* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Second degree heart block
Management of acute coronary syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Coronary artery disease wikipedia , lookup
Myocardial infarction wikipedia , lookup
Jatene procedure wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
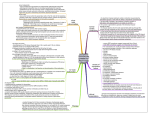
Electrocardiography wikipedia , lookup
ATRIOVENTRICULAR AND BUNDLE BRANCH BLOCK ATRIOVENTRICULAR (AV) BLOCK Atrioventricular conduction is influenced by autonomic activity. AV block can therefore be intermittent and may only be evident when the conducting tissue is stressed by a rapid atrial rate. Accordingly, atrial tachyarrhythmias are often associated with AV block . First degree heart block In this condition AV conduction is delayed so the PR interval is prolonged ( > 0.20 s) it rarely causes symptoms. Second degree heart block B(Intermittent Atrioventricular Conduction) In this condition dropped beats occur because some impulses from the atria fail to conduct to the ventricles . In Mobitz type 1 there is progressive lengthening of successive PR intervals culminating in a dropped beat. The cycle then repeats itself . this is known as Wenchebach 's phenomenon and is usually due to impaired conduction in the AV node itself .it may be physiological and sometimes observed at rest or during the sleep in athletic young adult with high vagal tone . In Mobitz type 2 the PR interval of the conducted impulses remains constant but some P waves are not conducted .this usually caused by diseases of the His-Purkinje system and carries a risk of a systole . In 2:1AV block alternate P waves are conducted , so it is impossible to distinguish between Mobitz type 1 and Mobitz type 2. Third degree (complete ) heart block When AV conduction fails completely , the atria and ventricles beat independently ( AV dissociation ) Ventricular activity is maintained by an escape rhythm arising in the AV node or bundle of His ( narrow QRS complexes) or the distal Purkinje tissues ( broad QRS complexes ) . Complete heart block produces a slow (25-50/min), regular pulse that, except in the case of congenital complete heart block, does not vary with exercise. There is usually a compensatory increase in stroke volume with a large volume pulse and systolic flow murmurs. Cannon waves may be visible in the neck and the intensity of the first heart sound varies due to the loss of AV synchrony. AETIOLOGY OF COMPLETE HEART BLOCK Congenital Acquired Idiopathic fibrosis Myocardial infarction/ischaemia Inflammation o Acute (e.g. aortic root abscess in infective endocarditis) o Chronic (e.g. sarcoidosis, Chagus disease). .Trauma ( cardiac surgery) .Drugs ( digoxin , b- blockers ) Stokes-Adams attacks Episodes of ventricular asystole may complicate complete heart block or Mobitz type 2 second degree heart block or occur in patient with sinoatrial disease .this may cause recurrent syncope or Stokes-Adams attacks. Typical episode is characterized by sudden loss of consciousness that occurs without warning and results in collapse . A brief anoxic seizure ( due to cerebral ischemia ) may occur if there is prolonged asystole. There is pallor and death like appearance during the attack, but when the heart starts beating again there is a characteristic flush . Unlike epilepsy , recovery is rapid .Sinoatrial disease and neurocardiogenic syncope may cause similar symptoms. Management AV block complicating acute MI Acute inferior MI is often complicated by transient AV block because the RCA supplies AV node . there is usually a reliable escape rhythm and if the patient remains well no treatment is required . symptomatic second and third degree heart block may respond to atropine (0.6mg to 3 mg ) or if this fail a temporary pacemaker . In most cases the AV block will resolve within 7-10 days . second and third degree heart block may complicate acute anterior MI indicates extensive ventricular damage involving both bundle branches and carries a poor prognosis . Asystole may ensue and temporary pacemaker should be inserted promptly . If the patient presents with asystole i.v atropine or iv isoprenaline 2mg in 500 ml 5% dextrose infused at 10-60 ml/hr may help to maintain the circulation until temporary pacemaker inserted . External (transcutaneous) pacing can provide effective temporary rhythm support . Chronic AV block Patient with symptomatic bradyarrhythmias