* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Long-term in vitro study of paclitaxel
Survey
Document related concepts
Psychopharmacology wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Neuropharmacology wikipedia , lookup
Prescription costs wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Pharmacognosy wikipedia , lookup
Theralizumab wikipedia , lookup
Plateau principle wikipedia , lookup
Discovery and development of tubulin inhibitors wikipedia , lookup
Drug design wikipedia , lookup
Drug interaction wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Nicholas A. Peppas wikipedia , lookup
Drug discovery wikipedia , lookup
Transcript
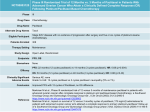
Available online at www.sciencedirect.com Journal of Controlled Release 126 (2008) 139 – 148 www.elsevier.com/locate/jconrel Long-term in vitro study of paclitaxel-eluting bioresorbable core/shell fiber structures Amir Kraitzer, Lia Ofek, Reut Schreiber, Meital Zilberman ⁎ Department of Biomedical Engineering, Faculty of Engineering, Tel-Aviv University, Tel-Aviv 69978, Israel Received 10 October 2007; accepted 16 November 2007 Available online 28 November 2007 Abstract Paclitaxel-eluting bioresorbable core/shell fiber structures for stent applications and local cancer treatment were developed and studied. These structures were composed of a polyglyconate core and a porous PDLGA shell loaded with the anti-proliferative agent paclitaxel, prepared using freeze drying of inverted emulsions. The investigation of these new composite fibers focused on the effects of the emulsion's composition (formulation) and process kinetics on the long-term drug release from the fibers, in light of the shell's morphology and degradation profile. Paclitaxel release from the porous shell was relatively slow due to its extremely hydrophobic nature. It exhibited three phases of release, which corresponded to the degradation profile of the host PDLGA. We found that the effect of the emulsion formulation on the release profile is more significant than the effect of the process kinetics. The copolymer composition had the most dominant effect on the drug release profile from the composite fibers. The polymer content also affected the release profile, whereas the drug content and the organic:aqueous phase ratio resulted in minor effects. Emulsions with a less hydrophobic nature are favorable for effective controlled release of the hydrophobic paclitaxel from the porous shell. © 2007 Elsevier B.V. All rights reserved. Keywords: Paclitaxel; Drug-eluting fibers; Controlled release; Poly(DL-lactic-co-glycolic acid); Degradation 1. Introduction Drug-loaded fibers have a high potential for various biomedical applications. Their advantages include ease of fabrication and a high surface area for controlled release and localized delivery of bioactive agents to their target. Only few controlled release fiber systems based on polymers have been investigated to date [1–8]. The two basic types of drug-loaded fibers that have been reported are monolithic fibers and reservoir fibers. In systems that use monolithic fibers, the drug is dissolved or dispersed throughout the polymer fiber. For example, curcumin, paclitaxel and dexamethasone have been melt spun with poly (L-lactic acid) (PLLA) to generate drug-loaded fibers [1] and aqueous drugs have been solution spun with PLLA [2]. Various steroid-loaded fiber systems have demonstrated expected firstorder release kinetics [3–5]. In systems that use hollow re⁎ Corresponding author. Tel.: +972 3 6405842; fax: + 972 3 6407939. E-mail address: [email protected] (M. Zilberman). 0168-3659/$ - see front matter © 2007 Elsevier B.V. All rights reserved. doi:10.1016/j.jconrel.2007.11.011 servoir fibers, drugs such as dexamethasone and methotrexane have been added to the internal section of the fiber [6–8]. The disadvantages of these systems include poor mechanical properties due to drug incorporation and limitations in drug loading. Furthermore, many drugs and all proteins do not tolerate melt processing and organic solvents. In one of our recent studies we presented a new concept of core/shell fiber structures which successfully meet these challenges [9]. These composite fibers combine a dense polymer core fiber and a drug-loaded porous shell structure, i.e. the drug or protein is located in a separate compartment (a “shell”) around a melt spun “core” fiber. The shell is prepared using mild processing conditions. This can result in good mechanical properties as well as in the desired drug release profile. Our new fibers are ideal for forming thin, delicate, biomedically important structures for various applications, such as fiber-based bioresorbable endovascular stents that mechanically support blood vessels while delivering drugs for preventing restenosis directly to the blood vessel wall, or drug delivery systems for 140 A. Kraitzer et al. / Journal of Controlled Release 126 (2008) 139–148 cancer treatment. The next two paragraphs focus on these two applications. Restenosis is the re-narrowing of a blood vessel which causes a reduction in the diameter of the lumen, consequently restricting blood flow after an intravascular procedure. In-stent restenosis is mainly characterized by an abnormal increase in tissue growth (neointimal hyperplasia) of the tissue composing the blood vessel [10,11]. Re-narrowing is the result of a complex series of biological events in response to the initial injury of the vessel caused by balloon expansion and the presence of the permanent stent implant [12]. Further progress in the treatment of coronary artery disease has been the development of drug-eluting stents that dramatically reduce the incidence of in-stent restenosis to less than 5% [13]. Several drug-coated metal stents have received FDA approval to date. The most popular ones are TAXUS™ (Boston Scientific) — a paclitaxel-eluting stent, and Cypher™ (J&J) — a sirolimus eluting stent. These are metal stents coated with a thin stable dense polymer layer in which the drug is located. Bioresorbable stents