable to the lactate anion because infusion of a
20-mM lactate solution that had been neutralized to
pH 7.30 had no effect on the F4m/F550 fluorescence
ratio in two hearts.
The response to CO2 does not represent a direct
effect of reduced pH on indo 1 fluorescence. This
has been established by in vitro acidification (to pH
Circulation Vol 78, No 4, October 1988
1056
A
CONTROL
2.0
1.4t-
i,
1,j
FIGURE 1 1. Recordings ofchanges in the
calcium transient produced by a 1-minute
CONTROL
infusion of a solution made acidic (pH
6.3) by elevation of CO2. Partial pressure
of C02, Pco2, is 232 mm Hg, whereas Po2
is
150 mm Hg. Elevation of C02 produces
/1/
l,
a marked increase in the peak systolic and
0
2 end-diastolic level of the calcium tran1
sec
sients while broadening the peak and
reducing beat frequency (Panel A, center).
These effects are seen within 15 seconds
(low speed recording in Panel B) and are
reversible upon return to normal conditions (Panel A, right). Broader appearance of the calcium transient in elevated
38
40 CO2 is presumably due to a slower rate of
intracellular calcium sequestration.
pH=6.3
'i
11,'
l
2
1
1
2
sec
sec
B
|pH
20
6.3
=
W4|M.
-1
20
0
30
sec
Downloaded from http://circ.ahajournals.org/ by guest on June 12, 2017
6.0) of three indo 1 solutions for which resulting
fluorescence ratios (F400/F550) are plotted in Figure
12. Acidification has no significant effect on the
F4m/F550 ratio, irrespective of whether the indo 1
solution is saturated with calcium (top plot), free of
calcium (bottom plot), or partially saturated with
calcium (middle plot). The increase in the F4m/F550
ratio during in vivo acidification must therefore be
ascribed to an increase in [Ca2+]i.
Discussion
These experiments show that it is practical to
study qualitatively the effects of ischemia on cytosolic calcium activity with the fluorescent calcium
Effect of pH on lndo-1 Fluorescence
5
50
Ln
Lf)
#
** .p
.i
.
4
UI.
0
0
LL.
3
-
2Um
1
1~~~~~w~
0
5
6
pH
7
8
FIGURE 12. Plot ofeffect of acidification on the F4co/Fs50
ratio of three indo 1 solutions studied in vitro. Top plot
shows data for a calcium-saturated solution, which contains 5 mM CaCI2 and 1 ,uM indo 1. Bottom plot shows
data for a calcium-free solution that contains zero calcium, 1 ,M indo 1, and 1.115 mM ethyleneglycol-bis-(/3aminoethyl ether)-N,N,N',N'-tetraacetic acid. Middle plot
shows data for a partially calcium-saturated solution,
which contains 21 ,uM indo 1 and 10 ,M CaCl2. Changes
of pH between 6.0 and 7.3 have little effect on the
fluorescence ratio (see text).
l
,1
indicator indo 1. This is the first study in which
calcium transients, action potentials, and contractions have been directly correlated in the intact
heart. Indo 1 and the related compound fura-2 have
been used previously in isolated myocytes from
both embryonic and adult hearts.12-14,26,31 Studies
with myocytes show that the acetoxymethylester
form of these indicators can be loaded selectively
into the myofilament space and can give highquality calcium transients at concentrations that do
not produce significant buffering. 3,30 The calcium
transients recorded from the rabbit heart are similar
in time course to those obtained in isolated cells,
and they respond appropriately to interventions
with known effects on [Ca2+]i. Absence of buffering
is confirmed by the normal strength and duration of
contractions in the indo 1-loaded hearts (Figure 2).
A particularly important feature of indo 1 is that
motion artifact can be cancelled by obtaining the
ratio of signals at two emission wavelengths. This
strategy has been used previously in isolated cardiac myocytes.13 Several observations show that
the fluorescence ratio in indo 1-loaded rabbit hearts
is free of motion artifact. First, calcium transients
always precede the onset of contraction (Figure 2)
and have an upstroke velocity that is faster than the
rise in force. Second, the fluorescence transients at
400 and 550 nm are opposite to one another, and are
often monophasic, with no common mode deflection at any point in the cycle (e.g., Figure 1). Hearts
with monophasic transients at 400 and 550 nm
produce no transients at the isosbestic wavelength
of indo 1.11-13 In other hearts, motion does produce
a common mode deflection in the 400- and 550-nm
signals, but these deflections cancel in the ratio,
leaving monophasic calcium transients comparable
to those in Figure 1.
