* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Motor pathways - autonomic Nervous system
Survey
Document related concepts
Transcript
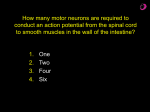
Motor (efferent) system Divided into: Somatic motor division that controls skeletal muscle Visceral/autonomic – controls smooth and cardiac muscles and the glands (exocrine and endocrine) These 2 system differ not only in the effector but also in their descending pathway and the response Copyright © 2010 Pearson Education, Inc. ANS Versus Somatic Nervous System (SNS) The ANS differs from the SNS in the following three areas 1. Effectors The effectors of the SNS are skeletal muscles The effectors of the ANS are cardiac muscle, smooth muscle, and glands Copyright © 2010 Pearson Education, Inc. ANS Versus Somatic Nervous System (SNS) 2. Efferent pathways In the SNS heavily myelinated axons of the somatic motor neurons extend from the CNS to the effector (one neuron) Efferent pathways in the ANS are a two-neuron chain The preganglionic (first) neuron has a lightly myelinated axon The post-ganglionic (second) neuron extends to an effector organ Pre-ganglionic Post-ganglionic Ganglion Copyright © 2010 Pearson Education, Inc. ANS Versus Somatic Nervous System (SNS) 3. Target organ responses All somatic motor neurons release Acetylcholine (ACh), which has an excitatory effect In the ANS: Preganglionic fibers release ACh Postganglionic fibers release norepinephrine or ACh and the effect is either stimulatory or inhibitory ANS effect on the target organ is dependent upon the neurotransmitter released and the receptor type of the effector Copyright © 2010 Pearson Education, Inc. Characteristic Somatic Nervous System Autonomic Nervous System Voluntary (skeletal) muscle Smooth muscle, Cardiac Muscle, Glands Adjustment to external environment. Adjustment within the internal environment (homeostasis) Number of neurons from CNS to effectors 1 2 Ganglia outside the CNS 0 Chain ganglia, collateral ganglia or terminal ganglia Acetylcholine Acetylcholine, adrenaline, noradrenalin Effectors General function Neurotransmitter On NMJ - nicotinic receptors – ACh always excitatory Copyright © 2010 Pearson Education, Inc. Receptors for neurotransmitters in the motor division Receptors are divided into 2 groups: Cholinergic – receive and respond to acetylcholine (ACh): Two subgroups that are names of chemicals that mimic some of the actions of Ach: Muscarinic (chemical found in the mushroom Amanita muscarina) Nicotinic (chemical found in the tobacco plant – nicotina tabacum) Adrenergic – receive and respond to norepinephrin (NE) / epinephrine (E) Divided into alpha and beta Copyright © 2010 Pearson Education, Inc. Cholinergic Nicotinic Receptors location Motor end plates of skeletal muscle cells (will be discussed later) All ganglionic neurons (sympathetic and parasympathetic) Hormone-producing cells of the adrenal medulla Effect of ACh at nicotinic receptors is always direct and stimulatory Copyright © 2010 Pearson Education, Inc. Cholinergic Muscarinic Receptors location All effector cells stimulated by postganglionic cholinergic fibers The effect of ACh at muscarinic receptors Can be either inhibitory or excitatory Depends on the receptor type of the target organ Copyright © 2010 Pearson Education, Inc. ACh (cholinergic) receptors Nicotinic receptors (nACh) Pre-ganglionic Direct mechanism – open Na+ channels (depolarization) Fast excitatory effect Muscarinic receptors (mACh) Post-ganglionic Indirect mechanism – use of G-protein and 2nd messenger system Increase intracellular Ca2+ release Slow excitatory M1, M3, M5 Copyright © 2010 Pearson Education, Inc. Inhibition of adenylate cyclase Slow inhibitory M2, M4 Adrenergic Receptors Two types Alpha () (subtypes 1, 2) – excited Beta () (subtypes 1, 2 , 3) Effects of NT depend on which subclass of receptor predominates on the target organ Norepinephrine excites mainly Alpha () receptors Epinephrine excites both alpha and beta equally Copyright © 2010 Pearson Education, Inc. NE (adrenergic) receptors - all indirect through G-protein 1 2 Increase intracellular Ca2+ release Inhibition of adenylate cyclase Slow excitation Slow inhibition Copyright © 2010 Pearson Education, Inc. 1 3 2 2nd messenger – cAMP Inhibition or activation of adenylate cyclase slow excitation Slow inhibition Lypolysis (excitation) Divisions of the ANS Enteric nervous system Copyright © 2010 Pearson Education, Inc. http://www.sirinet.net/~jgjohnso/nervous.html Autonomic Nervous System (ANS) function The ANS major function is to maintain homeostasis The ANS : functions via visceral (subconscious) reflexes The autonomic system is coordinated primarily by the hypothalamus and the medulla (higher centers) The brain stem and the spinal cord seem to have direct influence over autonomic functions Copyright © 2010 Pearson Education, Inc. Autonomic reflexes Autonomic reflexes are mediated by neural circuits in the spinal cord and brain stem The afferent pathways include both visceral and somatic fibers The reflex includes interneurons that receive convergent input from visceral and somatic fibers Efferent pathway