are designed to support the vascular wall during the vessel healing process, gradually transferring the mechanical load to the vessel wall while the stent mass and strength decrease over time. Restenosis usually occurs within 3 to 6 months after coronary intervention, and rarely thereafter. Interest in bioresorbable vascular stents, with or without drug delivery, is therefore increasing. These stents are usually made of fibers. For example, Tamai et al. [14,15] described the Igaki/Tamai stent, a bioresorbable balloon expandable zigzag coil design based on a PLLA monofilament. We have developed and studied a fiber-based expandable stent design [16,17], which was prepared using a linear continuous coil array principle, by which four furled lobes convert into a single large lobe upon balloon expansion. This expandable stent design is based on melt-spun bioresorbable fibers that were made from a relatively high molecular weight PLLA. It demonstrated excellent initial radial compression strength and good in vitro degradation resistance for 20 weeks. Cancer may be defined as a disease characterized by uncontrolled proliferation and the spread of abnormal forms of the body's own cells in the body [18]. In cancer therapy, surgical treatment is usually carried out for patients with a resectable carcinoma. However, treatment failure due to local recurrence of primary tumors or metastatic spread often occurs. Surgical adjuvant chemotherapy employing an anticancer agent during or immediately after surgery would therefore be beneficial [18]. A delivery system loaded with paclitaxel at the tumor resection site will provide a high local concentration of the drug, which is detrimental to malignant cells that may have survived surgery, thus preventing tumor re-growth and metastasis. In glioblastoma, localized prolonged release of anti-proliferative drugs, which induces fewer side effects, can be applied to regions where systemic administration is not effective. Drug delivery systems explored for localized paclitaxel delivery to date include microspheres, surgical pastes and implants [18]. An example for a biodegradable implant is the Gliadel® wafer, a biodegradable wafer used to deliver the anticancer drug carmustine directly into a brain tumor site after the surgical removal of the tumor. It has been FDA approved since 1996. Paclitaxel is a potent cell proliferation inhibitor and is known to be very effective in the treatment of cancer [18] as well as in preventing restenosis [18,19]. However, it is potentially cytotoxic, and the paclitaxel dose that can be delivered is relatively small [20,21]. Paclitaxel has been shown to markedly attenuate stent-induced intimal thickening of the lumen [22,23]. Paclitaxel's anti-proliferative effect is reversible [24]. Its short cellular residence time (1 h), along with the reversible anti-proliferative activity, suggest that it should be formulated in sustainedrelease dosage form [25]. The TAXUS trials revealed significant inhibition of coronary stenosis by paclitaxel [26–28]. Drugeluting polymer-coated stents have thus moved into the limelight as vehicles for local drug administration [29,30]. In addition to usage in bioresorbable drug-eluting stents, our novel coating technique can be used for stable stents, where only the drug-loaded coat degrades with time. Studies on paclitaxeleluting bioresorbable microspheres for cancer treatment [31,32] have shown that its release in an aqueous medium is relatively slow due to paclitaxel's high hydrophobicity. Since paclitaxel has demonstrated effectiveness in both drug-eluting stents and local cancer treatment applications, its controlled release in a desired manner is highly important. Highly porous structures that encapsulate the drug, such as our fiber's “shell”, may therefore be advantageous for both applications. The current study focuses on composite core/shell fiber structures loaded with paclitaxel. The porous shell (drug-containing section) was prepared using the technique of freeze drying an inverted emulsion. The effect of the emulsion's composition (formulation) and process kinetics on the emulsion's stability and on the resulting shell's microstructure have already been reported [9]. The current article focuses on the long-term (9 months, relevant for cancer treatment) in vitro release of paclitaxel and its mechanisms. It describes the effects of the emulsion's formulation and process kinetics on the paclitaxel release profile from the fibers, in light of the shell's morphology and degradation profile. It should be noted that these paclitaxel-eluting composite fiber structures can also serve as a good model for composite fibers loaded with other hydrophobic bioactive agents for a wide range of biomedical applications. 2. Materials and methods 2.1. Materials Maxon™ polyglyconate monofilament (3–0) sutures, with a diameter of 0.20–0.25 mm, Syneture, USA were used as core fibers. Bioresorbable porous structures (the shell coating) were made of the following polymers: • 75/25 poly(DL-lactic-co-glycolic acid), inherent viscosity (i.v.) = 0.65 dL/g (in CHCl3 at 30 °C, approximately 97,100 g/mol), Absorbable Polymer Technologies Inc., USA. This polymer is termed 75/25 PDLGA. • 50/50 poly(DL-lactic-co-glycolic acid), inherent viscosity (i.v.) = 0.56 dL/g (in CHCl3 at 30 °C, approximately A. Kraitzer et al. / Journal of Controlled Release 126 (2008) 139–148 80,000 g/mol), Absorbable Polymer Technologies Inc., USA. This polymer is termed 50/50 PDLGA. Drug: Paclitaxel (Genexol™) was purchased from Sam Yang Corp. (Seoul, Korea). 2.1.1. Reagents 1,1,1,3,3,3-Hexafluoro-2-propanol (H1008) was purchased from Spectrum Chemical Mfg. Corp. Chloroform (CHCl3) HPLC grade and methylene chloride (CH2Cl2) HPLC grade were purchased from Frutarom, Israel. Acetonitrile (CH3CN) HPLC grade was purchased from J.T. Baker. 2.2. Preparation of core/shell fiber structures 2.2.1. Fiber surface treatment The sutures were surface-treated in order to enhance the adhesion between the core fiber and the coating. The polyglyconate fibers were slightly stretched on special holders and dipped in 1,1,1,3,3,3-hexafluoro-2-propanol (hexafluorisopropanol) for 40 s. The fibers were then washed with ethanol and dried at room temperature. 