The major limitation of the indo 1 method, as
presently used, is the absence of a satisfactory
calibration procedure. Calibration is known to be
hindered by incomplete deesterification of the indo
1-AM,'7 which clearly occurs based on the results
Lee et al Ischemia and Calcium-Dependent Fluorescence Transients
of the manganese quenching studies. Changes in
autofluorescence may also complicate the calibration of indo 1 recordings, although these effects are
largely cancelled in the ratio, and can be corrected
more precisely by subtracting the autofluorescence
Downloaded from http://circ.ahajournals.org/ by guest on June 12, 2017
at each wavelength.
Once it is possible to record calcium transients in
the intact heart, it is then possible to study the effects
of ischemia. Ischemia produces striking abnormalities in the calcium transient that appear 5-10 seconds
after cessation of flow. These abnormalities include
1) marked elevation of the systolic peak, 2) marked
elevation of the end-diastolic level, 3) broadening of
the systolic peak, and 4) an increase in the net
amplitude of the transients. All of these changes can
be observed in the individual fluorescence signals
(Figure 5) as well as in the F4m/F550 ratio.
The above observations indicate that fluctuations
in cytosolic calcium become larger during the first
90 seconds of ischemia in the rapidly paced rabbit
heart. We presume that the calcium-dependent fluorescence ratio, F400/F550, is a monotonic function of
cytoplasmic free calcium, [Ca2+]i. Granted that this
is so, our recordings show not only an increase in
the peak [Ca21]i that is achieved during systole but
also an increase in the end-diastolic level from
which the transients arise. Changes in end-diastolic
[Ca2 ]i are a common finding with tetracarboxylate
indicators, owing to the fact that at physiological
heart rates each transient arises before the preceding transient has fully decayed. End-diastolic [Ca2+i,
is strikingly dependent upon the interbeat interval
and can be altered by pharmacological agents that
either accelerate or impair the uptake of calcium by
the sarcoplasmic reticulum.32 It is, of course, possible that the fluorescence ratio is affected by some
other factor, such as accumulation of calcium within
a noncytosolic compartment that contains indo 1.
However, our cell fractionation studies (see "Materials and Methods") show that most of the calciumsensitive indo 1 fluorescence is in the soluble fraction and that very little calcium-sensitive fluorescence
is associated with the mitochondria, which would be
the most likely compartment to accumulate calcium
under conditions of metabolic stress.
In addition to the overall elevation of [Ca2+]i,
ischemia produces striking nonuniformities in the
calcium transient, which are associated with similar
nonuniformities in electrical and mechanical activities. The above abnormalities may explain various
physiological correlates of ischemia, such as the
dispersion of electrical refractoriness that leads to
arrhythmias in the first few minutes of ischemia.
Mechanism of Ischemia-Induced [Ca2+L Increase
The role of abnormal calcium handling in cardiac
ischemia has been discussed for many years and is
especially well documented in models where protracted ischemia is followed by reperfusion.33,34
Whether or not [Ca2+I increases during brief ischemic trials is less certain for two reasons. First, the
1057
rapid decline in contractile force during the first 2
minutes of ischemia might be regarded as evidence
against a [Ca2+], increase. It is now clear that the
sensitivity of the myofilaments to calcium is depressed during ischemia and that contractions may
therefore cease, even in the face of a brisk [Ca2']i
increase (Figure 2). Second, studies with aequorinloaded cardiac fibers have shown that extended
periods of hypoxia or metabolic inhibition20 often
fail to increase [Ca2+]i. Possible reasons for this
discrepancy include 1) failure of isolated preparations to simulate conditions in the intact heart (e.g.,
inability of isolated fibers to sustain physiological
work loads and stimulus rates), 2) failure of energy
deprivation to reproduce the conditions of ischemia, and 3) differences in the behavior of various
calcium indicators.
An important feature of ischemia, which is not
duplicated by hypoxia or metabolic inhibition, is
accumulation of acid metabolites, such as CO2.
Acidification35 and CO2 accumulation27 both occur
within seconds of coronary occlusion. Myocardial
acidification is accelerated by pacing and diminished by verapamil.35 Maneuvers that modulate
acidification may have parallel effects on [Ca21]i.
