* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Bradyarrhythmia Pacing Devices
Heart failure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Myocardial infarction wikipedia , lookup
Cardiac surgery wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Atrial fibrillation wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
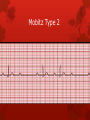
Bradyarrhythmia’s, Pacemaker’s & Complex Devices Dr Chris McAloon Medical Student Teaching Overview Interpreting Bradyarrhythmia’s Different types of Bradyarrhythmia’s Pacemakers Complex Devices First Rule “ Always look at the patient” Conducting system Heart Blocks NSR Sinus brady SSS Sinoatrial block Sinus arrest 7 Heart Blocks 1st degree 2nd degree Mobitz Type 1 Mobitz Type 2 2:1, 3:1 AVB 3rd degree Fascicular block - LAD, RAD, TFB LBBB, RBBB AF, Flutter 8 Reversible Causes of Slow Heart Rate Drug therapy Acute Myocardial Infarction Hypothermia Hypothyroidism Athletic Heart Vaso-vagal mechanisms Complete AV Block All patients with persistent or intermittent complete AV block should be paced unless there is a reversible cause Irrespective of symptoms Reversible causes include recent inferior MI, hypothyroidism and drugs This includes patients with congenital CHB If you are not going to pace, you really need to be able to justify that decision Sinus Node Dysfunction Inappropriate bradycardia Intermittent – faintness / syncope Persistent – SOB / muscle fatigue / exhaustion Associated atrial tachyarrhythmias / AV Block Intermittent – palpitations / faintness / syncope Persistent – SOB / muscle fatigue / exhaustion Associated clinical syndromes Embolic Heart Failure The ‘ALS’ Approach 1. Is there electrical activity? 2. What is the ventricular (QRS) rate? 3. Is the QRS rhythm regular or irregular? 4. Is the QRS complex width normal or prolonged? 5. Is there atrial activity present? 6. Is the atrial activity related to ventricular activity, if so how? The Heart Block System 1. Are the P waves associated with the QRS complex at all? No = This is 3rd Degree Heart Block Yes= Move to Question 2 Third Degree/ Complete Heart Block The Heart Block System 2. Is there one P wave to one QRS, with a prolonged PR interval that is not progressing (in length)? Yes= This is 1st Degree Heart block No = Go to question 3 First Degree Heart Block The Heart Block System 3. Is there progression in PR interval duration until there is a non-conducted P wave? Yes= This is Wenckebach No = Go to question 4 Mobitz Type 1/ Wenckebach The Heart Block System 4. Therefore it must be Mobitz type 2 Mobitz type 2 difficult to explain P waves conducted normal PR interval There are P waves that are not conducted Not always a specific block 2:1 3:1 4:3 Mobitz Type 2 Mobitz 2 – 3:1 Block SA Slow Sinus Rate Atrial Tachy-arrhythmias AV Block Pacemaker’s Pacing Indications Paced Patients: Predominant ECG Indication CHB AF SSS Other percentage of total 100% 80% 60% 40% 20% 0% 0-9 10-19 20-29 30-39 40-49 50-59 60-69 70-79 80-89 90-99 100+ age by decade BPEG / HRUK National Database 2003 - 4 Paced Patients: Predominant Presenting Symptom syncope pre syncope other percentage of total 100% 80% 60% 40% 20% 0% 0-9 10-19 20-29 30-39 40-49 50-59 60-69 70-79 80-89 90-99 100+ decade BPEG / HRUK National Database 2003-4 Pacing Indications AV Block Complete Heart Block Second degree AV block (High block or symptoms) Reversible: Inferior MI, Hypothyroidism Sinus Node Disease Chronotropic Incompetence If resting HR in day time <30 Atrial Fibrillation Bradycardia Bradycardia in presence drugs for uncontrolled Tachycardia International Codes Pacemaker First Letter = Chamber(s) being PACED (A,V,D) Second Letter = Chamber(s) being SENSED Third Letter= How the device RESPONDS to SENSED Event (Inhibits, Triggers, Dual (I+T)) Fourth Letter = Added feature e.g R = Rate Response Pacemaker Basic’s A Unipolar System A Bipolar System What is the PPM? What is the PPM? What is the PPM? What is the PPM? Electrodes -- Fixation Mechanism Passive Fixation Mechanism – Endocardial Tined Finned Canted/curved Electrodes – Fixation Mechanism Active Fixation Mechanism – Endocardial Fixed screw Extendible/retractable Pacemaker Prescription Re-establish stable heart rate Restore AV synchrony Achieve chronotropic competence Achieve normal physiological activation and timing A lead if normal A function V lead if actual / threatened AV HB Rate modulation if slow 1% A Lead only 55% A + V Leads (Dual Chamber) 44% V Lead only (mostly in AF) A V V lead normally @ RV apex Complex Devices Complex Devices What can be done? What can be done? Technology Heart Failure and CRT Heart failure common and disabling condition Cardiac resynchronization therapy (CRT) NICE indications Applicable to ~1/3 of all symptomatic HF patients Improvement in long term survival NYHA III/IV, Optimal medical therapy LVEF <35% QRS > 120ms However, 20-30% non responders to CRT CARE-HF: CRT vs Medical Therapy - Primary End Point Cleland, J. et al. N Engl J Med 2005;352:1539-1549 NICE Guidance 95 & 120 Global Heroes 2012: 10 mile run Susan Filler was an avid runner 2007 survived Cardiac Arrest ARVD diagnosed & ICD implanted Completed Boise & Canada Ironman Patrick Grayson 21 Long QT diagnosed at 11 At 12 Cardiac Arrest & ICD implanted Protection of ICD gave confidence to run February 2012 ran 1st marathon Erin Clark 20 years ago SCA, diagnosed Long QT BB 1st, then implanted ICD. ICD gave confidence to be active as protection 1 year ago started running What patients say about ICD When I die will this keep shocking me? In my coffin? One day I want to join my wife – how can I do that with an ICD? Can I be comfortable at the end of my life? Will Deactivation hurt? Do I need surgery? Will I die immediately after the ICD is deactivated? I feel like the bionic man – can I die with this? ESC GUIDANCE 2010 ‘It seems clear at this point that this device is in your best interest, but you should know at some point if you become very ill from your heart disease or another process you developing the future, the burden of this device may outweigh its benefit. While that point is hopefully a long way off, you should know that turning off your defibrillator is an option.’ ‘Now that we’ve established that you would not want resuscitation in the event your heart was to go into an abnormal pattern of beating, we should reconsider the role of yourdevice. In many ways it is also a form of resuscitation. Tell me your understanding of the device and let’s talk about how it fits into the larger goals for your medical care at this point.’ ‘Clinicians may be concerned that withdrawing life-sustaining treatments such as CIED (ICD) therapies amounts to assisted suicide or euthanasia. However, two factors differentiate withdrawal of an unwanted therapy from assisted suicide and euthanasia: the intent of the clinician, and the cause of death. First, in withdrawing an unwanted therapy, the clinician’s intent is not to hasten the patient’s death, but rather, to remove a treatment that is perceived by the patient as a burden.’