2.2.2. Emulsion formation A known amount of 75/25 PDLGA was dissolved in chloroform to form an organic solution and paclitaxel was added to the solution. Double-distilled water was then poured into the organic phase (in a test tube) and homogenization of the emulsion was performed using a homogenizer (Polytron PT3100 Kinematica, 12 mm rotor) operating at 16,500 rpm (medium rate) for 3 min, for most investigated samples. As a reference sample we chose an emulsion formulation containing 17.5% w/v polymer in the organic solution, 1.43% w/w paclitaxel (relative to the polymer load), and an organic to aqueous (O:A) phase ratio of 2:1 v/v. Other formulations included 22.5% w/v polymer, 2.9% and 4.3% w/w paclitaxel, O:A phase ratios of 4:1 and copolymer composition of 50/50 PDLGA. Certain samples were prepared using homogenization rates of 5500 rpm (low rate) or 25,000 rpm (high rate) in order to investigate the effect of processing kinetics on the porous shell structure. 2.2.3. Core/shell fiber structure formation The treated core polyglyconate fibers were dip-coated (while placed on holders) in fresh emulsions and then frozen immediately in a liquid nitrogen bath. The holders + samples were then placed in a pre-cooled (− 105 °C) freeze dryer (Virtis 101 equipped with a nitrogen trap) capable of working with organic solvents (freezing temperature of the condenser was approximately − 105 °C) and freeze dried in order to preserve the microstructure of the emulsion-based core/shell fiber structures. Drying was performed in two stages: 1. The freeze dryer chamber pressure was reduced to 100 mTorr while the temperature remained at − 105 °C. 2. The condenser was turned off and its plate temperature slowly rose to room temperature while the pressure was 141 monitored between 100 mTorr and 700 mTorr. During this step the liquid nitrogen trap condensed the excess water and solvent vapors. The samples were stored in desiccators until use. 2.2.4. Morphological characterization The morphology of the composite core/shell fiber structures (cryogenically fractured surfaces) was observed using a Jeol JSM-6300 scanning electron microscope (SEM) at an accelerating voltage of 5 kV. The SEM samples were Au sputtered prior to observation. The mean pore diameter of the observed morphologies was analyzed using the Sigma Scan Pro software and statistics were drawn using SPSS. Statistical significance was determined using the ANOVA (Tukey–Kramer) method. Statistical significance was determined at p b 0.05. 2.3. In vitro paclitaxel release studies The composite core/shell fiber structures (triplicates) were immersed in phosphate buffered saline (PBS) at 37 °C and pH = 7.4 for 37 weeks in order to determine paclitaxel's release kinetics from these structures. The release studies were conducted in closed glass vessels containing 3 ml PBS medium, using a horizontal bath shaker operated at a constant rate of 130 rpm. The medium was removed (completely) periodically, at certain sampling times, and fresh medium was introduced. This experiment enabled simulating conditions similar to those which exist in a blood vessel. 2.3.1. Extraction procedure Paclitaxel extraction from the medium was performed as follows: the 3 ml medium was completely removed at each time point and placed in a scintillation vial. 3 ml acetonitrile and 1 ml methylene chloride were added. Methylene chloride evaporation was performed under a nitrogen stream and the paclitaxel concentration was then estimated using HPLC. An extraction factor was used for correction. Known weights of paclitaxel were dissolved in 1 ml of methylene chloride and subjected to the same extraction procedure in order to determine the recovery efficiency of the extraction procedure. Recoveries were always greater than 75% and the value of the measured drug was corrected accordingly. The paclitaxel content of the medium samples was determined using Jasco High Performance Liquid Chromatography (HPLC) with a UV 2075 plus detector and a reverse phase column (Zorbax ODS 5 µm, inner diameter d = 4.6 mm, length = 150 mm), and was kept at 25 °C. The mobile phase consisted of a mixture of acetonitrile and double-distilled water (55/45, v/v) at a flow rate of 1 ml/min with a quaternary gradient pump (PU 2089 plus) without gradient. 100 µl samples were injected with an autosampler (AS 2057 Plus). The column effluent was eluted for 15 min and detected at 227 nm. The area of each eluted peak was integrated using the EZstart software version 3.1.7. The cumulative release profiles were determined relative to the initial amount of paclitaxel in the composite fibers (quantity released during the incubation period + the residue remaining in 142 A. Kraitzer et al. / Journal of Controlled Release 126 (2008) 139–148 the fibers). All experiments were performed in triplicates. Results are presented as means ± standard errors. The effects of the emulsion's formulation on the release profile were studied by examining the following parameters: polymer content in the organic phase (%w/v), drug content relative to polymer content (%w/w), organic:aqueous (O:A) phase ratio and copolymer composition. The effect of the process kinetics (homogenization rate) on the release profile was also studied. 2.4. Residual drug recovery from composite fibers Residual paclitaxel recovery from the composite fibers was measured as follows: the fibers were placed in 1 ml methylene chloride and 3 ml of a 50/50 acetonitrile/water solution was added. Methylene chloride evaporation was performed under a nitrogen (99.999%) stream and the paclitaxel concentration was then estimated using HPLC. An extraction factor was used for correction. Five solutions with known concentrations of paclitaxel were subjected to the same extraction procedure in order to determine the recovery efficiency of the extraction procedure. Recoveries were always greater than 75% and the value of the residual drug was corrected accordingly. 