Acidification of isolated cardiac fibers increases
the peak amplitude of [Ca21]i transients recorded
with aequorin (Orchard30; Figure 1). A corresponding increase in diastolic [Ca2]ij has not been resolved
with aequorin but can be observed in quiescent
fibers with ion-selective electrodes. Bers and Ellis29
find that cytoplasmic acidification can elevate resting [Ca21]i to 2 ,M, which is greater than the level
that is normally achieved during the peak of the
[Ca2+]i transient. This observation corroborates our
finding that infusion of CO2 into isolated hearts can
elevate end-diastolic [Ca2+]i to the normal systolic
level (Figure 11).
Our experiments with indo 1 partly confirm results
obtained with the calcium-sensitive nuclear magnetic
resonance probe 5,5'-difluorobis(o-aminophenoxy)
ethane-N,N,N',N'-tetraacetic acid (5F-BAPTA).36,37
In these studies, ischemia produces a threefold
increase in time averaged [Ca2+II, after 20 minutes,
but no increase is observed during the first 5 minutes. A possible reason for this discrepancy is the
greater buffering that 5F-BAPTA produces, which
inhibits contraction at physiological concentrations
of extracellular calcium.
Correlation of [Ca2+i With Electrophysiological
Derangements
A principal reason why abnormalities in [Ca2+]i
could be important during ischemia lies in the
ability of cytosolic calcium to regulate membrane
potential. Increased [Ca2+]i can depolarize cardiac
cells by means of a calcium-activated inward current. Such current can flow either through sodiumcalcium exchange7 or through calcium-activated
cation channels5 that have been described in cardiac
cells. Activation of these currents by a sustained
1058
Circulation Vol 78, No 4, October 1988
Downloaded from http://circ.ahajournals.org/ by guest on June 12, 2017
rise in [Ca2"]i could contribute to the reduction in
resting potential that occurs during ischemia.
A major arrhythmogenic effect of ischemia is
dispersion of the ventricular refractory period, which
allows premature beats to initiate ventricular
fibrillation.2 Recordings obtained in ischemic dog
hearts show that the onset of ventricular fibrillation
is preceded by the appearance of an alternans
pattern in the T wave of the epicardial electrogram.38
Recordings obtained with suction electrodes in the
ischemic pig heart reveal beat-to-beat alternations
of action potential duration, which do not occur in
simultaneous recordings obtained from the border
zone or normal myocardium.24 We have observed
similar alternation of action potential duration in the
globally ischemic rabbit heart (Figure 9) and have
shown that there are associated variations in the
amplitude of the intracellular calcium transient.
These variations in the calcium transient are not
caused by conduction block, or impaired excitability, because the time course of the action potential
does not vary during the first 80 msec, when the
calcium transient rises to its peak (Figure 9B).
Variations in the calcium transient can occur independently in localized regions of the heart. This can
be shown by rapid relocation of the fiber-optic
probe, which can reverse the parity of the alternans
during continuous recordings. Because membrane
currents initiated by the calcium transient are known
to have important effects on the action potential
plateau,6 10 it seems quite possible that primary
abnormalities of cytosolic calcium might be responsible for the nonuniformities of repolarization that
occur in the ischemic heart.
An important implication of our findings is that
the ability of various drugs to limit the electrophysiological consequences of ischemia may reflect prevention of concurrent abnormalities of [Ca21]i. In
our experiments, concentrations of verapamil that
inhibit the effects of ischemia on the calcium transient also prevent the abnormalities of the monophasic action potential that are illustrated in Figures
8 and 9. Both verapamil and diltiazem retard the
occurrence of ventricular fibrillation in vivo39,40 and
prevent the decline in the threshold for production
of fibrillation by application of pulse trains during
the T wave.41 The latter finding suggests that the
uniformity of the ventricular refractory period is
somehow preserved. Our experiments show that
preservation of normal [Ca2+]i levels could be the
basis for these beneficial actions.
Acknowledgments
We thank Robert Marshall Jr. and Prof. U.J.
McMahan of the Stanford Neurobiology Department for their assistance in performing electron
microscopy and Dr. Bruce Hill of the Palo Alto
Medical Foundation for guidance in the design of
optical apparatus. We are also indebted to Cecil
Profitt, Robert Kernoff, and George Snidow for
assistance with the experiments.