associated with AV block should receive a permanent pacemaker . asymptomatic first degree or Mobitz type 1 second degree heart block does not require treatment but may be an indication of serious underlying heart disease . permanent pacemaker is usually indicated in a patient with asymptomatic Mobitz type 2 second or third degree heart block because of the risk of asystole and sudden death. Pacing improve the prognosis . Bundle branch block With complete bundle branch blocks, the QRS interval is 0.12 s in duration; with incomplete blocks the QRS interval is between 0.10 and 0.12 s. Conduction block of left bundles can ocurr as a result of many pathologies , including ischemia , hypertensive heart disease or cardiomyopathy or aortic valves disease while conduction block in the right could be normal or from ASD or ischemia . Depolarization proceeds the slow myocardial route in the affected ventricle rather than through the rapidly conducting Purkinje tissues that constitute the bundle branches .this causes delayed conduction into LV or RV , broadens the QRS complex(>0.12 s) and produce the characteristic alterations in QRS morphology with RBBB, the terminal QRS vector is oriented to the right and anteriorly (rSR' in V1 and qRS in V6, typically). Left bundle branch block alters both early and later phases of ventricular depolarization . Right bundle branch block can occur in healthy people but the left bundle branch block often signifies important underlying heart disease . The left branch of the bundle of His divides into an anterior and a posterior fascicle. Damage to the conducting tissue at this point (hemiblock) does not broaden the QRS complex, but alters the mean direction of ventricular depolarisation (mean QRS axis), causing left axis deviation in left anterior hemiblock and right axis deviation in left posterior hemiblock. The combination of right bundle branch and left anterior or posterior hemiblock is known as bifascicular block. left anterior hemiblock 1 SINOATRIAL DISEASE (SICK SINUS SYNDROME) Sinoatrial disease can occur at any age, but is most common in the elderly. The underlying pathology is not understood but may involve fibrosis, degenerative changes and/or ischaemia of the sinoatrial (sinus) node. The condition is characterised by a variety of arrhythmias (Box below) and may present with palpitation, dizzy spells or syncope, due to intermittent tachycardia, bradycardia, or pauses with no atrial or ventricular activity (sinoatrial block or sinus arrest). A permanent pacemaker may benefit patients with troublesome symptoms due to spontaneous bradycardias, or those with symptomatic bradycardias induced by drugs required to prevent tachyarrhythmias. Atrial pacing may help to prevent episodes of atrial fibrillation. Permanent pacing does not improve prognosis and is not indicated in patients who are asymptomatic. COMMON FEATURES OF SINOATRIAL DISEASE Sinus bradycardia Sinoatrial block (sinus arrest) Paroxysmal supraventricular tachycardia Paroxysmal atrial fibrillation Atrioventricular block . Sinus Bradycardia Rates less than 60 beats per minute are usually described as bradycardia. In healthy persons, rates of 50 beats per minute are not unusual, however, and rates of 30 beats per minute may be recorded during sleep. Sinus bradycardia of clinical significance is usually defined as persistent rates less than 45 beats per minute while awake. sinus bradycardia can occur in athletes , hypothyroidism , ischemia , obstructive joundice or secondary to cardioactive drugs such as β-blockers or calcium-channel blockers. treatment • • • • • • Correction of the underlying cause Asymptomatic : only follow up Symptomatic : either : Medical : 1- atropine and isoprenaline in the emergency states 2- B2 agonists or thiophylline may be benificial 3- Pacemakers Sinus Arrest Sudden disappearance of P waves could be due to either SA exit block or cessation of sinus node pacemaker function. Treated By pacemaker Bradycardia-Tachycardia Syndrome Because SND often represents atrial disease processes (e.g., fibrosis, degeneration, inflammation), coexistence of atrial tachyarrhythmias with bradycardia is not surprising. When an atrial tachycardia such as AF is terminated, the underlying rhythm may reveal sinus bradycardia, SA exit block, or even complete atrial standstill with an escape rhythm from a lower pacemaker in the AV junction or the HPS. Treated by permanent pacemaker