2.5. Paclitaxel's chemical stability Two milligrams of paclitaxel were placed in phosphate buffered saline (PBS) at 37 °C for 160 days in order to determine paclitaxel's stability throughout the release experiment. Closed scintillation vials containing 3 ml PBS medium were placed in a horizontal bath shaker operated at a constant rate of 130 rpm. The paclitaxel content of a single vial was measured at each point of time. Paclitaxel was extracted as follows: 3 ml methylene chloride were added to the 3 ml PBS/paclitaxel mixture and stirred for 10 min in order to dissolve the drug. One milliliter was carefully removed from the bottom of the vial (the organic phase) using a pipette and placed in a new vial. Five milliliters of acetonitrile/ double-distilled water (the medium) were added to the vial and then evaporated under nitrogen conditions. The content of each vial was transferred to a test tube and diluted to 20 ml. The paclitaxel content of the medium samples was determined using HPLC, as described above. permeation chromatography (GPC). The GPC (Waters 21515 isocratic pump, operating temperature 40 °C using a column oven) was equipped with a refractive index detector (Waters 2414, operating temperature 40 °C) and calibrated with poly-Llactic acid MW kit standards (Polysciences Inc., USA). Data were analyzed using the Breeze version 3.3 software. The samples were dissolved in methylene chloride, filtered, and eluted through 4 Styragel columns (model WAT044234 HR1 THF, WAT044237 HR2, WAT044225 HR4, WAT054460 HR5, 300 × 7.8 mm, 5 µm particle diameter) at a flow rate of 1 ml/ min. The elution medium was Baker analyzed HPLC grade methylene chloride. 3. Results and discussion The freeze drying technique is unique in being able to preserve the liquid structure in solids. We used this technique in order to produce inverted emulsions in which the continuous phase contained polymer and drug dissolved in a solvent, with water being the dispersed phase. SEM fractographs showing the bulk morphology of the reference specimen are presented in Fig. 1. The diameter of the treated core fiber was in the range of 200–250 µm and a shell thickness of 30–70 µm was obtained for most emulsion formulations. Relatively high contents of hydrophobic components (such as PDLGA and paclitaxel) resulted in an increase in shell thickness, due to the emulsion's 2.6. In vitro degradation study of the porous PDLGA structure Porous 75/25 PDLGA film structures especially prepared for degradation trial were based on the reference emulsion formulation. The inverted emulsion was prepared as described earlier in the paragraph about emulsion formation (in the Materials and methods section describing preparation of core/shell fiber structures), poured into an aluminum plate and freeze dried in liquid nitrogen. Each dried film sample was then incubated in 20 ml phosphate buffered saline (PBS) containing 0.05% (v/v) sodium azide (as preservative) at 37 °C and pH = 7.4 for 17 weeks, under static conditions. Each sample was taken out at weekly intervals and dried using a vacuum oven (35 °C for 1 h), and stored in a dessicator. The weight-average molecular weight and number-average molecular weight of the samples were determined by gel Fig. 1. SEM fractographs showing cross sections of the reference composite fiber. A. Kraitzer et al. / Journal of Controlled Release 126 (2008) 139–148 143 higher viscosity [9]. There are almost no gaps between the core and the shell (Fig. 1b), indicating that the quality of the interface between the fiber and the porous coating is high, i.e. the surface treatment enabled good adhesion between core and shell. The shell's porous structure in all studied specimens based on stable emulsions contained round-shaped pores, usually within the 4– 10 µm range, with a porosity between 67 and 82%. The shell's microstructure was uniform in each sample, probably due to rapid quenching of the emulsion, which enabled preservation of its microstructure [9]. The pores were partially interconnected by smaller inner pores. The emulsions were stable only within a certain formulation range. Only structures that were based on unstable emulsion formulations demonstrated a pore size higher than 10 µm. The effects of emulsion parameters (formulation) and processing conditions on the shell morphology are described in detail in a previous publication [9]. The encapsulation efficiency of all studied samples was in the 45–60% range. The GPC curves of the porous 75/25 PDLGA reference structure at various degradation times are presented in Fig. 2. The curve of the initial structure (time 0) exhibits the expected single peak. As the structure degraded and low molecular weight chains were produced, the peak shifted to the right (higher release time, i.e. smaller molecular weight) and it became broader, indicating a larger molecular weight distribution. The weight-average molecular weight (MW) of the porous structure decreased with degradation time (Fig. 3a), as expected. It is clear that the curve can be divided into two domains: (start– week 10) and (week 10–week 19). The slope of the second domain is double that of the first, indicating that the degradation rate during the second domain is higher than during the first. The cumulative release of paclitaxel from the reference specimen for 37 weeks is presented in Fig. 3(b). Paclitaxel's cumulative release exhibited the following three phases of release: Fig. 2. GPC curves of the 75/25 PDLGA porous structure at various times of immersion in aqueous medium. The time is indicated next to each curve. (a) The first phase of release (phase a) occurred during weeks 1–10, in which the drug was released in an exponential manner, i.e. the rate of release decreased with time. Such a release profile is typical of diffusion-controlled systems. A minor initial burst release (less than 1%) was obtained during the first day of release. Paclitaxel release from the porous shell was relatively slow, mainly