References
1. Kleber AG: Resting membrane potential, extracellular potassium activity and intracellular sodium activity during acute
global ischemia in isolated perfused guinea pig hearts. Circ
Res 1983;52:442-450
2. Han J, Garcia-DeJalon PD, Moe GK: Adrenergic effects on
ventricular vulnerability. Circ Res 1964;14:516-524
3. Clusin WT, Buchbinder M, Harrison DC: Calcium overload,
"injury" current, and early ischaemic cardiac arrhythmiasa direct connection. Lancet 1983;1:272-274
4. Kass RS, Lederer WJ, Tsien RW, Weingart R: Role of
calcium ions in transient inward currents and aftercontractions induced by strophanthidin in cardiac Purkinje fibers. J
Physiol (Lond) 1978;281:187-208
5. Colquhoun D, Neher E, Reuter H, Stevens CF: Inward
current channels activated by intracellular Ca+ + in cultured
cardiac cells. Nature 1981;294:752-754
6. Karagueuzian HS, Katzung BG: Voltage-clamp studies of
transient inward current and mechanical oscillations induced
by ouabain in ferret papillary muscle. J Physiol (Lond) 1982;
327:255-271
7. Mullins LJ: The generation of electric currents in cardiac
fibers by Na/Ca exchange. Am J Physiol 1979;237:C 103-C1 10
8. Kenyon JL, Sutko JL: Calcium- and voltage-activated plateau currents of cardiac Purkinje fibers. J Gen Physiol 1987;
89:921-958
9. Clusin WT: Caffeine induces a transient inward current in
cultured cardiac cells. Nature 1983;301:248-250
10. Mitchell MR, Powell T, Terrar DA, Twist VW: The effects
of ryanodine, EGTA and low sodium on action potentials in
rat and guinea pig ventricular myocytes: Evidence for two
inward currents during the plateau. Br J Pharmacol 1984;
81:551
11. Grynkiewicz G, Poenie M, Tsien RY: A new generation of
Ca2t indicators with greatly improved fluorescence proper-
ties. J Biol Chem 1985;260:3440-3450
12. Lee H, Clusin WT: Cytosolic calcium staircase in cultured
myocardial cells. Circ Res 1987;61:934-939
13. Peeters GA, Hlady V, Bridge JHB, Barry WH: Simultaneous measurement of calcium transients and motion in
cultured heart cells. Am J Physiol 1987;253:H1400-H1408
14. duBell WH, Houser SR: Calcium transients and cell shortening in indo-1 loaded isolated feline ventricular myocytes.
Biophys J 1987;51: 1 1Oa
15. Franz MR: Long-term recordings of monophasic action
potentials from human endocardium. Am J Cardiol 1983:
51:1629-1634
16. Franz MR, BurkhoffD, Spurgeon H, Weisfeldt ML, Lakatta
EG: In vitro validation of a new cardiac catheter technique
for recording monophasic action potentials. Eur Heart J
1986;7:34-41
17. Luckhoff A: Measuring cytosolic free calcium concentration
in endothelial cells with indo-l: The pitfall of using the ratio
18.
19.
20.
21.
22.
of two fluorescence intensities recorded at different wavelengths. Cell Calcium 1986;7:233-248
Allfrey V: The isolation of subcellular components, in J
Brachet and AE Mirsky (eds): The Cell. New York/London,
Academic Press, 1959, pp 193-290
Steinberg SF, Bilezikian JP, Al-Awqati Q: Fura-2 fluorescence is localized to mitochondria in endothelial cells. Am J
Physiol 1987;253:C744-747
Allen DG, Orchard CH: The effect of hypoxia and metabolic
inhibition on intracellular calcium in heart muscle. J Physiol
(Lond) 1983;339:102-122
Kusuoka H, Weisfeldt ML, Zweier JL, Jacobus WE, Marban E: Mechanism of early contractile failure during hypoxia
in intact ferret heart: Evidence for modulation of maximal
Ca' -activated force by inorganic phosphate. Circ Res
1986;59:270-282
Clusin WT: Mechanism by which metabolic inhibitors depolarize cultured cardiac cells. Proc Natl Acad Sci USA 1983;
80:3865-3869
Lee et al Ischemia and Calcium-Dependent Fluorescence Transients
Downloaded from http://circ.ahajournals.org/ by guest on June 12, 2017
23. Russell DC, Smith HJ, Oliver MF: Transmembrane potential
changes and ventricular fibrillation during repetitive myocardial ischemia in the dog. Br Heart J 1979;42:88-96
24. Dilly SG, Lab MJ: Changes in monophasic action potential
duration during the first hour of regional myocardial ischaemia in the anaesthetized pig. Cardiovasc Res 1987;21:908-915
25. Horackova M: Excitation-contraction coupling in isolated
adult ventricular myocytes from the rat, dog, and rabbit:
Effects of various inotropic interventions in the presence of
ryanodine. Can J Physiol Pharmacol 1986;64: 1473-1483
26. Barcenas-Ruiz L, Wier WG: Voltage dependence of intracellular [Cat t']j transients in guinea pig ventricular myocytes.