parasympathetic can be sympathetic or Main difference: visceral reflex arc has two neurons in the motor pathway Copyright © 2010 Pearson Education, Inc. Copyright © 2010 Pearson Education, Inc. Copyright © 2010 Pearson Education, Inc. The 2 divisions of the ANS exit the spinal cord in different regions There are 2 anatomical differences between the 2 branches: The point of origin in the CNS Location of autonomic ganglia Copyright © 2010 Pearson Education, Inc. Anatomy of ANS Division Origin of Fibers Length of Fibers Location of Ganglia Sympathetic Thoraco -lumbar region of the spinal cord Short pre - ganglionic and long post ganglionic Close to the spinal cord Parasympathetic Brain and sacral spinal cord Long preganglionic and short postganglionic In the visceral effector organs Copyright © 2010 Pearson Education, Inc. Copyright © 2010 Pearson Education, Inc. The functions of the parasympathetic division It is also called the anabolic division The functions center on Relaxation Food processing Energy absorption Copyright © 2010 Pearson Education, Inc. The major effects of the parasympathetic division Constriction of pupils Increase secretion of salivary, gastric, duodenal and intestinal glands, pancreas (both exocrine and endocrine) and liver Increase of digestive system movement (smooth muscle) Stimulation of defecation Contraction of urinary bladder Constriction of respiratory passageways Reduction of heart rate and force of contraction Copyright © 2010 Pearson Education, Inc. Para sympathetic functions Copyright © 2010 Pearson Education, Inc. http://users.rcn.com/jkimball.ma.ultranet/BiologyPages/P/PNS.html Parasympathetic Division Outflow Cranial Outflow Sacral Outflow Cranial Nerve Ganglion Effector Organ(s) Effect on effector Occulomotor (III) Ciliary Eye (iris) Constrict pupil Facial (VII) Pterygopalatin Submandibular Salivary, nasal, Increase secretion and lacrimal glands Glossopharyngeal (IX) Otic Parotid salivary Increase secretion glands Vagus (X) Located within the walls of target organs Heart, lungs, and most visceral organs Decrease HR, constrict bronchioles S2-S4 Located within the walls of the target organs Large intestine, urinary bladder, ureters, and reproductive organs Increase motility and secretion of the GI tract, release of urine, erection Copyright © 2010 Pearson Education, Inc. Copyright © 2010 Pearson Education, Inc. Cranial Outflow Sacral Outflow Copyright © 2010 Pearson Education, Inc. Figure 14.4 Parasympathetic pre and post-ganglionic receptors (nACh) (mACh) (nACh) (mACh) Copyright © The McGraw-Hill Companies, Inc Copyright © 2010 Pearson Education, Inc. Break down of ACh The effect of ACh is short-lived Inactivated in the synapse by the enzyme acetylcholinesterase (AChE) Inactivated in cholinesterase the surrounding tissues The effect of the parasympathetic division is localized and lasts about 20 msec. Copyright © 2010 Pearson Education, Inc. Copyright © 2010 Pearson Education, Inc. Parasympathetic drugs Modes of action: direct agonistic action on the receptor (pilocarpine and methacholine) Indirect agonists work by inactivation of acetylcholinesterase (enzyme that breaks down acetylcholine), resulting in accumulation of acetylcholine in synaptic cleft antagonist drugs (for example atropine) block the muscarinic receptors and thus block the action of Ach Copyright © 2010 Pearson Education, Inc. Drugs affecting the parasympathetic nervous system Nicotinic receptors: Agonists at muscles will cause contraction Antagonists at muscles will cause paralysis. Muscarinic receptors: Agonists will cause increased bowel and bladder function, decreased HR, bronchoconstriction, and miosis. Antagonists will cause constipation, urinary retention, increased heart rate, bronchodilation, and dilated pupils Copyright © 2010 Pearson Education, Inc. Sympathetic division functions Involves E activities – exercise, emergency, and embarrassment excitement, Increases mental alertness Increases metabolic rate Activates energy reserves Increase respiratory rates and dilate respiratory passageways Increase heart rate and blood pressure Activate sweat glands Copyright © 2010 Pearson Education, Inc. Copyright © 2010 Pearson Education, Inc. http://users.rcn.com/jkimball.ma.ultranet/BiologyPages/P/PNS.html Sympathetic division anatomy The preganglionic cell bodies are located in the lateral horn of segments T1 and L2 (thoracolumbar outflow). Ganglionic neurons cell bodies are in 3 locations: Paired Chain ganglia on both sides of the spinal cord All preganglionic fibers go through the chain ganglia. Unpaired Collateral/prevertebral ganglia found anterior to the vertebral column Adrenal medulla – modified sympathetic ganglion that release NT into the blood Copyright © 2010 Pearson Education, Inc. Copyright © 2010 Pearson Education, Inc. Organization of the sympathetic division After passing through the intervertebral foramen the ventral ramus gives rise to a myelinated white ramus The white ramus carries the preganglionic axons to a sympathetic chain ganglion The preganglionic fibers diverge extensively and can synapse on several ganglionic neurons Sympathetic Trunks and Pathways A