due to paclitaxel's extremely hydrophobic nature. Moreover, the release rate decreased with time, since the drug had a progressively longer distance to pass and a lower driving force for diffusion. During this phase of release the degradation of the host polymer resulted in a decrease in MW from 60 kDa to 40 kDa (Fig. 3a). (b) The second phase of release (phase b) occurred during weeks 10–20, in which the drug was released at a constant, relatively high rate. The higher degradation rate of the host polymer in this phase probably resulted in polymer erosion and therefore enabled a faster rate of drug release. During this phase of release the degradation of the host polymer resulted in a decrease in MW from 40 kDa to 2 kDa (Fig. 3a). (c) The third phase of release (phase c) occurred during weeks 21–38, when the porous shell structure was already destroyed due to intensive erosion. In fact, the drug was released from oligomers and short chain polymers of less than 2 kDa. Most of these shell remains are no longer Fig. 3. (a) The weight-average molecular weight of the 75/25 PDLGA reference as a function of degradation time. (b) Cumulative paclitaxel release profile from the reference core/shell fiber specimen. 144 A. Kraitzer et al. / Journal of Controlled Release 126 (2008) 139–148 be specific hydrophobic interactions between the paclitaxel and the polymer. It is clear that the paclitaxel release profile during phases a and b (Fig. 3b) corresponds to the degradation profile of the porous host PDLGA shell (Fig. 3a). Intensive degradation of the host polymer is necessary in order to obtain release of the highly hydrophobic paclitaxel. Although a relatively small percentage of the loaded drug was released, this is the relevant quantity for the stent application [19]. Other investigators working on paclitaxel eluting systems also reported its relatively slow release rate from various polymeric systems [33,34]. The shell's microstructure may affect the drug release profile, which is determined by both thermodynamic and kinetic parameters. The thermodynamic parameters are actually the emulsion's formulation, i.e. the polymer and drug contents, the O:A ratio and the copolymer composition (relative quantities of lactic acid and glycolic acid in PDLGA), whereas the kinetic considerations are actually the processing conditions, which include the rate of homogenization. The effects of these parameters on the paclitaxel's controlled release profile from the fibers are described below (Fig. 4) with reference to the shell's microstructure (Fig. 5) and its degradation profile. 3.1. Effect of polymer content The effect of the polymer content of the organic phase on the drug release from the porous shell is presented in Fig. 4a. In both release phases, a and b, the release rate and quantity from the formulation containing 17.5% w/v polymer were higher Fig. 4. Effect of the emulsion formulation on the release profile of paclitaxel from core/shell fiber structures: (a) effect of polymer content: — 17.5% w/v, — 22.5% w/v, (b) effect of paclitaxel content: — 1.43% w/w, — 2.9% w/w, — 4.3% w/w, (c) effect of O:A phase ratio: — 2:1 v/v, — 4:1, (d) copolymer composition: — 75/25 PDLGA, — 50/50 PDLGA. attached to the core fiber and the core fiber also undergoes erosion. We would expect release of the entire loaded drug during phases a and b. However, in our system the highly hydrophobic paclitaxel is probably attached to the surface of the hydrophobic 75/25 PDLGA's remains even when their molecular weight is extremely low. There may Fig. 5. SEM fractographs of composite fibers showing the effect of the emulsion's formulation on the shell's microstructure: (a) The reference specimen containing 17.5% w/v polymer, 1.43% w/w paclitaxel and phase ratio of 2:1, (b) formulation with 22.5% w/v polymer, (c) formulation with 4.3% w/w paclitaxel, (d) formulation with O:A ratio of 4:1, (e) formulation with copolymer composition of 50/50 PDLGA. A. Kraitzer et al. / Journal of Controlled Release 126 (2008) 139–148 than the release rate and quantity from the formulation containing 22.5% w/v polymer. Since larger drug quantities are released during phase b, the differences between these two formulations are more significant during this phase of release than during phase a. It is suggested that since the pore size and porosity remained almost unchanged with the emulsion's polymer content (Fig. 5a,b and Table 1) but denser “polymeric walls” were probably created between adjacent pores of the formulation with 22.5% w/v polymer, a relatively high polymer content increases the interactions between the matrix and paclitaxel, resulting in a lower diffusion coefficient which results in slower drug release. During the third phase of release, in which the drug was released from shell remains with a very low molecular weight, the polymer content had almost no effect on the rate of drug release, as expected. 3.2. Effect of drug content The effect of the paclitaxel content on its release profile is presented in Fig. 4b. Since the drug content strongly affects the emulsion's stability [9], a relatively low range of drug contents (1.4% w/w–4.3% w/w) was used. The highly hydrophobic paclitaxel diffuses out very slowly from the shell. Therefore, the drug content did not show a significant effect on the release profile during the first phase of release. During the second phase of release the release rate and the amount of released drug decreased slightly with the increase in the drug content from 2.8% w/w to 4.3% w/w (Fig. 4b). We would expect an increase in the release rate with the increase in drug content, due to a higher driving force for diffusion. However, paclitaxel is a hydrophobic drug and a higher paclitaxel content in the organic phase of the emulsion therefore results in a higher interfacial tension (difference between the surface tension of the organic and aqueous phases), leading to a less stable emulsion with a larger pore size (Fig. 5a,c and Table 1). Larger pores are expected to reduce the release rate when the