Circ Res 1987;61:148-154
27. Case RB, Felix A, Castellana FS: Rate of rise of myocardial
pCO2 during early myocardial ischemia in the dog. Circ Res
1979;45:324-330
28. Lea TJ, Ashley CC: Increase in free Ca'+ in muscle after
exposure to CO2. Nature 1978;275:236-238
29. Bers DM, Ellis D: Intracellular calcium and sodium activity
in sheep heart Purkinje fibers: Effects of changes of external
sodium and intracellular pH. PflugersArchiv 1982;393:171-178
30. Orchard CH: The role of the sarcoplasmic reticulum in the
response of ferret and rat heart muscle to acidosis. J Physiol
(Lond) 1987;384:431-449
31. Berlin JR, Cannell MB, Lederer WJ: The dependence of the
calcium transient on depolarization duration in voltageclamped single heart cells. Biophys J 1987;51:197a
32. Lee H, Smith N, Mohabir R, Clusin WT: Cytosolic calcium
transients from the beating mammalian heart. Proc Natl
Acad Sci USA 1987;84:7793-7797
33. Sharma AD, Saffitz JE, Lee BI, Sobel BE, Corr PB: Alpha
adrenergic-mediated accumulation of calcium in reperfused
myocardium. J Clin Invest 1983;72:802-818
1059
34. Coetzee WA, Opie LH: Effects of components of ischemia
and metabolic inhibition on delayed afterdepolarizations in
guinea pig papillary muscle. Circ Res 1987;61:157-165
35. Couper GS, Weiss J, Hiltbrand B, Shine KI: Extracellular
pH and tension during ischemia in the isolated rabbit ventricle. Am J Physiol 1984;247:H916-H927
36. Steenbergen C, Murphy E, Levy L, London RE: Elevation
in cytosolic free calcium concentration early in myocardial
ischemia in perfused rat heart. Circ Res 1987;60:700-707
37. Marban E, Kitakaze M, Kusuoka H, Porterfield JK, Yue
DT, Chacko VP: Intracellular free calcium concentration
measured with '9F NMR spectroscopy in intact ferret hearts.
Proc Natl Acad Sci USA 1987;84:6005-6009
38. Kleber AG, Janse MJ, van Capelle FJL, Durrer D: Mechanism and time course of S-T and T-Q segment changes
during acute regional myocardial ischemia in the pig heart
determined by intracellular and extracellular recordings.
Circ Res 1978;42:603-613
39. Kaumann AJ, Aramendia P: Prevention of ventricular fibrillation induced by coronary ligation. J Pharmacol Exp Ther
1968;164:326-332
40. Clusin WT, Bristow MR, Baim DS, Schroeder JS, Jaillon P,
Brett P, Harrison DC: The effects of diltiazem and reduced
serum ionized calcium on ischemic ventricular fibrillation in
the dog. Circ Res 1982;50:518-526
41. Fondacaro JD, Han J, Yoon MS: Effects of verapamil on
ventricular rhythm during acute coronary occlusion. Am
Heart J 1978;96:81-86
KEY WORDS * calcium transients * indo 1 * cardiac ischemia
* mechanical alternans * calcium alternans
Effect of ischemia on calcium-dependent fluorescence transients in rabbit hearts
containing indo 1. Correlation with monophasic action potentials and contraction.
H C Lee, R Mohabir, N Smith, M R Franz and W T Clusin
Downloaded from http://circ.ahajournals.org/ by guest on June 12, 2017
Circulation. 1988;78:1047-1059
doi: 10.1161/01.CIR.78.4.1047
Circulation is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 1988 American Heart Association, Inc. All rights reserved.
Print ISSN: 0009-7322. Online ISSN: 1524-4539
The online version of this article, along with updated information and services, is located on
the World Wide Web at:
http://circ.ahajournals.org/content/78/4/1047
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally
published in Circulation can be obtained via RightsLink, a service of the Copyright Clearance Center, not the
Editorial Office. Once the online version of the published article for which permission is being requested is
located, click Request Permissions in the middle column of the Web page under Services. Further
information about this process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Circulation is online at:
http://circ.ahajournals.org//subscriptions/