preganglionic fiber follows one of three pathways upon entering the paravertebral ganglia 1. Synapse with the ganglionic neuron within the same ganglion 2. Ascend or descend the sympathetic chain to synapse in another chain ganglion 3. Pass through the chain ganglion and emerge without synapsing Copyright © 2010 Pearson Education, Inc. Figure 14.6 Chain ganglia 2 possible pathways in both the synapse can be either on the same segment or in a different one (pathways 1 or 2) postganglionic unmyelinated fibers return via gray ramus to the spinal nerve (about 8% of each spinal nerve fibers are sympathetic postganglionic) postganglionic fibers innervate structures in the body wall, head, neck and limbs (sweat glands, superficial blood vessels, arrector pilli muscle, skin) postganglionic unmyelinated fibers do not return but create sympathetic nerves Those innervate structures in the thoracic cavity Copyright © 2010 Pearson Education, Inc. 2 1 Collateral ganglia Postganglionic fibers that follow the third pathway synapse in the collteral/prevertebral ganglia Those ganglia are not paired and they are found only in the abdominal and pelvic regions They are close to the spinal cord As a result the postganglionic fibers are longer than the preganglionic one Copyright © 2010 Pearson Education, Inc. 1&2 3 Copyright © 2010 Pearson Education, Inc. Figure 14.5 Pathways with Synapses in the Adrenal Medulla Some preganglionic fibers pass directly to the adrenal medulla without synapsing Upon stimulation, medullary cells secrete norepinephrine and epinephrine into the blood Copyright © 2010 Pearson Education, Inc. Copyright © 2010 Pearson Education, Inc. Sympathetic pre and post-ganglionic receptors (nACh) (nACh) Copyright © The McGraw-Hill Companies, Inc Copyright © 2010 Pearson Education, Inc. Copyright © 2010 Pearson Education, Inc. Recept Found in or Sensitivity Effect 1 Most sympathetic NE>E target tissue Smooth muscle contraction 2 Digestive system and pancreas NE>E Smooth muscle contraction 1 Heart muscle, kidney NE=E Heart muscle contraction 2 Smooth muscle of E>NE some organs Smooth muscle relaxation 3 Adipose tissue lipolysis Copyright © 2010 Pearson Education, Inc. NE>E Unique Roles of the Sympathetic Division only sympathetic fibers are found on: The adrenal medulla, sweat glands, arrector pili muscles, kidneys, and most blood vessels The sympathetic division controls Thermoregulatory responses to heat Release of renin from the kidneys and increased blood pressure Metabolic effects Increases metabolic rates of cells Raises blood glucose levels Mobilizes fats for use as fuels Copyright © 2010 Pearson Education, Inc. Drugs that act on the sympathetic division Agonists can work in 2 ways: Direct -mimic E, NE function on receptors Indirect – cause release of NE from storage vesicles Antagonists can: Prevent synthesis and storage of NE Block release of NE Block receptors Copyright © 2010 Pearson Education, Inc. Example of Drugs affecting the sympathetic nervous system • Alpha 1 receptors – • agonists will raise BP, • antagonists will lower BP • Beta 1 receptors – • agonists will increase heart rate and strength of contraction, • antagonists will decrease heart rate and BP • Beta 2 receptors – • agonists will increase respiratory airflow, will increase blood flow to skeletal muscles (via blood vessels dilation) • antagonists will constrict respiratory flow Copyright © 2010 Pearson Education, Inc. Interactions of the Autonomic Divisions Most visceral organs have dual innervation Dynamic antagonism allows for precise control of visceral activity Sympathetic tone (vasomotor tone) Keeps the blood vessels in a continual state of partial constriction Parasympathetic division normally dominates the heart and smooth muscle of digestive and urinary tract organs Slows the heart Dictates normal activity levels of the digestive and urinary tracts The sympathetic division can override these effects during times of stress Copyright © 2010 Pearson Education, Inc. More ANS neurotransmitters Transmitter Functions nitric oxide (NO) parasympathetic - important in erection and in gastric emptying. Activates guanylate cyclase. vasoactive intestinal polypeptide (VIP) parasympathetic - co-release with ACh affects salivation; also in sympathetic cholinergic fibres. May be important throughout the gastrointestinal tract. adenosine triphosphate (ATP) sympathetic - blood vessels and vas deferens. Co-released with catecholamines. neuropeptide Y (NPY) sympathetic - facilitates effect of noradrenaline (co-released). Causes prolonged vasoconstriction. serotonin (5HT) important in enteric neurones (peristalsis) gamma-amino butyric acid (GABA) enteric. dopamine May mediate vasodilatation in the kidney gonadotropin releasing hormone (GnRH) co-transmitter with ACh in sympathetic ganglia. Substance P sympathetic ganglia, enteric neurones calcitonin gene related peptide (CGRP) contributes to neurogenic inflammation Copyright © 2010 Pearson Education, Inc. NT-receptor interaction - heart 2 Sympathetic presynaptic nerve terminal M2 NE + 1 2 + + ACh - parasympathetic nerve terminal Copyright © 2010 Pearson Education, Inc. M2 1 + 2 -