porosity and interconnectivity do not change too much. It can therefore be concluded that in this specific range of drug contents, the morphological changes do not enable the driving force for Table 1 The examined specimens and the structural characteristics of their shells Process parameters Reference Polymer content [% w/v] Paclitaxel content [% w/w] a 22.5 2.86 4.286 4:1 Mean pore size ± SD [µm] Mean porosity ± SD [%] 6.42 ± 2.32 5.34 ± 1.64 ( b) 9.22 ± 4.54 ( b) 29.96 ± 3.1 ( b) 5.96 ± 2.41 ( b) 69 ± 6 72 ± 8 73 ± 3 82 ± 9 80 ± 2 Organic to aqueous phase ratio [v/v] Homogenization rate [rpm] 5500 8.23 ± 3.15 ( b) 77 ± 8 25,000 5.98 ± 1.6 (P = 0.053) 75 ± 10 PDLGA copolymer 50/50 4.1 ± 1.35 ( b) 67 ± 6 composition [w/w] a The reference sample was prepared using the following conditions: emulsion-based on 75/25 PDLGA, 17.5% w/v polymer, 1.43% w/w paclitaxel, O:A = 2:1 v/v, homogenization rate = 16,500 rpm. b Significant compared to the reference. 145 diffusion to affect paclitaxel's release profile. During the third phase of release (20–38 weeks) the release rate from the remaining short polymers and oligomers of the formulations with 2.9% w/w and 4.3% w/w paclitaxel is significantly higher than that obtained from the formulation with 1.4% w/w paclitaxel (Fig. 5a). The driving force for diffusion plays a major role at this stage, after intensive polymer erosion when the morphological features of the initial microstructure no longer exist. 3.3. Effect of O:A phase ratio The effect of the O:A phase ratio on paclitaxel's release profile from the composite fibers and on the shell's microstructure are presented in Figs. 4c and 5a,d, respectively. The release profile during release phases a and b (20 weeks) as well as the pore size (Table 1) exhibited almost no change in the O:A range of 2:1 to 4:1. It should be mentioned that the relatively narrow O:A range chosen for this study resulted from the emulsion's stability considerations. The porosity of samples derived from emulsions with O:A ratios higher than 4:1 may not be high enough to enable effective release of water-insoluble agents such as paclitaxel. On the other hand, samples derived from emulsions with O:A ratios less than 2:1 are not stable. During the third phase of release (20–40 weeks) the release rate from the 4:1 phase ratio was higher than from the 2:1 phase ratio. A relatively high organic phase content provides more binding sites for the hydrophobic paclitaxel. This higher drug content enables a higher release rate only when the drug diffuses out from very low molecular weight components which remain in the third phase of release. 3.4. Effect of copolymer composition The effect of the copolymer composition, i.e. the relative quantities of lactic acid (LA) and glycolic acid (GA) in the copolymer, on the drug release profile and on the shell's microstructure is presented in Figs. 4d and 5a,e, respectively. The rate of release from the 50/50 PDLGA formulation is higher than that obtained from the 75/25 PDLGA formulation (reference) during phases a and b (Fig. 4d). It is important to note that the differences in the release rate and quantity are low during the first phase of release but very high during the second phase of release. After 20 weeks of degradation the 50/50 formulation released 70% of the drug, whereas the 75/25 formulation released only 13%. These differences are attributed mainly to differences in the degradation rate of these two copolymers and differences in their hydrophilic/hydrophobic nature. The 50/50 copolymer degrades faster than the 75/25 copolymer and therefore during intensive erosion (phase b) it releases the drug at a faster rate. Furthermore, the less hydrophobic nature of the 50/50 copolymer relative to the 75/25 copolymer results in less drug attachment to its surface and therefore also contributes to a higher paclitaxel release rate. The mean pore diameter increased with the increase in the copolymer's LA content. The 50/50 composition exhibited a mean pore diameter of 4.1 µm, whereas the 75/25 composition (reference) exhibited a mean pore diameter of 6.4 µm (Table 1). 146 A. Kraitzer et al. / Journal of Controlled Release 126 (2008) 139–148 An increase in the copolymer's LA content actually increases the surface tension, prompting the water droplets to flocculate and coalescence. Therefore, increasing the mean pore diameter affects the emulsion in the same manner as addition of paclitaxel. The smaller pore size of the 50/50 PDLGA relative to the 75/25 PDLGA enables a higher surface area for diffusion. Since the pores are partially interconnected by smaller inner pores and the shell structure is highly porous, the smaller pore size also contributes to the higher rate of paclitaxel release during phases a and b. It can be concluded that a higher glycolic acid content in the copolymer, i.e. a less hydrophobic copolymer, enables higher paclitaxel release from the fibers due to a combination of 3 phenomena: higher degradation rate of the host polymer, less drug attachment to its surface and finer porous microstructure. The degradation rates achieved during the second phase of release in our study are actually higher than those reported in other studies on paclitaxel release from bioresorbable polymers. 