* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Chapter 12 The Cardiovascular System: The Heart Pages 388
Survey
Document related concepts
Heart failure wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Electrocardiography wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Coronary artery disease wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Artificial heart valve wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Myocardial infarction wikipedia , lookup
Cardiac surgery wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Transcript
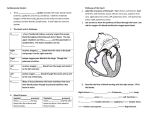
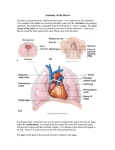
CHAPTER 12 THE CARDIOVASCULAR SYSTEM: THE HEART PAGES 388 - 411 LOCATION & GENERAL FEATURES OF THE HEART TWO CIRCUIT CIRCULATORY SYSTEM DIVISIONS OF THE HEART FOUR CHAMBERS Right Atrium Receives blood from the systemic circuit Left Atrium Receives blood from the pulmonary circuit FOUR CHAMBERS Right Ventricle Ejects blood into the pulmonary circuit Left Ventricle Ejects blood into the systemic circuit FOUR VALVES – ATRIOVENTRICULAR VALVES Right Atrioventricular Valve (AV) Tricuspid Valve Left Atrioventricular Valve (AV) Bicuspid Valve and Mitral Valve FOUR VALVES – SEMILUNAR VALVES Pulmonary valve Guards entrance to the pulmonary trunk Aortic Valve Guards entrance to the aorta FLOW OF BLOOD MAJOR VEINS AND ARTERIES AROUND THE HEART • Arteries carry blood AWAY from the heart • Veins allow blood to VISIT the heart MAJOR VEINS AND ARTERIES ON THE HEART Coronary Circulation – Supplies blood to the muscle tissue of the heart ARTERIES Elastic artery: Large, resilient vessels. Muscular artery: Medium-sized arteries. They distribute blood to skeletal muscles and internal organs. pulmonary trunk and aorta external carotid artery of the neck Arteriole: Smallest of arteries. Lead into capillaries VEINS Large veins: Largest of the veins. Medium-sized veins: Medium sized veins. Superior and Inferior Vena Cava Pulmonary veins Venules: the smallest type of vein. Lead into cappilaries CAPILLARIES Exchange of molecules between blood and interstitial fluid. FLOW OF BLOOD THROUGH HEART TISSUES OF THE HEART THE HEART WALL Pericardium Outermost layer Serous membrane Myocardium Middle layer Thick muscle layer Endocardium Inner lining of pumping chambers Continuous with endothelium CARDIAC MUSCLE Depend on oxygen to obtain energy Abundant in mitochondria In contact with several other cardiac muscles Intercalated disks – interlocking membranes of adjacent cells Desmosomes Gap junctions CONNECTIVE TISSUE Wrap around each cardiac muscle cell and tie together adjacent cells. Provide support for cardiac muscle fibers Add strength and prevent overexpansion of the heart Help the heart return to normal shape after contractions CHORDAE TENDINEAE Cord-like tendons that connect the papillary muscles to the tricuspid valve and mitral valve Connected to Papillary Muscle. Cone shaped projections on the inner surface of the ventricle Contraction of papillary muscles tenses the chordae tendineae and prevents the backflow of blood into the right and left atrium. WHY DO YOU THINK THE LEFT VENTRICLE HAS THE LARGEST AMOUNT OF MUSCLE?? ELECTRICAL ACTIVITY OF THE HEART THE HEARTBEAT The entire heart – atria and ventricles – contracts in a coordinated manner so that blood flows in the correct direction at the proper time. Two Types of Cardiac Muscle Cells Involved Contractile cells – contractions that propel blood Specialized noncontractile muscle cells – control and coordinate the activities of the contractile cells in the heart Part of the conducting system THE CONDUCTING SYSTEM A network of specialized cardiac muscle cells that initiates and distributes electrical impulses. Nodal Cells Located at the sinoatrial and atrioventricular nodes Responsible for establishing the rate of cardiac contraction. Coupled to one another causing a coordinated contraction when an action potential is initiated. Conducting Cells Include the Atrioventricular Bundle, bundle branches, and purkinje fibers Responsible for distributing the contraction THE CONDUCTING SYSTEM CONT. Pacemaker Cells – Depolarize rapidly, generating 70 – 80 action potentials per minute (bpm) Located in the sinoatrial node Atriventricular (AV) Bundle – (the bundle of His) extend along the interventricular septum before dividing into left and right ventricles Purkinje Fibers – Convey the impulses to the contractile cells of the ventricle muscles. THE ELECTROCARDIOGRAM A machine that records the electrical events occurring in the heart. Each time the heart beats a wave of depolarization radiates through the atria, reaches the AV node, travels down the interventricular septum to the apex, turns, and spreads though the ventricular muscles towards the base of the heart. THE CARDIAC CYCLE THE CARDIAC CYCLE The peiod between the start of one heartbeat and the start of the next is a single cardiac cycle. Includes a period of contraction - systole The chambers contract squeezing blood into an adjacent chamber or arterial trunk Includes a period of relaxation – diastole When the chambers fill with blood and prepares for the start of the next cardiac cycle. HEART DYNAMICS Refers to movements and forces generated during cardiac contractions. Stroke volume - is the amount ejected by a ventricle during a single beat Each time the heart beats, two ventricles eject equal amounts of blood Stroke volume varies beat to beat so physicians are often more interested in cardiac output Cardiac output - is the amount of blood pumped by each ventricle in 1 minute Provides indication of blood flow through peripheral tissues; without adequate blood flow, homeostasis cannot be maintained FACTORS CONTROLLING CARDIAC OUTPUT The major factors that regulate cardiac output often affect both heart rate and stroke volume Primary factors include: Blood volume reflexes Autonomic innervation hormones