3.5. Effect of process kinetics The effects of the emulsion's homogenization rate (prepared during a 180 s homogenization) on the drug release from the porous shell and on the microstructure are presented in Fig. 6. The homogenization rate had practically no effect on the release profile during the first phase of release (10 weeks), but had some effect on the release profile during the second phase of release (Fig. 6a) due to small changes in the shell's porous structure (Fig. 6b,c and Table 1). An increase in homogenization rate from 5500 rpm to 25,000 rpm resulted in a slight decrease in mean pore size from 8.2 µm to 6.0 µm with almost no change Fig. 6. (a) The effect of the stirring rate on the release profile of paclitaxel from core/shell fiber structures: — low rate, — high rate, (b) SEM fractograph of a fiber prepared using the low stirring rate (5500 rpm), (c) SEM fractograph of a fiber prepared using the high stirring rate (25,000 rpm). Fig. 7. A schematic representation of the qualitative model describing the dependence of the drug release profile on the emulsion's formulation and process kinetics. in the porosity. The higher surface area for diffusion enabled some increase in drug release rate and quantity. In conclusion, a qualitative model describing the process → structure → property effects in our system is presented in Fig. 7. Diffusion of the drug molecules is controlled chemically, by the emulsion formulation and also geometrically, through the surface area. The emulsion formulation directly influences the diffusion by producing binding regions for the drug as more hydrophobic materials are introduced into the emulsion, thus delaying the drug molecules. The emulsion's formulation also affects its stability during processing, and as a result determines the freeze dried microstructure. The microstructure determines the surface area available for diffusion, which affects the drug release rate. In general, a high diffusion rate is achieved when high porosity is combined with small pore size. In our system, the process kinetics (rate of homogenization) showed a considerably smaller effect on the microstructure and on the paclitaxel release profile. It should be mentioned that degradation of the host polymer also affects the diffusion rate, as in other bioresorbable drug delivery systems. Finally, since long-term drug release was examined in this study, the chemical stability of paclitaxel was measured, as described in the experimental section. An example of an HPLC run is presented in Fig. 8a. Two peaks are shown: a major peak Fig. 8. (a) HPLC run showing the peaks of paclitaxel and its derivative, (b) the derivative percentage as a function of immersion time in the aqueous medium. A. Kraitzer et al. / Journal of Controlled Release 126 (2008) 139–148 of paclitaxel after an elution time of 4–5 min, and a minor peak of its derivative after an elution time of 7 min. The derivative percentage (derivative content divided by paclitaxel content) as a function of immersion time in the aqueous medium is presented in Fig. 8b. As expected, the derivative percentage increases with time, but even after 23 weeks it is lower than 5%, thus demonstrating that 95% of the paclitaxel remained stable. 4. Summary and conclusions Bioresorbable core/shell fiber structures for biomedical applications were developed and studied. These structures were composed of a polyglyconate core and a porous PDLGA shell loaded with the anti-proliferative agent paclitaxel, prepared using freeze drying of inverted emulsions. A long-term in vitro release study was performed. The investigation of these new composite fibers focused on the effects of the emulsion's composition (formulation) and process kinetics on the drug release profile from the fibers, in light of the shell's morphology and degradation profile. These unique fiber structures can be used as basic elements of vascular stents and also for local cancer treatment. In general, porous “shell” structures (porosity of 67–82% and pore size of 4–10 µm) were obtained with good adhesion to the core fiber. Paclitaxel release from the porous shell was relatively slow due to its extremely hydrophobic nature. It exhibited three phases of release. It is clear that the first phase (1–10 weeks) was governed by diffusion, whereas the second phase (10–20 weeks) was governed by degradation. The release profile of paclitaxel from the porous shell corresponds to the degradation profile of the host 75/25 PDLGA. The copolymer composition had the most dominant effect on the drug release profile from the composite fibers. An increase in the glycolic acid content (or decrease in lactic acid content) resulted in a tremendous increase in the release rate during the second phase, which was attributed mainly to the increased degradation rate and decreased drug attachment to the host polymer. A decrease in polymer content also resulted in an increase in the release rate during the second phase of release, whereas the drug content and the O:A phase ratio in the studied range affected the release profile only during the third phase of release. The effect of the emulsion formulation on the release profile is more significant than the effect of the process kinetics. Furthermore, emulsions with a less hydrophobic nature are favorable for effective controlled release of the hydrophobic paclitaxel from the porous shell, since they do not provide many binding regions for the drug and their higher stability enables obtaining highly porous shell structures with a large surface area for diffusion after freeze drying. Acknowledgements The authors are grateful to the RAMOT (Horowitz) Foundation and to the Slezak Foundation, Tel-Aviv University, for supporting this research. 147 References [1] S.H. Su, C.L. Landau, R.Y. Chao, R.B. Timmons, R.S. Meidell, L. Tang, R.C. Eberhart, Expandable bioresorbable endovascular stent with anti-platelet and anti-inflammation treatments, Circulation 104 (II) (2001) 500–507. [2] N. Alikacem, T. Yoshizawa, C. Wilson, K.D. Nelson, Quantitative MR Imaging study of intravitreal sustained release of VEGF in rabbits, Invest. Ophthalmol. Vis. Sci. 41 (2000) 1561–1569. [3] R.L. Dunn, D.H. Lewis, J.M. Goodson, Monolithic fibers for controlled delivery of tetracycline, Proc. Int. Symp. Control. Rel. Bioact. Mater. 9 (1982) 157–163. [4] R.L. Dunn, J.P. English, W.C. Stoner, A.G. Potter, B.H. Perkins, Biodegradable fibers for the controlled release of tetracycline in treatment of peridontal disease, Proc. Int. Symp. Control. Rel. Bioact. Mater. 14 (1987) 289–294. [5] R.L. Dunn, D.H. Lewis, L.R. Beck, Fibrous polymer for the delivery of contraceptive steroids to the female reproductive track, in: D.H. Lewis (Ed.), Controlled Release of Pesticides and Pharmaceuticals, Plenum Press, New York, 1981, pp. 125–146. [6] M.D.J. Eenink, J. Feijen, J. Oligslanger, J.H.M. Albers, J.C. Rieke, P.J. Greidonus, Biodegradable hollow fibers for the controlled release of hormones, J. Control. Rel. 6 (1987) 225–237. [7] G. Polacco, M.G. Cascone, L. Lazzeri, S. Ferrara, P. Giusti, Biodegradable hollow fibers containing drug-loaded nanoparticles as controlled release systems, Polym. Int. 51 (12) (2002) 1464–1472. [8] L. Lazzeri, M.G. Cascone, S. Quiriconi, L. Morabito, P. Giusti, Biodegradable hollow microfibers to produce bioactive scaffolds, Polym. Int. 54 (2005) 101–107. [9] A. Kraitzer, M. Zilberman, Paclitaxel-loaded composite fibers: microstructure and emulsion stability, J. Biomed. Mater. Res. A. 81 (2) (2007) 427–436. [10] M.N. Babapulle, M.J. Eisenberg, Coated stents for prevention of restenosis: part I, Circulation 106 (2002) 2734–2740. [11] S.H. Duda, T.C. Poerner, B. Wiesinger, J.H. Rundback, G. Tepe, J. Wiskirchen, K.K. Haase, Drug-eluting stents: potential applications for peripheral occlusive disease, J. Vasc. Interv. Radiol. 14 (2003) 291–301. [12] A.L. Lewis, L.A. Tolhurst, P.W. Stratford, Analysis of a phosphorylcholine-based polymer coating on a coronary stent pre- and post-implantation, Biomaterials 23 (2002) 1697–1706. [13] T.C. Woods, A.R. Marks, Drug-eluting stents, Ann. Rev. Med. 55 (2004) 169–178. [14] H. Tamai, K. Igaki, E. Kyo, K. Kosuga, A. Kawashima, S. Matsui, H. Komori, T. Tsuji, S. Motohara, H. Uehata, Initial and 6-month results of biodegradable poly-L-lactic acid coronary stents in humans, Circulation 102 (2000) 399–404. [15] H. Tamai, K. Igaki, T. Tsuji, E. Kyo, K. Kosuga, A. Kawashima, S. Matsui, H. Komori, S. Motohara, H. Uehata, E. Takeuchi, A biodegradable poly-Llactic acid coronary stent in porcine coronary artery, J. Interv. Cardiol. 12 (1999) 443–449. [16] M. Zilberman, N.D. Schwade, R.C. Eberhart, Protein-loaded bioresorbable fibers and expandable stents: mechanical properties and protein release, J. Biomed. Mater. Res. B. 69 (2004) 1–10. [17] M. Zilberman, R.C. Eberhart, Drug-eluting bioresorbable stents for various applications, Ann. Rev. Biomed. Eng. 8 (2006) 153–180. [18] A.B. Dhanikula, R. Panchagnula, Localized paclitaxel delivery, Int. J. Pharm. 183 (2) (2000) 85–100. [19] S. Silber, E. Grube, The Boston scientific antiproliferative paclitaxel eluting stent (TAXUS), in: P.W. Serruys (Ed.), Handbook of Coronary Stents, Martin Dunitz, London, 2001, pp. 311–319. [20] AHFS Drug Information, American Society of Health System Pharmacists, Bethseda, 1989, pp. 1075–1086. [21] E.K. Rowinsky, R.C. Donehower, Drug therapy: paclitaxel (Taxol), N. Engl. J. Med. 332 (1995) 1002–1014. [22] T. Yamawaki, H. Shimokawa, T. Kozai, K. Miyata, T. Higo, E. Tanaka, K. Egashira, T. Shiraishi, H. Tamai, K. Igaki, Intramural delivery of a specific tyrosine kinase inhibitor with biodegradable stent suppresses the restenotic changes of the coronary artery in pigs in vivo, J. Am. Coll. Cardiol. 32 (1998) 780–786. 148 A. Kraitzer et al. / Journal of Controlled Release 126 (2008) 139–148 [23] D.E. Drachman, E.R. Edelman, P. Seifert, A.R. Groothuis, D.A. Bornstein, K.R. Kamath, M. Palasis, D. Yang, S.H. Nott, C. Rogers, Neointimal thickening after stent delivery of paclitaxel: change in composition and arrest of growth over six months, J. Am. Coll. Cardiol. 36 (2000) 2325–2332. [24] H. Suh, B. Jeong, R. Rathi, S.W. Kim, Regulation of smooth muscle cell proliferation using paclitaxel-loaded poly(ethylene oxide)-poly(lactide/ glycolide) nanospheres, J. Biomed. Mater. Res. 42 (1998) 331–338. [25] F. Alexis, S.S. Venkatraman, S.K. Rath, F. Boey, In vitro study of release mechanisms of paclitaxel and rapamycin from drug-incorporated biodegradable stent matrices, J. Cont. Rel. 98 (2004) 67–74. [26] E. Grube, S. Silber, K.E. Hauptmann, R. Mueller, L. Buellesfeld, U. Gerckens, M.E. Russel, TAXUS I: six- and twelve-month results from a randomized, double-blind trial on a slow-release paclitaxel-eluting stent for de novo coronary lesions, Circulation 107 (2003) 38–42. [27] K. Tanabe, P.W. Serruys, M. Degertekin, G. Guagliumi, E. Grube, C. Chan, T. Munzel, J. Belardi, W. Ruzyllo, L. Bilodeau, H. Kelbaek, J. Ormiston, K. Dawkins, L. Roy, B.H. Strauss, C. Disco, J. Koglin, M.E. Russell, A. Colombo, Chronic arterial responses to polymer-controlled paclitaxel-eluting stents: comparison with bare metal stents by serial intravascular ultrasound analysis: data from the randomized TAXUS-II trial, Circulation 109 (2004) 196–200. [28] K. Tanabe, P.W. Serruys, E. Grube, P.C. Smits, G. Selbach, W.J. van der Giessen, M. Staberock, P. de Feyter, R. Müller, E. Regar, M. Degertekin, J.M.R. Ligthart, C. Disco, B. Backx, M.E. Russell, TAXUS III trial: in- [29] [30] [31] [32] [33] [34] stent restenosis treated with stent-based delivery of paclitaxel incorporated in slow-release polymer formulation, Circulation 107 (2003) 559–564. G.W. Stone, S.G. Ellis, D.A. Cox, J. Hermiller, C. O'Shaughnessy, J.T. Mann, M. Turco, R. Caputo, P. Bergin, J. Greenberg, J.J. Popma, M.E. Russell, A polymer-based, paclitaxel-eluting stent in patients with coronary artery disease, N. Engl. J. Med. 350 (2004) 221–231. T. Tsuji, H. Tamai, K. Igaki, E. Kyo, K. Kosuga, T. Hata, T. Nakamura, S. Fujita, S. Takeda, S. Motohara, H. Uehata, Biodegradable stents as a platform to drug loading, Int. J. Cardiovasc, Interv. 5 (2003) 13–16. L. Mu, S.S. Feng, A novel controlled release formulation for the anticancer drug Paclitaxel (Taxol): PLGA nanoparticles containing vitamin E TPGS, J. Cont. Rel. 86 (2003) 33–48. T.L. Richard, H.L. Burt, Paclitaxel loaded poly (L-lactic acid) (PLLA) microspheres II. The effect of processing parameters on microsphere morphology and drug release kinetics, Int. J. Pharm. 281 (2004) 103–106. D. Chitkara, A. Shikanov, N. Kumar, A.J. Domb, Biodegradable injectable in situ depot-forming drug delivery systems, Macromol. Biosci. 6 (2006) 977–990. A. Shikanov, B. Vaisman, M.Y. Krasko, A. Nyska, A.J. Domb, Poly (sebatic acid-co-ricinoleic acid) biodegradable carrier for paclitaxel: invitro release and in-vivo toxicity, J. Biomed. Mater. Res. A. 69 (1) (2004) 47–54.